No products in the cart.
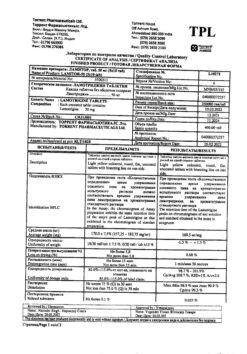
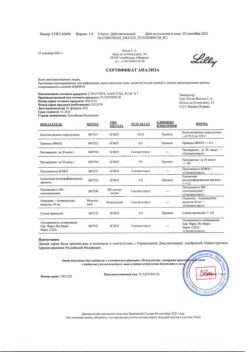
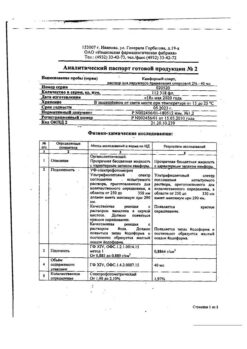
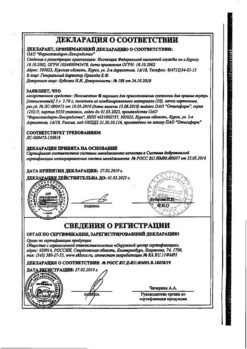
Lamictal, tablets 25 mg 30 pcs
€19.99 €17.33
Description
Partial and generalized seizures, including tonic-clonic and Lennox-Gastaud syndrome-related seizures (adults and children), bipolar disorders in adults over 18 years of age with predominantly depressive phases.
Indications
Indications
Partial and generalized seizures, including tonic-clonic and those associated with Lennox-Gastaut syndrome (in adults and children), bipolar disorders in adults over 18 years of age with predominantly depressive phases.
Pharmacological effect
Pharmacological effect
Anticonvulsant.
Special instructions
Special instructions
Skin rash
There is evidence of the development of skin rashes, which were usually noted during the first 8 weeks after the start of treatment with Lamictal. In most cases, skin rashes are mild and go away on their own, but sometimes serious cases have been reported that require hospitalization of the patient and discontinuation of Lamictal (for example, Stevens-Johnson syndrome and Lyell’s syndrome).
Severe skin reactions in adults taking Lamictal® in accordance with generally accepted recommendations develop with a frequency of approximately 1 in 500 patients with epilepsy. Approximately half of these cases have Stevens-Johnson syndrome (1 in 1000). In patients with bipolar disorder, the incidence of severe skin rashes in clinical studies is approximately 1 in 1000 patients.
Children are at higher risk of developing severe skin rashes than adults. The reported incidence of skin rashes requiring hospitalization in children with epilepsy ranged from 1 in 300 to 1 in 100 children.
In children, the initial manifestations of a rash may be mistaken for an infection, so the possibility of a reaction in children to the drug, manifested by the development of a rash and fever in the first 8 weeks of therapy, should be taken into account.
In addition, the overall risk of developing a rash is largely associated with a high initial dose of Lamictal and exceeding the recommended rate of increase, as well as with combined use with valproate drugs.
Caution is warranted when prescribing to patients with a history of allergic reactions or rash in response to other antiepileptic drugs, since the incidence of rash (not classified as serious) in patients with such a history was observed 3 times more often when prescribing lamotrigine than in patients with no history.
If a rash is detected, all patients (adults and children) should be examined by a doctor immediately. Lamotrigine should be discontinued immediately unless the rash appears to be unrelated to the drug. It is not recommended to restart lamotrigine in cases where its previous prescription was canceled due to the development of a skin reaction, unless the expected therapeutic effect of the drug outweighs the risk of side effects.
It has been reported that the rash may be part of a hypersensitivity syndrome associated with various systemic manifestations, including fever, lymphadenopathy, facial swelling, and hematologic and hepatic abnormalities. The severity of the syndrome varies widely and in rare cases can lead to the development of DIC and multiple organ failure. It should be noted that early manifestations of hypersensitivity syndrome (ie, fever, lymphadenopathy) can be observed even if there is no obvious manifestation of a rash. If such symptoms develop, the patient should be immediately examined by a physician and, unless another cause of the symptoms is determined, lamotrigine should be discontinued.
