No products in the cart.
Hypotef, tablets 20 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Hypotef is a combination drug for the treatment of arterial hypertension in patients over 45 years of age, with less side effects than monotherapy with its constituent components due to lower doses.
Vinpocetine
A semi-synthetic derivative of the alkaloid devincan, found in the periwinkle plant; the active ingredient is the ethyl ester of apovincamic acid. Vinpocetine improves cerebral circulation, activates metabolic processes in the CNS.
Vinpocetine has a significant protective effect in relation to higher brain functions, has a pronounced cerebroprotective effect. Vinpocetine intensively and selectively increases cerebral blood flow. Pharmacological effects of the drug are realized through several mechanisms.
Vinpocetine significantly improves cerebral microcirculation, inhibits platelet aggregation, reduces increased blood viscosity. The drug has a direct effect on brain metabolism by inhibiting cycloadenosine monophosphate (cAMP), thereby inhibiting the rate of cAMP breakdown. The level of cAMP also increases as a result of the indirect effect of vinpocetine on the synthesis of cAMP through the increased levels of noradrenaline and dopamine in the brain tissue, which, in turn, increase the activity of adenylate cyclase – the catalyst of the last stage of cAMP synthesis. Vinpocetine improves hypoxia tolerance of brain cells by promoting oxygen transport to the tissues, due to the decrease of red blood cell affinity for it, increasing glucose uptake and metabolism. Glucose metabolism switches to a more energetically advantageous, aerobic direction.
The other important target of action of vinpocetine is calcium. The drug inhibits calcium entry into the intracellular space or into synaptosomes induced by depolarization and the release of intracellular calcium. Vinpocetine combines vascular and metabolic effects and promotes normalization of venous outflow against the background of decreased resistance of cerebral vessels.
Vinpocetine is prescribed orally. It should be taken for a long time, at least 2 months.
Indapamide
Indapamide is a drug that has diuretic, vasodilatory and hypotensive activity. The drug is a diuretic, a derivative of sulfonamide, which inhibits reverse sodium absorption in the cortical segment of the nephron loop and increases renal excretion of sodium, chlorine, calcium and magnesium.
Indapamide reduces the sensitivity of the vascular wall to noradrenaline and angiotensin II; stimulates the synthesis of prostaglandin E2, which has vasodilator and hypotensive effects; inhibits calcium flow into the smooth muscle cells of the vascular wall and thus reduces total peripheral vascular resistance (TPR). This mechanism leads to reduction of vasoconstriction and normalization of BP.
Indapamide is used once daily (preferably in the morning). Thiazide and thiazide-like diuretics reach a plateau of therapeutic effect at a certain dose, while the incidence of side effects continues to increase with further increasing of the drug dose.
Metoprolol acts predominantly on the beta1-adrenoreceptors of the heart and has no intrinsic sympathomimetic or membrane stabilizing activity. It reduces the stimulating effect of sympathetic innervation on the heart, has antianginal, antihypertensive, antiarrhythmic effects. It selectively blocks beta-adrenoreceptors. Reduces heart rate (HR), slows anthrioventricular (AV) conduction, reduces myocardial contractility and excitability. BP reduction occurs due to these mechanisms, as well as due to suppression of the secretion of blood renin activity. In addition, there is a decrease in pressure in the portal vein system due to the reduction of hepatic and mesenteric blood flow. The effect of metoprololol develops within 1 hour after oral administration.
Enalapril inhibits ACE, which promotes conversion of angiotensin I into angiotensin II, reduces the concentration of aldosterone in blood, increases renin release, improves functioning of kallikrein-kinin system, stimulates release of prostaglandins and endothelial relaxing factor, inhibits sympathetic nervous system. Taken together, these effects eliminate spasm and dilate peripheral arteries, reduce ROSS, systolic and diatolic BP, post- and preload on the myocardium. Dilates arteries to a greater extent than veins, and there is no reflex increase in HR.
The antihypertensive effect is more pronounced at high plasma renin concentration than at normal or reduced. Reduction of BP within therapeutic limits has no effect on the cerebral circulation. Improves blood supply to ischemic myocardium. Increases renal blood flow without changing glomerular filtration rate. In patients with initially decreased glomerular filtration its rate usually increases. Maximum effect of enalapril develops after 6-8 hours and lasts up to 24 hours after oral administration.
Hypotenef is a combined drug in which the doses of the active components are 2-4 times lower than the therapeutic doses for each component. Antihypertensive effect is achieved due to simultaneous action on most of the stages causing arterial hypertension, resulting in relaxation of vessels (enalapril, vinpocetine), reduction of fluid in the body (indapamide) and normalization of cardiac activity (metoprolol). The drug prevents an increase in the tone of the cerebral membranes, including ischemic brain damage, a condition characteristic of a very wide range of diseases, as well as in persons of advanced age. Introduction of vinpocetine in combination promotes restriction of lipid peroxidation development, maintenance of partial oxygen pressure in brain, has antiedematous effect and improves mental activity in arterial hypertension combined with cerebral ischemia.
Pharmacokinetics
Absorption
For Hypoteph, it was found that when administered orally to rabbits at a dose of 18.In rabbits at a dose of 18.5 mg/kg metoprolol is rapidly absorbed into the gastrointestinal tract, the maximal concentration (Cmax) is reached within 1.17 h with subsequent elimination of metoprolol from the blood stream. The half-life (T1/2β) is 2.15 h.
