No products in the cart.
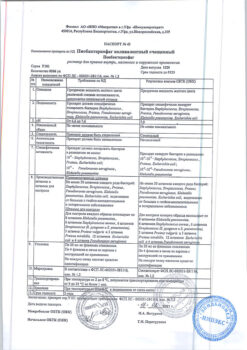
Jaquinus, 5 mg 56 pcs.
€1415.32 €1179.43
Description
Jaquinus is a selective immunosuppressant. Tofacitinib is a potent, selective inhibitor of the Janus kinase family with high selectivity against other kinases of the human genome. According to the results of kinase studies, tofacitinib inhibits Janus kinases 1, 2, 3 and, to a lesser extent, tyrosine kinase 2.
In those cells where janus kinases transmit signals in pairs, tofacitinib preferentially inhibits the signal transduction of heterodimeric receptors associated with janus kinase-3 and/or janus kinase-1, with functional selectivity for receptors that transmit signals via janus kinase-2 pairs. Inhibition of janus kinase-1 and janus kinase-3 by tofacitinib blocks signaling through common receptors containing gamma chains against several cytokines including IL-2, -4, -7, -9, -15 and -21.
These cytokines have an integrating role in the processes of lymphocyte activation, proliferation, function and inhibition of signal transduction, leading to modulation of diverse aspects of the immune response. In addition, inhibition of Janus kinase-1 leads to attenuation of signal transduction by additional proinflammatory cytokines, such as IL-6 and IFN-γ. At higher drug exposure, inhibition of Janus kinase-2 signaling leads to inhibition of erythropoietin signaling.
Pharmacodynamic effects
The treatment with Jaquinus is accompanied by a dose-dependent decrease in circulating CD16/56+ natural killer cells. The estimated maximum reduction is achieved after about 8-10 weeks of therapy. The described changes usually resolve 2-6 weeks after the end of therapy. Treatment with Jaquinus was accompanied by a dose-dependent increase in the number of B-cells. Changes in the number of circulating T-lymphocytes and their subpopulations were insignificant and inconstant. The clinical significance of these changes is unknown. The change in total serum IgG, M and A levels during the 6-month treatment period in patients with rheumatoid arthritis was small, dose-independent and similar to that with placebo.
After treatment with Jaquinus, patients with rheumatoid arthritis experienced a rapid decrease in serum C-reactive protein (CRP) that persisted throughout the treatment period. The changes in C-RB levels observed during treatment with Jaquinus did not persist for 2 weeks after discontinuation of therapy, indicating a longer duration of pharmacodynamic activity compared to the half-life.
Pharmacokinetics
Absorption and distribution
The pharmacokinetics profile of tofacitinib is characterized by rapid absorption (Cmax is reached within 05-1 h), rapid excretion (T1/2 about 3 h) and dose-proportional increase in systemic exposure. Css is reached within 24-48 h with slight accumulation after administration 2 times/day.
Tofacitinib is well absorbed with a bioavailability of 74%. Administration of tofacitinib with fat-rich foods was not accompanied by changes in AUC, while Cmax in plasma is reduced by 32%. In clinical trials tofacitinib was used regardless of food intake.
The binding of tofacitinib to plasma proteins is approximately 40%. Tofacitinib predominantly binds to1-acid glycoprotein.
It is equally distributed between erythrocytes and blood plasma.
Metabolism and excretion
The excretion of tofacitinib is approximately 70% by metabolism in the liver and 30% by excretion by the kidneys as unchanged tofacitinib. Metabolism of tofacitinib is predominantly mediated by CYP3A4 isoenzyme and to a lesser extent by CYP2C19 isoenzyme. In a study of radioactively labeled tofacitinib, more than 65% of the total circulating radioactivity was due to unchanged tofacitinib and the remaining 35% was due to 8 metabolites (each less than 8% of the total radioactivity). Pharmacological activity was associated with unmetabolized tofacitinib.
Pharmacokinetics in patients with rheumatoid arthritis
The AUC of tofacitinib at minimum and maximum body weight (40 and 140 kg) was found to be similar to that of 70 kg in patients with rheumatoid arthritis.