Aseptic meningitis
The development of aseptic meningitis is reversible when the drug is discontinued in most cases and resumes in some cases when the drug is re-administered. Repeated use results in a rapid return of symptoms, which are often more severe. Lamotrigine is not re-prescribed to patients in whom treatment discontinuation was associated with aseptic meningitis.
Hormonal contraceptives
1. Effect of hormonal contraceptives on the pharmacokinetics of lamotrigine
The combination drug ethinyl estradiol/levonorgestrel (30 mcg/150 mcg) has been shown to approximately double the clearance of lamotrigine, resulting in a decrease in plasma levels. When prescribing it, to achieve the maximum therapeutic effect, it is necessary to increase the maintenance doses of lamotrigine, but not more than 2 times. In women no longer taking lamotrigine glucuronidation inducers and taking hormonal contraceptives whose treatment regimen includes a week of taking an inactive drug (or a week’s break from taking the contraceptive), a gradual transient increase in lamotrigine concentrations will be observed during this period of time. The increase in concentration will be more pronounced if the next increase in the dose of lamotrigine is carried out immediately before or during the period of taking the inactive drug.
Health care providers should develop clinical skills to manage women who are starting or stopping hormonal contraceptives while on lamotrigine, as this may require lamotrigine dosage adjustments.
Other oral contraceptives and hormone replacement therapy have not been studied, although they may have a similar effect on the pharmacokinetic parameters of lamotrigine.
2. Effect of lamotrigine on the pharmacokinetics of hormonal contraceptives
Co-administration of lamotrigine and a combined hormonal contraceptive (ethinyl estradiol/levonorgestrel) leads to a moderate increase in the clearance of levonorgestrel and changes in the concentrations of FSH and LH. The effect of these changes on ovulatory activity of the ovaries is unknown. However, we cannot exclude the possibility that in some patients taking lamotrigine and hormonal contraceptives, these changes may cause a decrease in contraceptive effectiveness. Patients should be informed of the need to immediately inform the doctor about changes in the nature of the menstrual cycle, i.e. about sudden bleeding.
Dihydrofolate reductase
Lamotrigine is a weak inhibitor of dihydrofolate reductase, and therefore the drug may affect folate metabolism during long-term therapy. However, even with long-term use, lamotrigine has not been shown to cause significant changes in hemoglobin, mean red blood cell volume, serum folate concentrations (up to 1 year of use), or red blood cell concentrations (up to 5 years of use).
Effect of lamotrigine on the cationic transporter of organic substrates
Lamotrigine is an inhibitor of tubular secretion through its effect on the cationic protein transporter. This may lead to increased plasma concentrations of some drugs that are eliminated primarily through the kidneys. Co-administration of lamotrigine and substrates with a narrow therapeutic index, such as dofetilide, is not recommended.
Kidney failure
Single administration of lamotrigine to patients with severe renal failure did not reveal significant changes in lamotrigine concentrations. However, accumulation of the glucuronide metabolite is very likely, so caution should be exercised when treating patients with renal failure.
Patients taking other drugs containing lamotrigine
If the patient is receiving any other drug containing lamotrigine, he should not take Lamictal® without consulting a doctor.
Epilepsy
Abrupt discontinuation of lamotrigine, like other AEDs, can trigger the development of seizures. If abrupt cessation of therapy is not considered safe (eg, if rash occurs), the dose of lamotrigine should be reduced gradually over 2 weeks. There are reports in the literature that severe seizures, including status epilepticus, can lead to the development of rhabdomyolysis, multiple organ dysfunction and internally disseminated vascular coagulation, sometimes with fatal outcome. Similar cases were observed when treating patients with lamotrigine.
Suicidal risk
Symptoms of depression and/or bipolar disorder may occur in patients with epilepsy. Patients with epilepsy and comorbid bipolar disorder are at high risk of suicide. 25-50% of patients with bipolar disorder have had at least one suicide attempt; These patients may experience worsening suicidal thoughts and behavior (suicidality) while taking medications for bipolar disorder, including lamotrigine, or without treatment.
