No products in the cart.
Lamolep, tablets 100 mg 30 pcs
€56.98 €47.49
Description
A anticonvulsant (antiepileptic) drug. Stabilizes potential-dependent sodium channels of cell membranes. It also blocks release of neurotransmitters, mainly glutamic amino acid (which plays key role in development of epileptic seizures).
Pharmacokinetics
Absorption
After oral administration it is quickly and completely absorbed from the intestine, significantly not subject to the “first pass” effect. Cmax is reached 2.5 h after oral administration. Food intake slows down the absorption process, but does not affect its effectiveness. Bioavailability is 98%. Pharmacokinetics of the drug after a single dose not exceeding 450 mg is linear. The concentration in equilibrium is sharply pronounced individual character.
Distribution
Protein binding is 55%. It is unlikely that displacement of lamotrigine from protein binding can cause toxic effects. Vd is 0.92-1.22 l/kg body weight. It is excreted with breast milk. The concentration in breast milk is 40-60% of the plasma concentration. In some cases, the drug concentration in the serum of infants whose mothers took the drug while breastfeeding reaches therapeutic levels.
Metabolism
The drug is biotransformed in the liver under the action of uridine diphosphate glucuronyl transferase. Among the metabolites, N -glucuronides predominate. Lamotrigine moderately and dose-dependently induces its own metabolism.
The mean equilibrium clearance in healthy adults is 39±14 mL/min. It is excreted with urine as glucuronide conjugate, less than 10% – unchanged, about 2% (unchanged and as metabolites) – in faeces. Clearance and T1/2 are independent of dose.T1/2 of healthy volunteers is 24-35 h.
Pharmacokinetics in Special Clinical Cases
Clearance, calculated per kg body weight, is higher in children than in adults and is highest before the age of 5 years. T1/2 in children is usually shorter than in adults.
The T1/2 in children when concomitantly used with enzyme inducers is 7 h, with sodium valproate 45-60 h.
Lamotrigine clearance in elderly and younger patients is minimally different.
Indications
Indications
Epilepsy
for adults and children over 12 years old
as monotherapy or in combination with other antiepileptic drugs for the treatment of partial and generalized seizures (including tonic-clonic seizures and convulsive seizures in Lennox-Gastaut syndrome);
for children from 2 to 12 years old
as part of combination therapy for the treatment of partial and generalized seizures (including tonic-clonic seizures and convulsive seizures in Lennox-Gastaut syndrome).
Bipolar disorders
for adults (18 years and older)
for the prevention and treatment, mainly of episodes of depression.
Pharmacological effect
Pharmacological effect
Anticonvulsant (antiepileptic) drug. Stabilizes voltage-dependent sodium channels of cell membranes. It also blocks the release of neurotransmitters, mainly glutamine amino acid (which plays a key role in the development of epileptic seizures).
Pharmacokinetics
Suction
After oral administration, it is quickly and completely absorbed from the intestine and is not significantly affected by the “first pass” effect. Cmax is reached 2.5 hours after oral administration. Eating slows down the absorption process, but does not affect its effectiveness. Bioavailability – 98%. The pharmacokinetics of the drug after a single dose in a dose not exceeding 450 mg is linear. The concentration in the equilibrium state has a pronounced individual character.
Distribution
Protein binding is 55%. It is unlikely that displacement of lamotrigine from protein binding would cause a toxic effect. Vd is 0.92-1.22 l/kg body weight. Excreted in breast milk. The concentration in breast milk is 40-60% of the plasma concentration. In some cases, the concentration of the drug in the blood serum of infants whose mothers took the drug during breastfeeding reaches therapeutic levels.
Metabolism
Biotransformed in the liver under the action of glucuronyl transferase uridine diphosphate. Among the metabolites, N-glucuronides predominate. Lamotrigine induces its own metabolism to a moderate extent and in a dose-dependent manner.
Removal
The average clearance at steady state in healthy adults is 39±14 ml/min. It is excreted in the urine in the form of a glucuronide conjugate, less than 10% in unchanged form, about 2% (unchanged and in the form of metabolites) in feces. Clearance and T1/2 do not depend on the dose. T1/2 in healthy volunteers is 24-35 hours.
Pharmacokinetics in special clinical situations
Clearance, calculated per kg of body weight, is higher in children than in adults, and is highest before 5 years of age. T1/2 in children is usually shorter than in adults.
T1/2 in children when used simultaneously with enzyme inducers is 7 hours, with sodium valproate – 45-60 hours.
The clearance of lamotrigine in elderly and younger patients differs minimally from each other.
Special instructions
Special instructions
There are no data confirming the clinically significant inducing and inhibitory effects of lamotrigine on oxidative enzymes in the liver. The ability of the drug to induce its own metabolism is low and probably has no clinical significance.
Lamolep should not be prescribed concomitantly with other drugs containing lamotrigine.
If Lamolep provides good control of epileptic seizures, other antiepileptic drugs can be discontinued.