For the other components, the pharmacokinetics in combination have not been studied, but it is known that:
Vinpocetine is rapidly and completely adsorbed from the GI tract. Bioavailability is 57%. The value of therapeutic concentration of vinpocetine in blood plasma is from 10 to 20 ng/ml;
– indapamide is quickly and completely adsorbed from the GI tract. Bioavailability is high (93%). Cmax of indapamide is created 1-2 hours after oral administration. In blood plasma it is 71-79% bound to blood proteins, can also be sorbed by erythrocytes;
– enalapril – about 60% of enalapril is adsorbed from the GI tract. The volume of absorption is 60%. Cmax in blood serum is reached 3-4 hours after intake, equilibrium concentration – after 4 days. Decrease of BP appears 1 hour after intake, reaches its maximum by 6 hours and lasts for 1 day.
Distribution
The distribution in combination has not been studied.
Vinpocetine readily passes through histohematic barriers (including the BBB, placental), penetrates into breast milk.
– indapamide has a high volume of distribution, passes through the histohematic (including the placental) barriers, penetrates into the breast milk.
– metoprolol passes through the BBB and the placental barrier, penetrates into breast milk.
– enalapril easily passes through the histohematic barriers, excluding the HEB, penetrates the placental barrier.
Metabolism
Metabolism in combination has not been studied.
– Vinpocetine is extensively metabolized in the body, the main metabolites being apovincamic acid and hydroxyvinpocetine.
Indapamide is almost completely metabolized in the liver. The only pharmacologically active metabolite is formed by hydrolysis of the indole ring.
– metoprolol is extensively biotransformed in the liver to form the metabolites – o-desmethylmetoprolol and α-hydroxymetoprolol.
Enalapril undergoes biotransformation in the liver to form the metabolite enalaprilat with Cmax determined after 4 hours.
Elevation
Elevation in combination has not been studied.
Vinpocetine’s T1/2 is about 5 h. Most of vinpocetine is excreted by the kidneys as metabolites. Only a few percent of the drug is excreted unchanged.
Indapamide T1/2 is about 14 hours. Up to 80% is excreted by the kidneys as inactive metabolites and 20% – through the intestine.
– metoprolol – T1/2 is 2.15 h. It is excreted by the kidneys mainly as metabolites, about 3% – unchanged.
– Enalapril – T1/2 is 11 h. Excreted mainly by the kidneys (up to 40% is excreted as enalaprilate). Within 24 h up to 90% of the administered amount is excreted.
Indications
Indications
Arterial hypertension of 1st and 2nd severity in patients over 45 years of age.
Pharmacological effect
Pharmacological effect
Hypotef is a combination drug for the treatment of arterial hypertension in patients over 45 years of age, which has less pronounced side effects than monotherapy with its components due to lower doses.
Vinpocetine
A semi-synthetic derivative of the alkaloid devincane contained in the periwinkle plant; active substance – ethyl ester of apovincamic acid. Vinpocetine improves cerebral circulation and activates metabolic processes in the central nervous system.
Vinpocetine has a significant protective effect on higher brain functions and has a pronounced cerebroprotective effect. Vinpocetine intensively and selectively increases cerebral blood flow. The pharmacological effects of the drug are realized through several mechanisms.
Vinpocetine significantly improves cerebral microcirculation, inhibits platelet aggregation, and reduces increased blood viscosity. The drug has a direct effect on brain metabolism, inhibiting cycloadenosine monophosphate (cAMP), thereby inhibiting the rate of cAMP breakdown. The level of cAMP also increases as a result of the indirect effect of vinpocetine on the synthesis of cAMP through an increase in the level of norepinephrine and dopamine in the brain tissue, which, in turn, enhance the activity of adenylate cyclase, the catalyst for the last stage of cAMP synthesis. Vinpocetine improves the tolerance of hypoxia by brain cells, promoting the transport of oxygen to tissues, due to a decrease in the affinity of red blood cells for it, increasing the absorption and metabolism of glucose. Glucose metabolism switches to an energetically more favorable, aerobic direction.
Another important target of action of vinpocetine is calcium. The drug inhibits the entry of calcium into the intracellular space or into synaptosomes induced by depolarization and the release of intracellular calcium. Vinpocetine combines vascular and metabolic effects and helps normalize venous outflow while reducing cerebral vascular resistance.
Vinpocetine is prescribed orally. The drug is taken for a long time, at least 2 months.
Indapamide
Indapamide is a drug with diuretic, vasodilating and hypotensive activity. The drug is a diuretic, a sulfonamide derivative, which inhibits the reverse absorption of sodium in the cortical segment of the nephron loop, increases the excretion of sodium, chlorine, calcium and magnesium by the kidneys.
Indapamide reduces the sensitivity of the vascular wall to norepinephrine and angiotensin II; stimulates the synthesis of prostaglandin E2, which has vasodilating and hypotensive effects; inhibits the flow of calcium into the smooth muscle cells of the vascular wall and, thus, reduces total peripheral vascular resistance (TPVR). This mechanism leads to a decrease in vasoconstriction and normalization of blood pressure.
Indapamide is used once a day (preferably in the morning). Thiazide and thiazide-like diuretics at a certain dose reach a plateau of therapeutic effect, while the frequency of side effects continues to increase with further increases in the dose of the drug.