Suicidal ideation and behavior have been reported in patients taking AEDs for several indications, including epilepsy and bipolar disorder. A meta-analysis of randomized, placebo-controlled trials of AEDs (including lamotrigine) showed a small increase in suicide risk. The mechanism of this action is unknown, and available data do not exclude the possibility of an increased risk of suicide with lamotrigine. Therefore, patients should be closely monitored for suicidal thoughts and behavior. Patients and caregivers should be informed of the need for medical advice if such symptoms occur.
Bipolar affective disorder
Children and adolescents under 18 years of age
Treatment with antidepressants is associated with an increased risk of suicidal ideation and behavior in children and adolescents with major depression and other mental disorders.
Clinical worsening in patients with bipolar disorder
Patients with bipolar disorder receiving lamotrigine should be closely monitored for symptoms of clinical worsening (including the emergence of new symptoms) and suicidality, particularly during treatment initiation and at the time of dose changes. Patients with a history of suicidal ideation or behavior, young patients, and patients who have been identified as having significant suicidal ideation prior to treatment are at high risk for developing suicidal ideation or behavior and should be closely monitored during treatment.
Patients (and caregivers of patients) should be alerted to monitor for any deterioration in patients’ condition (including the appearance of new symptoms) and/or the emergence of suicidal thoughts/behaviors or thoughts of harming themselves and should seek medical attention immediately if these symptoms occur.
In this case, the situation should be assessed and appropriate changes to the treatment regimen should be made, including the possibility of discontinuing the drug in patients who experience clinical worsening (including the appearance of new symptoms) and/or the emergence of suicidal thoughts/behavior, especially if these symptoms are severe, of sudden onset and not previously noted.
Impact on the ability to drive vehicles and operate machinery
Two studies conducted in healthy volunteers showed that the effects of lamotrigine on fine visual-motor coordination, eye movements and subjective sedation were no different from placebo. There are reports of neurological side effects of lamotrigine, such as dizziness and diplopia. Therefore, before driving a car or operating machinery, patients should evaluate the effect of lamotrigine on their condition.
Because Since the effect of all antiepileptic drugs varies from person to person, patients should consult their doctor about their ability to drive.
Active ingredient
Active ingredient
Lamotrigine
Composition
Composition
1 tab. contains:
Pregnancy
Pregnancy
Since lamotrigine is a weak inhibitor of dihydrofolate reductase, there is at least
Contraindications
Contraindications
Hypersensitivity.
Use with caution in case of renal failure.
Side Effects
Side Effects
Available information on adverse events is divided into 2 parts: adverse events in patients with epilepsy and adverse events in patients with bipolar affective disorder. However, when considering the safety profile of lamotrigine as a whole, the information in both sections must be taken into account.
The adverse events presented below are listed depending on the anatomical and physiological classification and frequency of occurrence. The frequency of occurrence is determined as follows: very often (≥1/10), often (≥1/100,
Epilepsy
From the skin and subcutaneous fat: very often – skin rash; rarely – Stevens-Johnson syndrome, very rarely – toxic epidermal necrolysis.
In double-blind clinical trials in adults where lamotrigine was used as combination therapy, the incidence of skin rash was 10% in patients taking lamotrigine and 5% in patients taking placebo. In 2% of cases, the occurrence of skin rash was the reason for discontinuation of lamotrigine. The rash, mainly maculopapular in nature, usually appears within the first 8 weeks of starting therapy and resolves after discontinuation of the drug.
There have been reports of rare cases of severe, potentially life-threatening skin lesions, including Stevens-Johnson syndrome and toxic epidermal necrolysis (Lyell’s syndrome). Although most symptoms reversed when the drug was discontinued, some patients were left with permanent scarring, and in rare cases, drug-related deaths have been reported.