An objective criterion for the effectiveness of treatment is the ability to reduce the frequency of peaks on the EEG by 78-98%.
In the first 8 weeks of treatment, skin reactions may develop. Skin rashes are usually mild and disappear spontaneously. Severe forms may develop, requiring hospitalization and discontinuation of lamotrigine therapy (for example, Stevens-Johnson syndrome and toxic epidermal necrolysis). The use of the drug in high initial doses and acceleration of the recommended rate of increase in the dose of lamotrigine, as well as the simultaneous use of valproic acid drugs, contribute to the appearance of skin rash. To reduce the likelihood of developing such dermatological reactions, the indicated doses and rates of increase should be strictly observed.
Children are more predisposed to developing severe forms of skin reactions (the incidence of cases requiring hospitalization in children is 1/300–1/100).
Early symptoms of an allergic rash can easily be confused with an infectious rash, so if high fever and rash occur in the first 8 weeks of treatment, a drug reaction should be suspected.
It is important to remember that early manifestations of hypersensitivity reactions (eg, fever, lymphadenopathy) can occur without a rash. If a rash appears (regardless of the patient’s age), the patient should be carefully examined immediately and lamotrigine therapy should be discontinued if the development of dermatological symptoms cannot be explained by another cause.
The appearance of a rash may be accompanied by various systemic manifestations of hypersensitivity (high body temperature, lymphadenopathy, facial swelling, reactions from the liver and hematopoietic system). The severity of hypersensitivity reactions can vary, and sometimes the development of disseminated intravascular coagulopathy and multiple organ functional failure is possible. It should be kept in mind that early signs of hypersensitivity (eg, high body temperature, lymphadenopathy) are not always accompanied by a skin rash.
Liver dysfunction is usually part of the hypersensitivity syndrome, but is not always accompanied by other symptoms.
Long-term treatment with lamotrigine may alter folic acid metabolism because Lamotrigine is a weak inhibitor of dihydrofolate reductase. At the same time, long-term, 12-month treatment with lamotrigine does not significantly affect the level of hemoglobin, the average volume of erythrocytes, the concentration of folic acid in plasma and erythrocytes, and after 5 years of treatment – on the concentration of folic acid.
If you are lactose intolerant, please note that tablets containing 25 mg of lamotrigine contain 16.35 mg of lactose monohydrate, containing 50 mg – 32.5 mg, 100 mg – 65 mg.
Despite the fact that when taking oral contraceptives, lamotrigine does not affect the concentrations of ethinyl estradiol and levonorgestrel, menstrual irregularities during lamotrigine therapy in patients taking oral contraceptives require close attention from the attending physician.
When treating patients with renal failure undergoing hemodialysis, it should be borne in mind that on average 20% of lamotrigine is excreted from the body during 4-hour hemodialysis.
Abrupt cessation of treatment with lamotrigine provokes epileptic seizures, including status epilepticus. Therefore, with the exception of special cases (for example, the appearance of a skin rash) requiring immediate cessation of therapy, discontinuation of the drug should be carried out gradually with a gradual dose reduction over 2 weeks.
Severe seizures and status epilepticus can lead to rhabdomyolysis, multiple organ failure, and disseminated intravascular coagulopathy, sometimes fatal. Similar cases have occurred in connection with the use of lamotrigine.
Bipolar disorders are characterized by suicidal tendencies, therefore, when prescribing the drug to patients with suicidal tendencies, careful monitoring of patients is required.
Impact on the ability to drive vehicles and operate machinery
During treatment, it is prohibited to drive a car or engage in activities that require increased concentration and speed of psychomotor reactions.
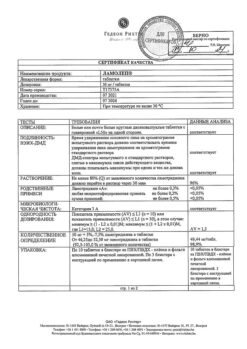
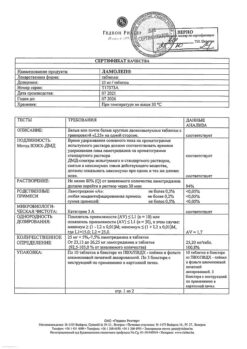
Active ingredient
Active ingredient
Lamotrigine
Composition
Composition
1 tab.:
lamotrigine 100 mg
Excipients:
silicon dioxide colloidal anhydrous,
magnesium stearate,
povidone,
sodium carboxymethyl starch,
lactose monohydrate,
microcrystalline cellulose.
Pregnancy
Pregnancy
Lamolep is contraindicated during pregnancy, unless the expected therapeutic benefit to the mother outweighs the potential risk to the fetus.
Due to the inhibitory effect of lamotrigine on dihydrofolate reductase, the development of fetal malformations is likely when the drug is used during pregnancy, but currently available data are insufficient to determine the degree of safety.