Metoprolol acts predominantly on beta1-adrenergic receptors of the heart and does not have internal sympathomimetic and membrane-stabilizing activity. Reduces the stimulating effect of sympathetic innervation on the heart, has antianginal, antihypertensive, and antiarrhythmic effects. Selectively blocks beta-adrenergic receptors. Reduces heart rate (HR), slows down atrioventricular (AV) conduction, reduces myocardial contractility and excitability. A decrease in blood pressure occurs due to these mechanisms, as well as due to the suppression of the secretion of blood renin activity. In addition, there is a decrease in pressure in the portal vein system due to a decrease in hepatic and mesenteric blood flow. The effect of metoprolol develops 1 hour after oral administration.
Enalapril inhibits ACE, which promotes the conversion of angiotensin I to angiotensin II, reduces the concentration of aldosterone in the blood, increases the release of renin, improves the functioning of the kallikrein-kinin system, stimulates the release of prostaglandins and endothelial relaxing factor, and inhibits the sympathetic nervous system. Together, these effects eliminate spasm and dilate peripheral arteries, reduce peripheral vascular resistance, systolic and diatolic blood pressure, and post- and preload on the myocardium. It dilates arteries to a greater extent than veins, but there is no reflex increase in heart rate.
The antihypertensive effect is more pronounced with high plasma renin concentrations than with normal or reduced ones. Reducing blood pressure within therapeutic limits does not affect cerebral circulation. Improves blood supply to ischemic myocardium. Increases renal blood flow, while the glomerular filtration rate does not change. In patients with initially reduced glomerular filtration rate, its rate usually increases. The maximum effect of enalapril develops within 6-8 hours and lasts up to 24 hours after oral administration.
Hypotef is a combination drug, the doses of the active components in which are 2-4 times lower than the therapeutic doses for each component. The antihypertensive effect is achieved through simultaneous action on most of the stages that cause the development of arterial hypertension, leading to vascular relaxation (enalapril, vinpocetine), a decrease in the amount of fluid in the body (indapamide) and normalization of cardiac activity (metoprolol). The drug prevents an increase in the tone of the meninges, including in cases of ischemic brain damage – a condition characteristic of a very wide range of diseases, as well as for the elderly. The introduction of vinpocetine into the combination helps limit the development of lipid peroxidation, maintain the partial pressure of oxygen in the brain, has an anti-edematous effect and improves mental activity in arterial hypertension in combination with cerebral ischemia.
Pharmacokinetics
Suction
For the drug Hypotef, it has been established that when administered orally to rabbits at a dose of 18.5 mg/kg, metoprolol is rapidly absorbed in the gastrointestinal tract, the maximum concentration (Cmax) is reached within 1.17 hours, followed by the removal of metoprolol from the bloodstream, the half-life (T1/2β) is 2.15 hours.
For the remaining components, the pharmacokinetics in combination have not been studied, but it is known that:
— Vinpocetine is quickly and completely absorbed from the gastrointestinal tract. Bioavailability is 57%. The therapeutic concentration of vinpocetine in blood plasma ranges from 10 to 20 ng/ml;
— indapamide is quickly and completely adsorbed from the gastrointestinal tract. Bioavailability is high (93%). Cmax of indapamide occurs 1-2 hours after oral administration. In blood plasma, it is 71-79% bound to blood proteins and can also be absorbed by erythrocytes;
— enalapril – about 60% of enalapril is adsorbed from the gastrointestinal tract. The suction volume is 60%. Cmax in blood serum is achieved 3-4 hours after administration, equilibrium concentration is achieved after 4 days. A decrease in blood pressure appears 1 hour after administration, reaches a maximum at 6 hours and continues for 1 day.
Distribution
The distribution in the combination has not been studied.
— vinpocetine easily passes through histohematic barriers (including the BBB, placental), penetrates into breast milk.
— indapamide has a high volume of distribution, passes through histohematic (including placental) barriers, and penetrates into breast milk.
— metoprolol passes through the blood-brain barrier and the placental barrier and passes into breast milk.
— enalapril easily passes through histohematic barriers, excluding the BBB, and penetrates the placental barrier.
Metabolism
Metabolism in combination has not been studied.
— vinpocetine is intensively metabolized in the body, the main metabolites being apovincamic acid and hydroxyvinpocetine.
– indapamide is almost completely metabolized in the liver. The only pharmacologically active metabolite is formed as a result of hydrolysis of the indole ring.
— metoprolol is intensively biotransformed in the liver with the formation of metabolites – o-desmethylmetoprolol and α-hydroxymetoprolol.
– enalapril undergoes biotransformation in the liver with the formation of a metabolite – enalaprilat, the Cmax of which is determined after 4 hours.
Removal
Excretion in combination has not been studied.
— vinpocetine T1/2 – about 5 hours. Most of vinpocetine is excreted by the kidneys in the form of metabolites. Only a few percent of the drug is excreted unchanged.
– indapamide T1/2 – about 14 hours. Up to 80% is excreted by the kidneys in the form of inactive metabolites and 20% through the intestines.
— metoprolol – T1/2 is 2.15 hours. It is excreted by the kidneys mainly in the form of metabolites, about 3% unchanged.
— enalapril – T1/2 is 11 hours. It is excreted mainly by the kidneys (up to 40% is excreted in the form of enalaprilat). Within 24 hours, up to 90% of the administered amount is excreted.