The AUC was less than 5% higher in elderly patients aged 80 years compared to patients aged 55 years.
The AUC of tofacitinib was 7% lower in women compared to men.
The data also showed no significant difference (< 5%) in the AUC of tofacitinib in Caucasian, Negroid and Asian patients.
A nearly linear relationship between body weight and Vd was observed, resulting in a higher Cmax and lower Cmin in plasma in patients with lower body weight. However, this difference is not considered clinically significant. The interindividual variability (% coefficient of variability) of the AUC for tofacitinib is approximately 27%.
Pharmacokinetics in Special Clinical Cases
Patients with mild, moderate or severe renal impairment had higher AUCs of 37%, 43% and 123%, respectively, compared to healthy volunteers. In patients with end-stage renal failure, the contribution of dialysis to the total clearance of tofacitinib is relatively small.
In patients with mild to moderate hepatic impairment, AUCs were 3% and 65% higher than in healthy volunteers. Patients with severe hepatic impairment have not been studied.
Tofacitinib pharmacokinetics, safety and efficacy in children have not been studied.
Indications
Indications
Moderate to severe active rheumatoid arthritis in adults with an inadequate response to one or more disease-modifying anti-inflammatory drugs (DMARDs).
Pharmacological effect
Pharmacological effect
Jaquinus is a selective immunosuppressant. Tofacitinib is a potent, selective inhibitor of the Janus kinase family with high selectivity for other kinases in the human genome. Based on the results of kinase studies, tofacitinib inhibits Janus kinases 1, 2, 3 and, to a lesser extent, tyrosine kinase 2.
In cells where Janus kinases signal in pairs, tofacitinib preferentially inhibits heterodimeric receptor signaling associated with Janus kinase 3 and/or Janus kinase 1, having functional selectivity for receptors that signal through Janus kinase 2 pairs. Inhibition of Janus kinase 1 and Janus kinase 3 by tofacitinib blocks signaling through common gamma chain receptors for several cytokines, including IL-2, -4, -7, -9, -15 and -21.
These cytokines play an integral role in the processes of lymphocyte activation, proliferation, function and inhibition of signal transduction, which leads to the modulation of various aspects of the immune response. In addition, inhibition of Janus kinase 1 leads to attenuation of signal transduction by additional proinflammatory cytokines such as IL-6 and IFN-γ. At higher drug exposures, inhibition of Janus kinase 2 signaling results in inhibition of erythropoietin signaling.
Pharmacodynamic effects
Treatment with Yaquinus is accompanied by a dose-dependent decrease in circulating natural killer cells CD16/56+. The estimated maximum reduction is achieved approximately 8-10 weeks after initiation of therapy. The described changes usually resolve 2-6 weeks after the end of therapy. Treatment with Yaquinus was associated with a dose-dependent increase in the number of B cells. Changes in the number of circulating T lymphocytes and their subpopulations were small and inconsistent. The clinical significance of these changes is unknown. Changes in total serum levels of IgG, M, and A during the 6-month treatment period in patients with rheumatoid arthritis were small, dose-independent, and similar to placebo.
After treatment with Yaquinus in patients with rheumatoid arthritis, a rapid decrease in serum C-reactive protein (CRP) was observed, which persisted throughout the treatment period. Changes in CRP levels noted during treatment with Yaquinus did not resolve within 2 weeks after discontinuation of therapy, indicating a longer duration of pharmacodynamic activity compared to the half-life.
Pharmacokinetics
Suction and distribution
The pharmacokinetic profile of tofacitinib is characterized by rapid absorption (Cmax achieved within 0.5-1 hour), rapid elimination (T1/2 about 3 hours) and a dose-proportional increase in systemic exposure. Css is achieved within 24-48 hours with slight accumulation after dosing 2 times a day.
Tofacitinib is well absorbed and its bioavailability is 74%. Administration of tofacitinib with a meal rich in fat was not associated with changes in AUC, while plasma Cmax decreased by 32%. In clinical studies, tofacitinib was administered without regard to food intake.
The binding of tofacitinib to plasma proteins is approximately 40%. Tofacitinib binds preferentially to the 1-acid glycoprotein.
Equally distributed between red blood cells and blood plasma.