The overall risk of developing rash was significantly associated with the high initial dose of lamotrigine and exceeding the recommended rate of lamotrigine dose titration, as well as with concomitant administration of valproic acid. The development of a rash has also been considered a manifestation of a hypersensitivity syndrome associated with various systemic manifestations.
From the hematopoietic organs and lymphatic system: very rarely – hematological disorders (neutropenia, leukopenia, anemia, thrombocytopenia, pancytopenia, aplastic anemia, agranulocytosis), lymphadenopathy. Hematologic abnormalities and lymphadenopathy may or may not be associated with hypersensitivity syndrome.
From the immune system: very rarely – hypersensitivity syndrome (including symptoms such as fever, lymphadenopathy, swelling of the face, disorders of the blood and liver function, disseminated intravascular coagulation syndrome, multiple organ failure). The rash is also considered to be part of a hypersensitivity syndrome associated with various systemic manifestations, including fever, lymphadenopathy, facial swelling, and blood and liver abnormalities. The syndrome occurs with varying degrees of severity and can, in rare cases, lead to the development of DIC syndrome and multiple organ failure. It is important to note that early manifestations of hypersensitivity (ie, fever, lymphadenopathy) may occur even in the absence of obvious signs of rash. If such symptoms develop, the patient should be immediately examined by a doctor and, unless another cause for the development of symptoms is established, lamotrigine should be discontinued.
From the mental side: often – aggressiveness, irritability; very rarely – tics, hallucinations, confusion.
From the side of the central nervous system: with monotherapy: very often – headache; often – drowsiness, insomnia, dizziness, tremor; infrequently – ataxia; rarely – nystagmus. As part of combination therapy: very often – drowsiness, ataxia, headache, dizziness; often – nystagmus, tremor, insomnia; very rarely – aseptic meningitis, agitation, gait instability, movement disorders, worsening symptoms of Parkinson’s disease, extrapyramidal disorders, choreoathetosis, increased frequency of convulsive seizures. There are reports that lamotrigine may worsen extrapyramidal symptoms of parkinsonism in patients with concomitant Parkinson’s disease, and in isolated cases cause extrapyramidal symptoms and choreathetosis in patients without previous disorders.
From the senses: with monotherapy: infrequently – diplopia, blurred vision; as part of combination therapy: very often – diplopia, blurred vision; rarely – conjunctivitis.
From the digestive system: with monotherapy: often – nausea, vomiting, diarrhea; as part of combination therapy: very often – nausea, vomiting; often – diarrhea.
From the liver and biliary tract: very rarely – increased activity of liver enzymes, impaired liver function, liver failure. Liver dysfunction usually develops in combination with symptoms of hypersensitivity, but in isolated cases they have been observed in the absence of obvious signs of hypersensitivity.
From the side of muscle and connective tissue: very rarely – lupus-like syndrome.
Other: often – fatigue.
Bipolar affective disorder
To assess the overall safety profile of lamotrigine, the following adverse events should be taken into account along with those specific to epilepsy.
From the skin and subcutaneous fat: very often – skin rash; rarely – Stevens-Johnson syndrome. In an assessment of all studies (controlled and uncontrolled) examining the use of Lamictal in patients with bipolar affective disorder, skin rash occurred in 12% of all patients receiving lamotrigine, whereas the incidence of skin rash in controlled studies alone was 8% in patients receiving Lamictal® and in 6% of patients receiving placebo.
From the side of the central nervous system: very often – headache; often – agitation, drowsiness, dizziness.
From the side of muscle and connective tissue: often – arthralgia.
From the digestive system: often – dryness of the oral mucosa.
Other: often – pain, back pain.
Interaction
Interaction
UDP-glucuronyl transferase is the main enzyme that metabolizes lamotrigine. There is no data on the ability of lamotrigine to cause clinically significant induction or inhibition of liver microsomal enzymes. In this regard, interaction between lamotrigine and drugs metabolized by isoenzymes of the cytochrome P450 system is unlikely. Lamotrigine may induce its own metabolism, but this effect is moderate and has no clinical significance.
The effect of other drugs on the glucuronidation of lamotrigine.