Active ingredient
Active ingredient
Vinpocetine, Indapamide, Metoprolol, Enalapril
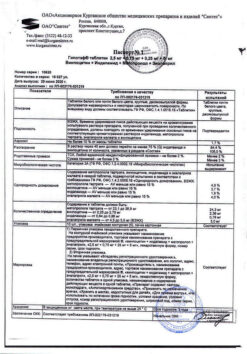
Composition
Composition
Active ingredients:
vinpocetine 2.5 mg;
indapamide0.75 mg;
metoprolol tartrate 25 mg;
enalapril maleate 5 mg;
Excipients:
hypromellose -15 thousand (hydroxypropyl methylcellulose 15) – 5.05 mg,
stearic acid – 2 mg,
copovidone (kollidon VA64, kollidon BA64) – 5 mg,
croscarmellose sodium (primellose) – 12 mg,
colloidal silicon dioxide (Aerosil) – 2 mg,
lactose monohydrate (milk sugar, lactose 80) – 45 mg,
microcrystalline cellulose – up to tablet weight 200 mg
Pregnancy
Pregnancy
The use of Hypotef during pregnancy is contraindicated. The active components of the drug Hypotef: metoprolol, enalapril, vinpocetine pass through the placental barrier and penetrate into breast milk.
If it is necessary to use the drug Hypotef during lactation, it is recommended to discontinue breastfeeding.
Contraindications
Contraindications
Vinpocetine
hypersensitivity to vinpocetine;
acute phase of hemorrhagic stroke, severe ischemic heart disease, severe cardiac arrhythmias;
pregnancy, breastfeeding period;
age up to 18 years.
Metoprolol
hypersensitivity to metoprolol;
cardiogenic shock;
AV block II and III degrees (without artificial pacemaker);
sinoatrial blockade, sick sinus syndrome, severe bradycardia (heart rate less than 50 beats/min), severe peripheral circulatory disorders, heart failure in the stage of decompensation;
bronchial hyperreactivity (for example, in severe bronchial asthma in patients receiving continuous or intermittent therapy with inotropic drugs acting on beta-adrenergic receptors, COPD in the acute stage);
Prinzmetal’s angina;
arterial hypotension (if used for secondary prevention of myocardial infarction – systolic blood pressure less than 100 mm Hg);
if acute myocardial infarction is suspected (heart rate less than 45 beats/min, PQ interval more than 0.24 seconds or systolic blood pressure less than 100 mm Hg);
pheochromocytoma (without simultaneous use of alpha-blockers);
simultaneous use of monoamine oxidase inhibitors (MAO);
breastfeeding period;
age under 18 years (efficacy and safety have not been established).
Indapamide
hypersensitivity to indapamide and other sulfonamide derivatives;
severe renal impairment (creatinine clearance less than 30 ml/min) and/or liver (including encephalopathy);
hypokalemia;
pregnancy, breastfeeding period;
age up to 18 years.
Enalapril
hypersensitivity to enalapril and other ACE inhibitors;
history of angioedema (Quincke’s edema) associated with taking an ACE inhibitor;
hereditary/idiopathic angioedema;
simultaneous use with aliskiren;
pregnancy, breastfeeding period;
age under 18 years (efficacy and safety have not been established).
Hypotef
hypersensitivity to the excipients included in the drug;
lactose intolerance, lactase deficiency and glucose-galactose malabsorption syndrome;
use in patients under 45 (efficacy and safety have not been established).
With caution
Vinpocetine
When used simultaneously with other antihypertensive drugs or drugs that prolong the QT interval, impaired liver function, poor tolerance to Vinca minor alkaloids.
Indapamide
Diabetes mellitus, hyperuricemia (especially accompanied by gout and urate nephrolithiasis), hyponatremia and other water-electrolyte imbalances, moderate hepatic and/or renal failure, ascites, ischemic heart disease, chronic heart failure, concomitant use of drugs that prolong the QT interval, hyperparathyroidism, in weakened patients with an increased QT interval on the ECG or receiving combined therapy with other antiarrhythmic drugs.
Metoprolol
Diabetes mellitus, metabolic acidosis, impaired liver and/or renal function (creatinine clearance less than 40 ml/min), myasthenia gravis, 1st degree AV block, thyrotoxicosis, depression (including history), psoriasis, history of allergic reactions (possible increased sensitivity to allergens, worsening arterial hypertension and decreased therapeutic response to adrenaline), bronchial asthma, COPD, pulmonary emphysema, chronic obstructive bronchitis, obliterating peripheral vascular diseases (intermittent claudication, Raynaud’s syndrome), old age (over 60 years).
Enalapril
Systemic connective tissue diseases (including systemic lupus erythematosus, scleroderma), immunosuppressant therapy (risk of developing neutropenia, agranulocytosis), inhibition of bone marrow hematopoiesis, reduced circulating blood volume (taking diuretics, salt-free diet, vomiting, diarrhea), coronary heart disease, cerebrovascular diseases, renovascular hypertension, diabetes diabetes, chronic heart failure (functional class IV according to the NYHA classification), old age (over 60 years); hemodialysis using high-flux membranes (for example, AN69) or desensitization, low-density lipoprotein (LDL) apheresis, renal artery stenosis (including bilateral), condition after kidney transplantation; Aortic valve stenosis/hypertrophic cardiomyopathy, hyperkalemia.
Side Effects
Side Effects
Vinpocetine
From the nervous system and sensory organs: rarely – dizziness, headache, insomnia, drowsiness, weakness.
From the cardiovascular system: rarely – slowing of intraventricular conduction, depression of the ST segment and prolongation of the QT interval, marked decrease in blood pressure, tachycardia, extrasystole.