Metabolism and excretion
Elimination of tofacitinib is approximately 70% via hepatic metabolism and 30% via renal excretion as unchanged tofacitinib. The metabolism of tofacitinib is predominantly mediated by the CYP3A4 isoenzyme and to a lesser extent by the CYP2C19 isoenzyme. In a study of radiolabeled tofacitinib, more than 65% of the total circulating radioactivity was due to unchanged tofacitinib, and the remaining 35% was due to 8 metabolites (each representing less than 8% of the total radioactivity). Pharmacological activity is associated with unmetabolized tofacitinib.
Pharmacokinetics in patients with rheumatoid arthritis
It was found that in patients with rheumatoid arthritis, the AUC of tofacitinib at minimum and maximum body weight (40 and 140 kg) was similar to that in patients weighing 70 kg.
In elderly patients aged 80 years, the AUC was less than 5% higher compared with patients aged 55 years.
The AUC of tofacitinib is 7% lower in women compared to men.
The data also showed no significant differences (<5%) in the AUC of tofacitinib in Caucasian, Black and Asian patients.
There was an almost linear relationship between body weight and Vd, which leads to higher Cmax and lower Cmin in blood plasma in patients with lower body weight. However, this difference is not considered clinically significant. The interindividual variability (% coefficient of variability) of the AUC for tofacitinib is approximately 27%.
Pharmacokinetics in special clinical situations
In patients with mild, moderate or severe renal impairment, AUC values were 37%, 43% and 123% higher, respectively, compared with healthy volunteers. In patients with end-stage renal disease, the contribution of dialysis to the overall clearance of tofacitinib is relatively small.
In patients with mild to moderate hepatic impairment, AUC values were 3% and 65% higher than those in healthy volunteers. Patients with severe hepatic impairment have not been studied.
The pharmacokinetics, safety and efficacy of tofacitinib have not been studied in children.
Special instructions
Special instructions
Serious infections
Serious and sometimes fatal infections due to bacterial, mycobacterial, fungal, viral, or other opportunistic pathogens have been reported in patients with rheumatoid arthritis receiving immunomodulators, including biologics and Jaquinus. The most common serious infections reported with use of Jaquinus include pneumonia, subcutaneous inflammation, herpes zoster, and urinary tract infection. Among the opportunistic infections when using the drug Yaquinus, cases of the development of tuberculosis and other mycobacterial infections, cryptococcosis, esophageal candidiasis, herpes zoster with damage to various dermatomes, cytomegalovirus infection, and BK virus infection were noted. In some patients, disseminated diseases were noted, most often with the simultaneous use of immunomodulators – methotrexate or corticosteroids, which in themselves and in addition to the underlying disease, rheumatoid arthritis, can predispose to the development of infections. It is also possible to develop other serious infections that were not reported in clinical studies (for example, histoplasmosis, coccidioidomycosis and listeriosis).
Jaquinus should not be used in patients with active infection, including localized infections. Before using Yaquinus, the risk/benefit ratio of therapy should be assessed in patients with chronic or recurrent infection, after contact with a patient with tuberculosis with a history of severe or opportunistic infection, in patients who have lived in or recently visited areas where tuberculosis or mycoses are endemic, as well as in patients with a predisposition to developing infection. Patients should be closely monitored for the development of signs and symptoms of infection during and after therapy with Jaquinus. Jaquinus should be temporarily discontinued if the patient develops a serious infection, opportunistic infection, or sepsis. If a new infection develops while using the drug Yaquinus, the patient is subject to a rapid and complete diagnostic examination, similar to a patient suffering from immunodeficiency. The appointment of appropriate antibacterial therapy, as well as careful dynamic monitoring, is indicated.
Since older patients usually have a higher incidence of infections, caution should also be exercised in such cases.
Tuberculosis
Before using Yaquinus, you should be screened for signs of latent or active tuberculosis infection.
Before initiating therapy with Yaquinus in patients with a history of latent or active tuberculosis, in the absence of confirmation of an adequate course of anti-tuberculosis therapy, as well as in patients with a negative test result for latent tuberculosis, but the presence of risk factors for tuberculosis infection, appropriate anti-tuberculosis therapy should be administered. When making a decision regarding the need for anti-tuberculosis therapy for each individual patient, it is recommended to consult with a TB specialist.