Potent inhibitors of lamotrigine glucuronidation
Potent inducers of lamotrigine glucuronidation
Drugs that have little effect on the glucuronidation of lamotrigine
valproic acid
carbamazepine
phenytoin
primidone
phenobarbital
rifampicin
lopinavir/ritonavir
atazanavir/ritonavir
combination drug ethinyl estradiol/levonorgestrel
lithium preparations
bupropion
olanzapine
oxcarbazepine
felbamate
gabapentin
levetiracetam
pregabalin
topiramate
zonisamide
aripiprazole
The effects of other oral contraceptives and hormone replacement therapy have not been studied, although they may have a similar effect on the pharmacokinetic parameters of lamotrigine.
Interaction with PEP
Valproic acid, which inhibits the glucuronidation of lamotrigine, reduces the rate of its metabolism and prolongs its average T1/2 by almost 2 times.
Some antiepileptic drugs (such as phenytoin, carbamazepine, phenabarbital and primidone) that induce liver microsomal enzymes accelerate the glucuronidation of lamotrigine and its metabolism. CNS adverse events have been reported, including dizziness, ataxia, diplopia, blurred vision and nausea in patients started taking carbamazepine during lamotrigine therapy. These symptoms usually resolved after reducing the dose of carbamazepine. A similar effect was observed when lamotrigine and oxcarbazepine were administered to healthy volunteers; the effect of dose reduction was not studied.
With the simultaneous administration of lamotrigine at a dose of 200 mg and oxcarbazepine at a dose of 1200 mg, neither oxcarbazepine nor lamotrigine disrupt each other’s metabolism.
The combined use of felbamate at a dose of 1200 mg 2 times a day and lamotrigine 100 mg 2 times a day did not lead to clinically significant changes in the pharmacokinetics of lamotrigine.
When lamotrigine and gabapentin were co-administered, the apparent clearance of lamotrigine did not change.
Potential drug interactions between levetiracetam and lamotrigine were investigated by assessing serum concentrations of both drugs in placebo-controlled clinical studies. These data indicate that lamotrigine and levetiracetam do not affect each other’s pharmacokinetics.
There was no effect of pregabalin at a dose of 200 mg 3 times / day on the equilibrium concentrations of lamotrigine, i.e. Pregabalin and lamotrigine do not interact pharmacokinetically with each other.
The use of topiramate did not lead to changes in lamotrigine plasma concentrations. However, lamotrigine resulted in a 15% increase in topiramate concentrations.
Taking zonisamide (at a dose of 200-400 mg/day) during a clinical program together with lamotrigine (at a dose of 150-500 mg/day) did not lead to changes in the pharmacokinetic parameters of lamotrigine.
Studies have shown that lamotrigine does not affect plasma concentrations of other antiepileptic drugs.
The results of in vitro studies showed that lamotrigine does not displace other antiepileptic drugs from binding to plasma proteins.
Interaction when used in combination with other psychotropic drugs
Lamotrigine at a dose of 100 mg/day does not interfere with the pharmacokinetics of anhydrous lithium gluconate (2 g 2 times/day for 6 days) when administered together.
Repeated oral administration of bupropion does not have a statistically significant effect on the pharmacokinetics of a single dose of lamotrigine and causes a slight increase in the AUC of lamotrigine glucuronide.
Olanzapine at a dose of 15 mg reduces the AUC and Cmax of lamotrigine by an average of 24% and 20%, respectively, which is clinically insignificant. Lamotrigine at a dose of 200 mg does not change the pharmacokinetics of olanzapine.
Repeated administration of lamotrigine at a dose of 400 mg/day did not have a clinically significant effect on the pharmacokinetics of risperidone after a single dose of 2 mg in healthy volunteers. At the same time, drowsiness was noted: in 12 out of 14 patients when taking lamotrigine and risperidone in combination; in 1 in 20 patients when taking risperidone alone; in none of the patients taking lamotrigine alone.
Inhibition of the action of lamotrigine by amitriptyline, bupropion, clonazepam, fluoxetine, haloperidol or lorazepam has minimal effect on the formation of lamotrigine’s primary metabolite 2-N-glucuronide.