From the gastrointestinal tract: rarely – dryness of the oral mucosa, nausea, heartburn.
From the skin: rarely – increased sweating, allergic reactions.
Indapamide
Most adverse reactions are dose-dependent.
From the cardiovascular system: very rarely – a pronounced decrease in blood pressure; unspecified frequency – pirouette-type arrhythmia (possibly fatal).
From the hematopoietic organs: very rarely – thrombocytopenia, leukopenia, aplastic anemia, hemolytic anemia, hemolytic anemia.
From the urinary system: very rarely – renal failure.
From the digestive system: infrequently – vomiting; rarely – nausea, constipation, dryness of the oral mucosa; very rarely – pancreatitis, liver dysfunction; unspecified frequency – the possibility of developing hepatic encephalopathy in case of liver failure, hepatitis.
From the skin:
Hypersensitivity reactions, mainly dermatological, in patients with a predisposition to allergic reactions: often – maculopapular rash; uncommon – hemorrhagic vasculitis; very rarely – angioedema and/or urticaria, Stevens-Johnson syndrome, toxic epidermal necrolysis; unspecified frequency – hyponatremia, accompanied by hypovolemia, leading to dehydration and orthostatic hypotension; simultaneous hypochloremia can lead to metabolic alkalosis – in patients with an acute form of systemic lupus erythematosus, the course of the disease may worsen.
Cases of photosensitivity reactions have been described.
Laboratory indicators: very rarely – hypercalcemia; unspecified frequency – an increase in the QT interval on the ECG, an increase in the concentration of uric acid and glucose in the blood, an increase in the activity of liver transaminases, a decrease in potassium levels and the development of hypokalemia, especially significant for patients belonging to the compensatory group (the likelihood and severity of this effect is low).
Metoprolol
From the hematopoietic organs: very rarely – thrombocytopenia, leukopenia.
From the cardiovascular system: often – sinus bradycardia, postural disturbances (very rarely accompanied by fainting), “coldness” of the extremities, palpitations; infrequently – temporary increase in symptoms of heart failure, AV block of the first degree; cardiogenic shock in patients with acute myocardial infarction, peripheral edema, pain in the heart area; rarely – gangrene in patients with previous severe peripheral circulatory disorders.
From the nervous system: very often – increased fatigue; often – headache, dizziness; uncommon – parasthesia, convulsions, depression, decreased concentration, drowsiness or insomnia, nightmares; rarely – increased nervous excitability, anxiety, impotence/sexual dysfunction, Peyronie’s disease; very rarely – amnesia/hearing impairment and tinnitus.
From the senses: rarely – visual impairment, dryness and/or irritation of the eyes, conjunctivitis, hearing loss and tinnitus.
From the digestive system: often – nausea, abdominal pain, diarrhea, constipation; infrequently – vomiting; rarely – dryness of the oral mucosa; very rarely – disturbance of taste.
From the liver: rarely – liver dysfunction, increased activity of liver transaminases; very rarely – hepatitis.
From the skin: infrequently – urticaria, increased sweating; rarely – alopecia; very rarely – photosensitivity, exacerbation of symptoms of thyrotoxicosis.
From the respiratory system: often – shortness of breath with physical effort; infrequently – bronchospasm; rarely – rhinitis.
From the endocrine system: rarely – hypo-, hyperglycemia in patients with type I diabetes mellitus, masking the symptoms of thyrotoxicosis.
From the musculoskeletal system: very rarely – arthralgia.
From the side of metabolism: infrequently – weight gain; rarely – aggravation of latent diabetes mellitus.
Laboratory indicators: very rarely – a decrease in the concentration of high-density cholesterol and an increase in triglycerides in the blood plasma.
Enalapril
From the hematopoietic and lymphatic systems: rarely – decrease in hemoglobin and hematocrit; very rarely – suppression of bone marrow function, anemia, thrombocytopenia, leukopenia, neutropenia and agranulocytosis, hemolytic anemia, lymphadenopathy, eosinophilia, autoimmune diseases.
From the endocrine system: rarely – syndrome of inadequate secretion of antidiuretic hormone.
From the side of the central nervous system: often – headache, dizziness, fainting; infrequently – insomnia, anxiety, panic, confusion, depression, sleep disturbances, nightmares, drowsiness; rarely – parasthesia, memory impairment, peripheral neuropathy, tremor, migraine, confusion.
From the organ of vision: rarely – visual impairment, conjunctivitis, decreased visual acuity, dryness and burning of the eyes.
From the organ of hearing: infrequently – vertigo, tinnitus.
From the cardiovascular system: often – marked decrease in blood pressure, orthostatic hypotension; uncommon – palpitations, chest pain, arrhythmias (atrial fibrillation, sinus bradycardia, tachycardia, ventricular fibrillation), angina pectoris, 2nd degree AV block, cerebrovascular accident, myocardial infarction.
From the respiratory system: often – cough; infrequently – rhinitis, nasal congestion; very rarely – sinusitis, pharyngitis, laryngitis, sore throat, hoarseness, shortness of breath, bronchitis, pulmonary infiltrates, bronchospasm/bronchial asthma.
From the digestive system: often – nausea, diarrhea; infrequently – abdominal pain, constipation; rarely – dryness of the oral mucosa, stomatitis, flatulence, vomiting, gastritis, taste disturbance, peptic ulcer, aphthous ulcers; very rarely – pancreatitis, intestinal obstruction, intestinal angioedema.