Patients should be closely monitored for development of signs of tuberculosis, including patients who test negative for latent tuberculosis before initiating therapy.
The incidence of tuberculosis with the use of the drug Yaquinus in the global clinical development program was 0.1-0.2%. Patients with latent tuberculosis are subject to standard antimycobacterial therapy before starting therapy with Yaquinus.
Reactivation of viral infections
Reactivation of viral infections has been described with DMARD therapy. Cases of reactivation of the herpes virus (for example, herpes zoster) have also been described in clinical studies of the drug Jaquinus. The effect of Yaquinus on the reactivation of chronic viral hepatitis is unknown. Patients testing positive for hepatitis B and C were excluded from clinical studies. Screening for the presence of viral hepatitis should be performed before initiating therapy with Yaquinus.
Malignant and lymphoproliferative diseases (except non-melanoma skin cancer)
There is a possibility that Jaquinus affects the body’s defense against malignant neoplasms. The effect of therapy with Yaquinus on the development and course of malignant neoplasms is unknown, however, in clinical studies of this drug, cases of the development of malignant neoplasms were recorded.
Non-melanoma skin cancer (NSMC)
Cases of development of SCNM have been reported in patients receiving tofacitinib therapy. Periodic skin examination is recommended in patients at increased risk of developing skin cancer.
Cases of perforation of the gastrointestinal tract
Clinical studies of patients with rheumatoid arthritis have reported cases of gastrointestinal perforation, although the role of Janus kinase inhibition in these events is unknown. Such cases have mainly been described as diverticulum perforation, peritonitis, abscess and appendicitis. All patients who developed perforation of the gastrointestinal tract received concomitant therapy with NSAIDs and/or corticosteroids. The relative contribution of concomitant therapy and the use of Yaquinus in the development of gastrointestinal perforation is unknown.
Jaquinus should be used with caution in patients at increased risk of gastrointestinal perforation (eg, patients with a history of diverticulitis). Patients with new GI symptoms should be immediately evaluated for early detection of GI perforation.
Laboratory indicators
Neutrophils: Treatment with Yaquinus was associated with an increased incidence of neutropenia (less than 2000/mcL) compared to placebo. Treatment with Yaquinus in patients with low neutrophil concentrations (ANC less than 1000/mcL) is not recommended. In patients with a persistent decrease in ANC to 500-1000 cells/µl, the dose of Yaquinus should be reduced or treatment should be discontinued until the ANC concentration reaches more than 1000 cells/µl. In patients with an absolute neutrophil count less than 500/µl, treatment is not recommended. Neutrophil levels should be monitored after 4-8 weeks of therapy and then every 3 months.
Hemoglobin: It is not recommended to initiate therapy with Yaquinus in patients with low hemoglobin levels (less than 90 g/l). Treatment with Yaquinus should be discontinued in patients with a hemoglobin level of less than 80 g/L, or if the hemoglobin level decreases by 20 g/L or more during treatment. Hemoglobin should be monitored initially, after 4-8 weeks of therapy, and then every 3 months.
Lipids: treatment with Yaquinus is accompanied by an increase in blood lipid levels – total cholesterol, LDL cholesterol, and HDL cholesterol. Maximum effect was usually observed within 6 weeks. Assessment of lipid parameters should be performed approximately 4-8 weeks after the start of therapy. The use of statins in patients with elevated concentrations of total cholesterol and LDL cholesterol during therapy with Yaquinus allows achieving baseline values.
Vaccination
Information on vaccination response or secondary transmission of infection when live vaccines are administered to patients receiving Jaquinus is not yet available. It is not recommended to administer live vaccines at the same time as Jaquinus. It is recommended that all patients receive required immunizations in accordance with current vaccination recommendations before starting Yaquinus.
Patients with impaired renal function
In clinical studies, Yaquinus was not studied in patients with initial creatinine clearance <40 ml/min.
Impact on the ability to drive vehicles and operate machinery
Studies of the effect of the drug Yaquinus on the ability to drive a car and operate machinery have not been conducted.