A study of the metabolism of bufuralol by liver microsomal enzymes isolated from humans allows us to conclude that lamotrigine does not reduce the clearance of drugs metabolized primarily by CYP2D6 isoenzymes. Results from in vitro studies also suggest that clozapine, phenelzine, risperidone, sertraline or trazodone are unlikely to affect the clearance of lamotrigine.
Interaction with hormonal contraceptives
1. Effect of hormonal contraceptives on the pharmacokinetics of lamotrigine
Taking combined oral contraceptives containing 30 mcg ethinyl estradiol and 150 mcg levonorgestrel causes an approximately two-fold increase in the clearance of lamotrigine (after oral administration), resulting in a decrease in lamotrigine AUC and Cmax by an average of 52% and 39%, respectively. During the week without taking the active drug, an increase in lamotrigine plasma concentrations is observed, with lamotrigine concentrations measured at the end of this week before the next dose being administered on average 2 times higher than during the period of active therapy.
2. Effect of lamotrigine on the pharmacokinetics of hormonal contraceptives
During the period of equilibrium concentrations, lamotrigine at a dose of 300 mg does not affect the pharmacokinetics of ethinyl estradiol, a component of the combined oral contraceptive. There is a slight increase in the clearance of the second component of the oral contraceptive, levonorgestrel, which leads to a decrease in the AUC and Cmax of levonorgestrel by 19% and 12%, respectively. Measurements of serum levels of FSH, LH, and estradiol during this study revealed a slight decrease in ovarian hormonal suppression in some women, although measurements of plasma progesterone levels in none of the 16 women revealed hormonal evidence of ovulation. The effect of a moderate increase in levonorgestrel clearance and changes in plasma concentrations of FSH and LH on ovulatory activity of the ovaries has not been established. The effect of other doses of lamotrigine (except 300 mg/day) has not been studied and studies involving other hormonal drugs have not been conducted.
Interaction with other drugs
Rifampicin increases the clearance of lamotrigine and reduces its T1/2 due to the induction of liver microsomal enzymes responsible for glucuronidation. In patients taking rifampicin as concomitant therapy, the lamotrigine regimen should be consistent with the regimen recommended for co-administration of lamotrigine and glucuronidation-inducing agents.
An approximately 50% decrease in lamotrigine plasma concentrations was observed with lopinavir/ritonavir, possibly due to induction of glucuronidation. In patients receiving concomitant treatment with lopinavir/ritonavir, a dosing regimen of lamotrigine with concomitant inducers of glucuronidation should be recommended.
In a study in healthy volunteers, atazanavir/ritonavir (300 mg/100 mg) decreased the AUC and Cmax of lamotrigine (100 mg single dose) by approximately 32% and 6%, respectively.
The results of in vitro studies showed that lamotrigine is an inhibitor of cationic transporters of organic substrates in potentially clinically significant concentrations. These data indicate that lamotrigine is a more potent inhibitor (half inhibitory concentration (IC50) ranging from 53.8 nmol/L to 186 nmol/L, respectively) than cimetidine.
Interaction, including laboratory values
Lamotrigine has been reported to interfere with some rapid urinalysis tests for illicit drugs, which may result in false-positive results, particularly for phencyclidine (a dissociative anesthetic). A more specific alternative chemical method must be used to confirm a positive result.
Overdose
Overdose
Single administration doses exceeding the maximum therapeutic dose by 10-20 times have been reported. An overdose was manifested by the following symptoms: nystagmus, ataxia, impaired consciousness and coma.
Treatment: Hospitalization and supportive care are recommended in accordance with the clinical picture or recommendations of the national poison control center.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 30 °C
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
GlaxoSmithKline Pharmaceuticals S.A., Poland
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 30 °C |
| Manufacturer | GlaxoSmithKline Pharmaceuticals S.A., Poland |
| Medication form | pills |
| Brand | GlaxoSmithKline Pharmaceuticals S.A. |
Other forms…
Related products
Buy Lamictal, tablets 25 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.