From the liver and biliary tract: infrequently – increased activity of liver transaminases, increased bilirubin concentration; very rarely – liver dysfunction, hepatocellular or cholestatic hepatitis, jaundice.
Allergic reactions: infrequently – skin rash, itching; rarely – angioedema of the face, limbs, lips, tongue, vocal folds and/or larynx, dysphonia, urticaria; very rarely – toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme, photosensitivity.
From the skin: rarely – alopecia, psoriasis, dermatitis, dry skin; very rarely – pseudolymphoma, pemphigus.
From the genitourinary system: often – impaired renal function; rarely – uremia, acute renal failure, proteinuria; very rarely – oliguria, anuria.
From the musculoskeletal system: often – muscle spasms, back pain, leg pain, myalgia; uncommon – pain in the arms, arthralgia, musculoskeletal pain, stiffness and swelling of the joints.
From the reproductive system: infrequently – impotence; rarely – gynecomastia.
Other: often – asthenia, fatigue, hyperkalemia; infrequently – increased body temperature, slight increase in the concentration of urea and creatinine; rarely – hyperglycemia, nosebleeds, vasculitis, Raynaud’s syndrome, flushes of blood to the facial skin. A symptom complex has been described that may include fever, myalgia and arthralgia, serositis, vasculitis, increased erythrocyte sedimentation rate, leukocytosis and eosinophilia, skin rash, and a positive test for antinuclear antibodies.
Interaction
Interaction
Vinpocetine
It is possible to enhance the antihypertensive effect when used simultaneously with methyldopa (blood pressure monitoring is necessary). Despite the lack of data confirming the possibility of interaction, caution is recommended during simultaneous use with antiarrhythmics and anticoagulants.
Indapamide
Not recommended combination of drugs
With the simultaneous use of indapamide and lithium preparations, an increase in the concentration of lithium in the blood plasma is possible, accompanied by the appearance of signs of overdose (due to a decrease in lithium excretion). If it is necessary to use this combination, the concentration of lithium in the blood plasma should be monitored.
Combination of drugs requiring special attention
Drugs that can cause pirouette-type arrhythmia:
– class IA antiarrhythmic drugs (quinidine, hydroquinidine, disopyramide);
– Class III antiarrhythmic drugs (amiodarone, dofetilide, ibutilide) and sotalol;
– some neuroleptics: phenothiazines (chlorpromazine, cyamemazine, levopromazine, thioridazine, triftoperazine), benzamides (amisulpride, sulpiride, sultopride, tiapride), butyrophenones (droperidol, haloperidol);
– others: bepridil, cisapride, difemanil, erythromycin (iv), halofantrine, mizolastine, pentamidine, sparfloxacin, moxifloxacin, astemizole, vincamine (iv).
Increased risk of ventricular arrhythmias, especially pirouette-type arrhythmias (risk factor – hypokalemia).
It is necessary to monitor the potassium content in the blood plasma and, if necessary, adjust it before starting combination therapy with indapamide and the above drugs. It is necessary to monitor the patient’s clinical condition, the content of blood plasma electrolytes, and an ECG.
NSAIDs (for systemic use), including selective COX-2 inhibitors, high doses of salicylates (≥3 g/day):
– the antihypertensive effect of indapamide may be reduced;
– with significant fluid loss, acute renal failure may develop (due to a decrease in glomerular filtration rate). Patients need to compensate for fluid loss and regularly monitor kidney function, both at the beginning of treatment and during therapy.
ACE inhibitors:
The use of ACE inhibitors in patients with hyponatremia in the blood (especially in patients with renal artery stenosis) is accompanied by the risk of sudden arterial hypotension and/or acute renal failure.
Patients with arterial hypertension and possibly reduced sodium levels in the blood plasma due to diuretics should:
– 3 days before starting treatment with an ACE inhibitor, stop taking diuretics. In the future, if necessary, diuretics can be resumed;
– or start ACE inhibitor therapy with low doses, followed by a gradual increase in dose if necessary.
In chronic heart failure, treatment with ACE inhibitors should begin with low doses with a possible preliminary reduction in the doses of diuretics.
In all cases, in the first week of taking ACE inhibitors in patients, it is necessary to monitor renal function (plasma creatinine concentration).
Other drugs that can cause hypokalemia: amphotericin B (iv), gluco- and mineralcorticoids (when used systemically), tetracosactide, laxatives that stimulate intestinal motility.
Increased risk of hypokalemia (additive effect).
Regular monitoring of the potassium content in the blood plasma is necessary, and, if necessary, its correction. Particular attention should be paid to patients concomitantly receiving cardiac glycosides. It is recommended to use laxatives that do not stimulate intestinal motility.
– Baclofen:
There is an increase in the antihypertensive effect.
Patients need to compensate for fluid loss and carefully monitor renal function at the beginning of treatment.
– cardiac glycosides:
Hypokalemia enhances the toxic effect of cardiac glycosides.
With the simultaneous use of indapamide and cardiac cligosides, the potassium content in the blood plasma, ECG should be monitored, and, if necessary, therapy should be adjusted.
Drug combination requiring attention
– potassium-sparing diuretics (amiloride, spironolactone, triamterene):
Combination therapy with indapamide and potassium-sparing diuretics is advisable in some patients, but the possibility of developing hypokalemia (especially in patients with diabetes mellitus and patients with renal failure) or hyperkalemia cannot be excluded.