Active ingredient
Active ingredient
Tofacitinib
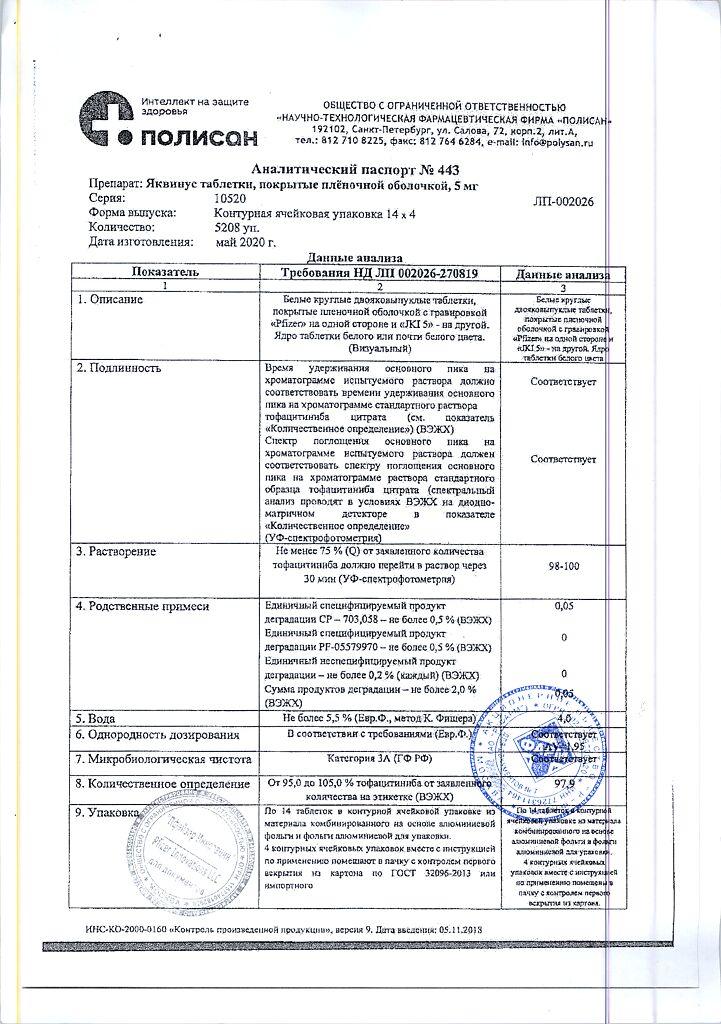
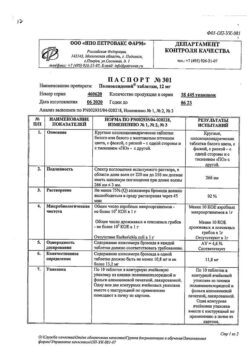
Composition
Composition
1 film-coated tablet contains:
active ingredient:
tofacitinib citrate 8.078 mg, which corresponds to the content of tofacitinib 5 mg,
excipients:
microcrystalline cellulose – 122.615 mg,
lactose monohydrate – 61.307 mg,
croscarmellose sodium – 6 mg,
magnesium stearate – 2 mg.
film shell composition:
opadry white – 6 mg (hypromellose – 2.4 mg, titanium dioxide – 1.5 mg, lactose monohydrate – 1.26 mg, macrogol – 0.48 mg, triacetin – 0.36 mg).
Pregnancy
Pregnancy
Adequate, well-controlled studies of the use of Yaquinus in pregnant women have not been conducted.
The ability of tofacitinib to pass into breast milk in humans has not been studied. Breastfeeding should be discontinued during therapy with Yaquinus.
Contraindications
Contraindications
hypersensitivity to tofacitinib or any other component of the drug Yaquinus.
severe liver dysfunction;
infection with hepatitis B and/or C viruses (presence of serological markers of HBV and HCV infection);
CC less than 40 ml/min;
simultaneous use of live vaccines;
the simultaneous use of the drug Yaquinus with biological drugs such as TNF inhibitors, interleukin antagonists (IL-1R, IL-6R), monoclonal anti-CD20 antibodies, selective costimulatory modulators, as well as powerful immunosuppressants such as azathioprine, cyclosporine and tacrolimus should be avoided, since this combination increases the likelihood of severe immunosuppression and the risk of developing infection;
severe infections, active infections, including local ones;
pregnancy (safety and effectiveness have not been studied);
breastfeeding period;
children and adolescents under 18 years of age (safety and effectiveness have not been studied);
lactase deficiency, lactose intolerance, glucose-galactose malabsorption.