There is limited data on the use of the drug during breastfeeding. In some cases, the concentration of the drug in the blood serum of infants whose mothers took the drug during breastfeeding reaches therapeutic levels. When using the drug during lactation, you should carefully weigh the benefits of breastfeeding and the likelihood of side effects in the child.
Use in children
The drug is prescribed with caution to children as the drug of choice for monotherapy of epilepsy. Contraindication: children under 2 years of age.
Contraindications
Contraindications
children under 2 years of age;
pregnancy;
lactation period (breastfeeding);
hypersensitivity to lamotrigine or any component of the drug.
The drug should be prescribed with caution to patients with renal failure (due to possible accumulation of the glucuronide metabolite).
The drug is prescribed with caution to children as the drug of choice for monotherapy of epilepsy.
Use for liver dysfunction
In case of moderate liver dysfunction (class B on the Child-Pugh scale), the initial, increasing and maintenance doses should be reduced by approximately 50%, in severe cases (class C on the Child-Pugh scale) – by 75%. Incremental and maintenance doses should be adjusted based on clinical response.
Use for renal impairment
Caution should be exercised when prescribing the drug to patients with renal failure.
Use in elderly patients
No dosage adjustment is required in elderly patients (over 65 years of age) (since the pharmacokinetics in this age group do not differ from those in adults).
Side Effects
Side Effects
Adverse reactions are presented for each indication separately, using the following conditional classification of the frequency of adverse reactions: very often (>1/10), often (>1/100.1/1000, 1/10,000,
In patients with epilepsy
From the hematopoietic system: very rarely – neutropenia, leukopenia, anemia, thrombocytopenia, pancytopenia, aplastic anemia, agranulocytosis.
Allergic reactions: very often – in the first 8 weeks of therapy, skin rash (maculopapular), which disappears after discontinuation of lamotrigine; rarely – Stevens-Johnson syndrome, very rarely – hypersensitivity syndrome (including symptoms such as fever, lymphadenopathy, facial swelling, disorders of the blood and liver function, disseminated intravascular coagulation syndrome, multiorgan disorders), toxic epidermal necrolysis (Lyell’s syndrome, in some cases recovery with scarring).
From the side of the central nervous system: very often – headache; often – irritability, drowsiness, insomnia, dizziness, tremor, nystagmus, ataxia, anxiety; sometimes – aggressiveness; very rarely – increased excitability, hallucinations, confusion, imbalance, worsening of Parkinson’s disease, extrapyramidal disorders, choreoathetosis, increased frequency of convulsive seizures.
From the organ of vision: very often – diplopia, blurred vision; rarely – conjunctivitis.
From the digestive system: often – nausea, vomiting; very rarely – increased levels of liver enzymes, impaired liver function, liver failure.
Other: often – increased fatigue; very rarely – lupus-like syndrome.
In patients with bipolar disorders
In addition to the above symptoms, the following phenomena are also possible.
From the musculoskeletal system: often – arthralgia, myalgia, back pain.
Interaction
Interaction
When used concomitantly, valproic acid drugs competitively block liver enzymes and interfere with the metabolism of lamotrigine, almost doubling its average T1/2, extending it to 70 hours.
Antiepileptic drugs that induce liver enzymes (such as phenytoin, carbamazepine, phenabarbital and primidone), as well as paracetamol, stimulate the metabolism of lamotrigine and reduce its T1/2 by 2 times, up to 14 hours (phenytoin, carbamazepine). In patients taking carbamazepine, administration of lamotrigine may cause undesirable central nervous system effects, including dizziness, ataxia, diplopia, decreased visual acuity and nausea. Reducing the dose of carbamazepine usually leads to the disappearance of these phenomena.
With simultaneous use, lamotrigine does not affect the concentrations of other antiepileptic drugs in plasma, as well as the concentrations of ethinyl estradiol and levonorgestrel (which are part of simultaneously used oral contraceptives).
When used concomitantly, lamotrigine does not reduce the clearance of drugs metabolized by CYP2D6.
When used concomitantly, clozapine, phenelzine, risperidone, sertaline and trazodone do not appear to affect the clearance of lamotrigine.
There are no data on the effect of lamotrigine on the pharmacokinetics of other antiepileptic drugs and on drug interactions between it and drugs metabolized by isoenzymes of the cytochrome P450 system.
Possible combined use with sedatives, antiepileptic and anxiolytic drugs.
Overdose
Overdose
Symptoms: nystagmus, ataxia, headache, vomiting, drowsiness, impaired consciousness up to coma.
Treatment: hospitalization in a hospital and appropriate supportive and symptomatic therapy; if necessary, gastric lavage and administration of activated carbon.
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C
Shelf life
Shelf life
5 years
Manufacturer
Manufacturer
Gedeon Richter, Hungary
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Gedeon Richter, Hungary |
| Medication form | pills |
| Brand | Gedeon Richter |
Other forms…
Related products
Buy Lamolep, tablets 100 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.