It is necessary to monitor potassium levels in the blood plasma, ECG indicators and, if necessary, adjust therapy.
– metformin:
Functional renal failure, which can occur against the background of diuretics, especially loop diuretics, with simultaneous administration of metformin increases the risk of developing lactic acidosis.
Metformin should not be taken if the creatinine concentration exceeds 15 mg/g (135 µmol/L) in men and 12 mg/g (100 µmol/L) in women.
– iodine-containing contrast agents:
Dehydration while taking diuretics increases the risk of developing acute renal failure, especially when using high doses of iodinated contrast agents.
Before using iodinated contrast agents, patients must compensate for fluid loss.
– tricyclic antidepressants, antipsychotics (neuroleptics):
Drugs in these classes enhance the antihypertensive effect of indapamide and increase the risk of orthostatic hypotension (additive effect).
– calcium salts:
With simultaneous administration, hypercalcemia may develop due to a decrease in the excretion of calcium ions by the kidneys.
– cyclosporine, tacrolimus:
It is possible to increase the concentration of creatinine in the blood plasma without changing the concentration of circulating cyclosporine, even with normal fluid and sodium ion levels.
– corticosteroid drugs (mineral and glucocorticosteroids), tetracosactide (if administered systemically):
Decreased antihypertensive effect (retention of fluid and sodium ions as a result of the action of corticosteroids).
Metoprolol
Concomitant use with MAO inhibitors is not recommended due to a significant increase in antihypertensive effect. The treatment break between taking MAO inhibitors and metoprolol should be at least 14 days.
Beta-blockers, theophylline, cocaine, estrogens (sodium retention), indomethacin and other NSAIDs (sodium retention and blocking renal prostaglandin synthesis) weaken the antihypertensive effect of metoprolol.
When used simultaneously with hypoglycemic agents for oral administration, their effect may be reduced; with insulin – increasing the risk of developing hypoglycemia, increasing its severity and duration, masking some symptoms of hypoglycemia (tachycardia, increased sweating, increased blood pressure).
When used simultaneously with antihypertensive drugs, diuretics, ACE inhibitors, nitroglycerin or blockers of “slow” calcium channels, a sharp decrease in blood pressure may develop (special caution is required when combined with prazosin); the risk of bradycardia increases when combined with epinephrine; a pronounced decrease in heart rate and inhibition of AV conduction up to complete blockade – when using metoprolol with verapamil, diltiazem, reserpine, methyldopa, clonidine, guanfacine and cardiac glycosides, agents for general anesthesia (along with cardiodepressive and antihypertensive effects).
Simultaneous intravenous administration of verapamil can provoke cardiac arrest.
Drugs that induce or inhibit the CYP2D6 isoenzyme may affect the plasma concentration of metoprolol. The concentration of metoprolol in the blood plasma may increase when taken concomitantly with other drugs that are substrates for CYP2D6, for example, antiarrhythmic drugs, antihistamines, H2 receptor antagonists, antidepressants (selective neuronal serotonin reuptake inhibitors, for example, paroxetine, fluoxetine, sertraline), antipsychotics and COX-2 inhibitors.
Class I antiarrhythmic drugs can lead to additive negative inotropic effects with the development of severe hemodynamic side effects in patients with impaired left ventricular function (this combination should be avoided in patients with sick sinus syndrome and impaired AV conduction). Quinidine inhibits the metabolism of metoprolol in patients with “fast” metabolism, leading to a significant increase in the concentration of metoprolol in the blood plasma and an increase in its beta-blocking effect.
Combination with amiodarone increases the risk of developing severe sinus bradycardia (including for a long time after discontinuation of amiodarone, due to its long half-life).
If metoprolol and clonidine are taken simultaneously, then when metoprolol is discontinued, clonidine is discontinued after a few days (due to the risk of withdrawal syndrome).
Inducers of microsomal liver enzymes (rifampicin, barbiturates) lead to increased metabolism and a decrease in effect. Inhibitors (cimetidine, oral contraceptives, phenothiazines) – increase the concentration of metoprolol in the blood plasma.
Diphenhydramine reduces the clearance of metoprolol, enhancing its effect.
Simultaneous use with high doses of phenylpropanolamine can lead to a paradoxical increase in blood pressure (up to a hypertensive crisis).
Allergens used for immunotherapy or allergen extracts for skin testing when used in combination with metoprolol increase the risk of systemic allergic reactions or anaphylaxis; iodine-containing radiocontrast agents for intravenous administration increase the risk of anaphylactic reactions.
Reduces the clearance of xanthines (except diphylline), especially in patients with initially increased clearance of theophylline under the influence of smoking. Reduces the clearance of lidocaine, increases the concentration of lidocaine in the blood plasma.
Strengthens and prolongs the effect of antidepolarizing muscle relaxants; prolongs the anticoagulant effect of coumarins.
When used together with anxiolytics and drugs with hypnotic activity, the antihypertensive effect is enhanced; with ethanol, the risk of a pronounced decrease in blood pressure increases and the inhibitory effect on the central nervous system increases.
There is an increased risk of peripheral circulatory disorders with ergot alkaloids.
Enalapril
Concomitant use is not recommended
– potassium-sparing diuretics (spironalactone, eplerenone, triamterene, amiloride) or potassium-containing salts, potassium supplements: when used simultaneously with ACE inhibitors, hyperkalemia may develop. If, due to diagnosed hypokalemia, the simultaneous use of these drugs is still indicated, they should be used with caution, with regular monitoring of potassium levels in the blood serum and electrocardiogram.