With caution: with an increased risk of perforation of the gastrointestinal tract (for example, in patients with a history of diverticulitis); in elderly patients due to the high risk of developing infectious diseases.
Side Effects
Side Effects
The most common serious adverse reactions observed during tofacitinib therapy were serious infections.
The most common adverse reactions during the first 3 months of controlled clinical trials (occurring in more than 2% of patients receiving Jaquinus alone or in combination with DMARDs) included upper respiratory tract infections, headache, nasopharyngitis and diarrhea.
Discontinuation of therapy due to any adverse reaction during double-blind, placebo-controlled studies was required in 6.8% of patients in the Yaquinus group and 3.7% of patients in the placebo group.
The most common adverse reactions leading to discontinuation of Yaquinus were infections. The most common infections leading to discontinuation of therapy included herpes zoster and pneumonia.
Within each frequency group, adverse reactions are presented in order of decreasing severity.
Infections and parasitic infestations: very often – nasopharyngitis; often – pneumonia, herpes zoster, bronchitis, influenza, sinusitis, urinary tract infections, pharyngitis; uncommon – sepsis, bacterial pneumonia, pneumococcal pneumonia, pyelonephritis, inflammation of subcutaneous fat, viral gastroenteritis, viral infection, herpes simplex; rarely – central nervous system tuberculosis, encephalitis, necrotizing fasciitis, cryptococcal meningitis, disseminated tuberculosis, urosepsis, pneumonia caused by Pneumocystis jiroveci, staphylococcal bacteremia, tuberculosis, bacterial arthritis, atypical infection caused by mycobacteria, infection caused by Mycobacterium avium complex, cytomegalovirus infection, bacteremia.
From the cardiovascular system: often – increased blood pressure.
From the digestive system: often – abdominal pain, vomiting, gastritis, diarrhea, nausea, dyspepsia; infrequently – hepatic steatosis.
Metabolism: often – hyperlipidemia, dyslipidemia; infrequently – dehydration.
From the nervous system: often – headache, insomnia; infrequently – paresthesia.
From the musculoskeletal system: often – pain in muscles and bones, arthralgia; uncommon – tendonitis, joint swelling, muscle tension.
From the hemostatic system: often – leukopenia, anemia; infrequently – neutropenia.
From the respiratory system: often – shortness of breath, cough; infrequently – congestion in the paranasal sinuses.
From the skin: often – rash; infrequently – erythema, skin itching.
Benign, malignant and unspecified neoplasms (including cysts and polyps): uncommon – skin cancer not associated with melanoma.
Laboratory and instrumental indicators: often – increased activity of liver enzymes, CPK, increased concentrations of LDL, blood cholesterol (in clinical studies, they were first noted after the first month of therapy and subsequently remained stable), increased body weight; uncommon – increased transaminase activity, increased plasma creatinine concentration, increased GGTP concentration, impaired liver function tests.
Other: often – fever, fatigue, peripheral edema.
Interaction
Interaction
Interactions affecting the use of Yaquinus
Since tofacitinib is metabolized by the CYP3A4 isoenzyme, interactions with drugs that inhibit or induce this isoenzyme are highly likely. When used simultaneously with strong inhibitors of the CYP3A4 isoenzyme (for example, ketoconazole), as well as when used simultaneously with one or more moderate inhibitors of the CYP3A4 isoenzyme and strong inhibitors of the CYP2C19 isoenzyme (for example, fluconazole), the exposure of tofacitinib is increased. Co-administration of ketoconazole (a strong CYP3A4 inhibitor) and a single dose of tofacitinib increased the AUC and Cmax of tofacitinib by 103% and 16%, respectively. Co-administration of fluconazole (a moderate CYP3A4 inhibitor and a strong CYP2C19 inhibitor) increases the AUC and Cmax of tofacitinib by 79% and 27%, respectively.
When used concomitantly with strong inducers of the CYP3A4 isoenzyme (for example, rifampicin), the exposure to tofacitinib is reduced. Concomitant use of rifampicin (a potent inducer of the CYP3A4 isoenzyme) reduces the AUC and Cmax of tofacitinib by 84% and 74%, respectively.
The likelihood of an effect of inhibitors of the CYP2C19 isoenzyme or P-glycoprotein on the pharmacokinetics of tofacitinib is low.
Co-administration of tacrolimus (a weak inhibitor of the CYP3A4 isoenzyme) increases the AUC of tofacitinib by 21% and reduces the Cmax of tofacitinib by 9%. Co-administration of cyclosporine (a moderate inhibitor of the CYP3A4 isoenzyme) increases the AUC of tofacitinib by 73% and reduces the Cmax of tofacitinib by 17%. Concomitant repeated use of tofacitinib and potent immunosuppressants has not been studied in patients with rheumatoid arthritis.
Concomitant use with methotrexate (15-25 mg methotrexate once a week) does not affect the pharmacokinetics of tofacitinib.
Interactions in which Jaquinus affects the pharmacokinetics of other drugs
In vitro studies have shown that tofacitinib, at concentrations greater than 150 times the Cssmax achieved when used at recommended therapeutic doses, does not significantly inhibit or induce the activity of major drugs metabolized by CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6 and CYP3A4. These results were confirmed by in vitro drug interaction studies, which showed no changes in the pharmacokinetics of midazolam, a highly selective substrate of the CYP3A4 isoenzyme, when administered concomitantly with tofacitinib. In vitro data have shown that the ability of tofacitinib at therapeutic concentrations to inhibit transporters such as P-glycoprotein, organic anionic or cationic transporters is very low.
Co-administration with tofacitinib had no effect on the pharmacokinetics of oral contraceptives, levonorgestrel and ethinyl estradol in healthy women.
Concomitant use of tofacitinib with methotrexate at a dose of 15-25 mg once a week. reduced the AUC and Cmax of methotrexate by 10% and 13%, respectively. These changes in the pharmacokinetics of methotrexate did not require dose adjustment or selection of individual doses of methotrexate.
In patients with rheumatoid arthritis, tofacitinib clearance did not change over time. This indicates that tofacitinib does not affect the activity of CYP isoenzymes in patients with rheumatoid arthritis. Therefore, it is unlikely that concomitant use of CYP isoenzyme substrates with tofacitinib will result in a clinically significant increase in their metabolism in patients with rheumatoid arthritis.
Overdose
Overdose
There is no experience of overdose with the use of the drug Yaquinus. Treatment is symptomatic and supportive. In case of overdose, it is recommended to monitor the patient’s condition for the development of signs and symptoms of adverse reactions. If adverse reactions develop, appropriate therapy should be prescribed. There is no specific antidote.