Concomitant use with caution
– thiazide or loop diuretics: previous treatment with diuretics in high doses may, at the beginning of enalapril therapy, lead to a decrease in blood volume and contribute to the development of arterial hypotension. The antihypertensive effect can be reduced by stopping the diuretic, increasing fluid or salt intake, or starting therapy with low doses of enalapril;
– drugs for general anesthesia: when used with ACE inhibitors, they can lead to worsening orthostatic hypotension;
– narcotic drugs/tricyclic antidepressants/psychotropic drugs/barbiturates: development of orthostatic hypotension may occur;
– other antihypertensive drugs (alpha- and beta-blockers, slow calcium channel blockers): the antihypertensive effect can be additive or potentiated. Caution is required when treating with nitroglycerin in various dosage forms and other nitrates or other vasodilators;
– cimetidine: increased risk of collapse;
– cyclosporine: when used simultaneously with ACE inhibitors, the risk of developing renal dysfunction increases;
– allopurinol, procainamide, cytostatics or immunosuppressants: when used simultaneously with ACE inhibitors, the risk of developing hypersensitivity reactions and leukopenia increases;
– hypoglycemic agents: in rare cases, ACE inhibitors may enhance the hypoglycemic effect of insulin and oral hypoglycemic agents (for example, sulfonylureas) in patients with diabetes mellitus. In these cases, with simultaneous use of ACE inhibitors, it may be necessary to reduce the dose of the hypoglycemic agent;
– Sympathomimetics may antagonize the antihypertensive effect of ACE inhibitors. To confirm the antihypertensive effect, such patients should be under close medical supervision;
– anatcides reduce the bioavailability of ACE inhibitors when used simultaneously;
– when used simultaneously with the drug gold (sodium aurothiomalate) for intravenous administration, patients experienced: “flushes” of blood to the facial skin, nausea, vomiting, as well as arterial hypotension. Arterial hypotension can be regarded as an increase in the effect of ACE inhibitors under the influence of the gold drug.
Dual blockade of the renin-angiotensin-aldosterone system (RAAS)
It has been reported in the literature that blockade of the RAAS in patients with an established diagnosis of atherosclerosis, heart failure, or diabetes mellitus with target organ damage is associated with a higher incidence of arterial hypotension, syncope, hyperkalemia and renal dysfunction (including the development of acute renal failure) compared with the use of single-component blockade of the RAAS. The use of dual blockade of the RAAS (for example, by simultaneous use of an ACE inhibitor with an angiotensin II receptor antagonist) should be decided on a case-by-case basis with careful monitoring of renal function.
Overdose
Overdose
Vinpocetine
There is no information about overdose.
Treatment: gastric lavage, taking activated carbon; symptomatic treatment.
Indapamide
Symptoms: possible disturbances in water-electrolyte balance (hyponatremia, hypokalemia), nausea, vomiting, marked decrease in blood pressure, convulsions, dizziness, drowsiness, confusion, polyuria or oliguria leading to anuria (due to hopivolemia).
Treatment: urgent measures aimed at removing the drug from the body: gastric lavage and/or administration of activated charcoal followed by restoration of water and electrolyte balance, symptomatic therapy. There is no specific antidote.
Metoprolol
Symptoms: severe sinus bradycardia, dizziness, nausea, vomiting, cyanosis, marked decrease in blood pressure, arrhythmia, ventricular extrasystole, bronchospasm, fainting, in case of acute overdose – cardiogenic shock, loss of consciousness, coma, AV block (up to the development of complete transverse block and cardiac arrest), cardialgia, hypoglycemia, hyperkalemia, convulsions, respiratory arrest.
Signs of overdose appear 20 minutes-2 hours after taking the drug.
Treatment: gastric lavage and administration of adsorbents; symptomatic therapy: with a pronounced decrease in blood pressure, the patient should be in the Trendelenburg position; in case of excessive decrease in blood pressure, bradycardia and heart failure – intravenously (i.v.), with an interval of 2-5 minutes, beta-adrenergic agonists – until the desired effect is achieved or i.v. 0.5-2 mg of atropine. If there is no positive effect, dopamine, dobutamine or norepinephrine (norepinephrine).
As a follow-up measure, it is possible to install an artificial pacemaker. For bronchospasm, beta2-agonists should be administered intravenously. Metoprolol is poorly excreted by hemodialysis.
Enalapril
Symptoms: increased diuresis, marked decrease in blood pressure with bradycardia or other heart rhythm disturbances, convulsions, disturbances of consciousness (including coma), acute renal failure, disturbances in the acid-base state and water-electrolyte balance of the blood.
Treatment: gastric lavage and ingestion of activated carbon; in more serious cases, transfer the patient to a horizontal position with raised legs, then carry out measures aimed at stabilizing blood pressure – intravenous administration of plasma expanders, infusion of 0.9% sodium chloride solution. The patient must monitor blood pressure, heart rate, respiratory rate, serum concentration of urea, creatinine, electrolytes and diuresis, and, if necessary, hemodialysis (enalaprilat excretion rate – 62 ml/min).
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 °C
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
Sintez, Russia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C |
| Manufacturer | Sintez OAO, Russia |
| Medication form | pills |
| Brand | Sintez OAO |
Other forms…
Related products
Buy Hypotef, tablets 20 pcs with delivery to USA, UK, Europe and over 120 other countries.