Pharmacokinetic data in healthy volunteers receiving single doses of up to 100 mg indicate that about 95% of the administered dose is eliminated within 24 hours.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C
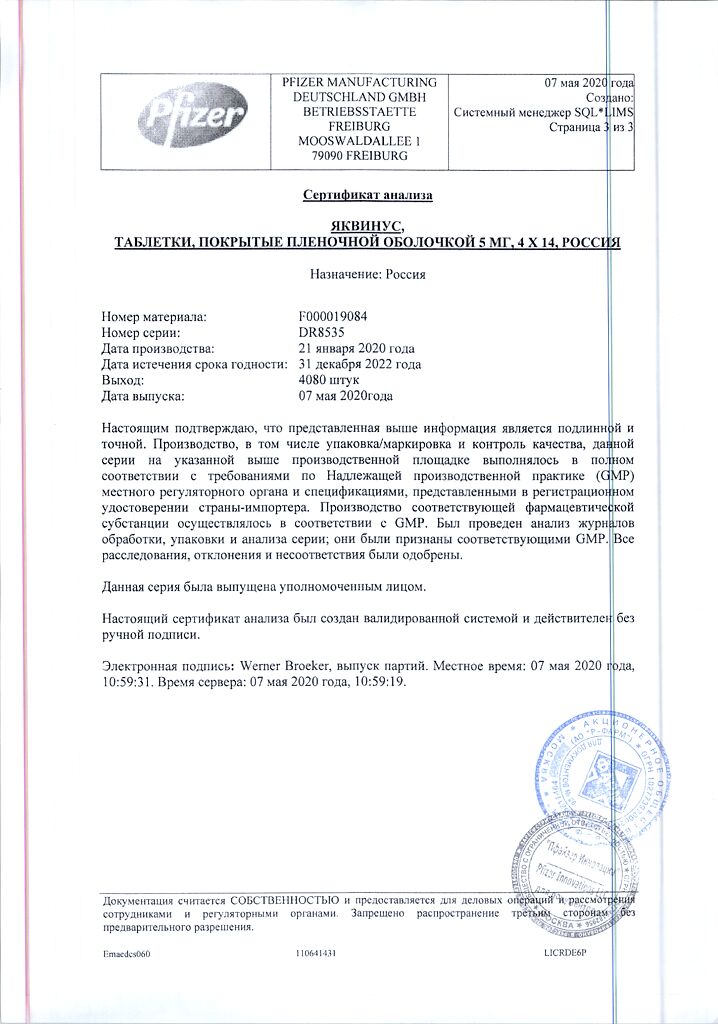
Shelf life
Shelf life
2 years
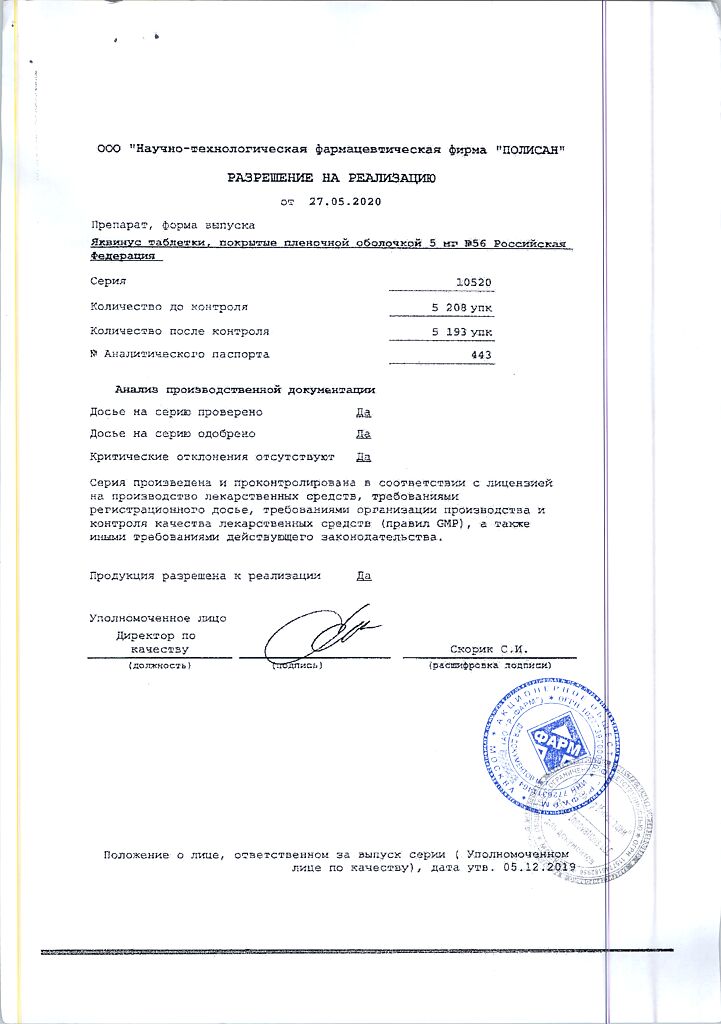
Manufacturer
Manufacturer
Polisan NTFF LLC, Russia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | Polysan NTFF LLC, Russia |
| Medication form | pills |
| Brand | Polysan NTFF LLC |
Related products
Buy Jaquinus, 5 mg 56 pcs. with delivery to USA, UK, Europe and over 120 other countries.