No products in the cart.
Heparin sodium,. 5000 units/ml 5 ml 5 pcs
€45.75 €38.13
Description
Pharmacotherapeutic group
Direct acting anticoagulant
ATCode
B01AB01
Pharmacodynamics:
The mechanism of action of sodium heparin is based primarily on its binding to antithrombin III, which is a natural inhibitor of activated clotting factors-IIa (thrombin) IXa Ha XIa and XIIa. Sodium heparin binds to antithrombin III and causes conformational changes in its molecule. As a result, the binding of antithrombin III with clotting factors IIa (thrombin) IXa Ha XIa and XIIa is accelerated and their enzymatic activity is blocked. The binding of sodium heparin with antithrombin III is electrostatic in nature and depends largely on the length and composition of the molecule (pentasaccharide sequence containing 3-0-sulfated glucosamine is required for heparin binding with antithrombin III).
The ability of sodium heparin in combination with antithrombin III to inhibit clotting factors IIa (thrombin) and Xa is the most important. The ratio of activity of sodium heparin against factor Xa to its activity against factor IIa is 09-11.
Sodium heparin reduces blood viscosity reduces vascular permeability stimulated by bradykinin histamine and other endogenous factors and thus prevents the development of stasis. Sodium heparin is able to sorb on the surface of endothelial membranes and blood cells increasing their negative charge that prevents platelet adhesion and aggregation. Sodium heparin slows smooth muscle hyperplasia and activates lipoprotein lipase and thus has hypolipidemic effect and prevents the development of atherosclerosis.
Sodium heparin binds some components of the complement system reducing its activity prevents the cooperation of lymphocytes and the formation of immunoglobulins binds histamine serotonin (i.e. has anti-allergic effect). Heparin increases renal blood flow increases cerebral vascular resistance reduces cerebral hyaluronidase activity reduces surfactant activity in the lungs suppresses excessive aldosterone synthesis in the adrenal cortex binds adrenaline modulates ovarian response to hormonal stimuli increases parathormone activity. As a result of interaction with enzymes, heparin can increase brain tyrosine hydroxylase activity of pepsinogen DNA polymerase and decrease myosin ATPase activity of pyruvate kinase RNA polymerase of pepsin. The clinical significance of these effects of heparin remains uncertain and poorly understood.
In acute coronary syndrome without persistent ST-segment elevation on the ECG (unstable angina pectoris without ST-segment elevation), sodium heparin in combination with acetylsalicylic acid reduces the risk of myocardial infarction and mortality. In ST-segment elevation myocardial infarction on ECG, sodium heparin is effective during primary percutaneous coronary revascularization in combination with glycoprotein IIb/IIIa receptor inhibitors and during thrombolytic therapy with streptokinase (increased rate of revascularization).
In high doses sodium heparin is effective in pulmonary thromboembolism and venous thrombosis in low doses it is effective for prevention of venous thromboembolism including after surgical operations.
After intravenous administration the drug action comes almost immediately, not later than 10-15 minutes and lasts only 3-6 hours. After subcutaneous injection the drug action starts slowly – after 40-60 minutes but lasts for 8 hours. Deficiency of antithrombin III in blood plasma or in the place of thrombosis may reduce the anticoagulant effect of sodium heparin.
Pharmacokinetics:
The maximum concentration (Cmax) after intravenous administration is reached almost immediately after subcutaneous administration in 2-4 h. Binding with plasma proteins – up to 95% volume of distribution is very small – 006 l/kg (does not leave the vascular bed due to strong binding to plasma proteins). It does not penetrate through the placenta and into the breast milk.
It is intensively taken up by endothelial cells and cells of the mononuclear-macrophage system (cells of the reticulo-endothelial system) and concentrated in the liver and spleen.
It is metabolized in the liver with the participation of N-desulfamidase and platelet heparinase, which is included in the metabolism of heparin at a later stage. Participation in the metabolism of platelet factor IV (anti-heparin factor), as well as the binding of heparin to the macrophage system explains the rapid biological inactivation and short duration of action. Desulfated molecules under the influence of renal endoglycosidase are converted into low molecular weight fragments. T1/2- 1-6 h (average – 15 h); increases in obesity hepatic and/or renal failure; decreases in pulmonary thromboembolism infections malignant tumors.
Extracted by the kidneys mainly as inactive metabolites and only when administered in high doses is excretion possible (up to 50%) in unchanged form. It is not excreted by hemodialysis.
Indications
Indications
prevention and treatment of venous thrombosis (including thrombosis of the superficial and deep veins of the lower extremities, renal vein thrombosis) and pulmonary embolism;
prevention and treatment of thromboembolic complications associated with atrial fibrillation;
prevention and treatment of peripheral arterial embolism (including those associated with mitral heart defects);
treatment of acute and chronic consumption coagulopathies (including stage I of DIC syndrome);
acute coronary syndrome without persistent ST segment elevation on the ECG (unstable angina, myocardial infarction without ST segment elevation on the ECG);
myocardial infarction with ST segment elevation during thrombolytic therapy, during primary percutaneous coronary revascularization (balloon angioplasty with or without stenting) and at a high risk of arterial or venous thrombosis and thromboembolism;
prevention and treatment of microthrombosis and microcirculation disorders, including hemolytic-uremic syndrome, glomerulonephritis (including lupus nephritis) and forced diuresis;
prevention of blood clotting during blood transfusion, in extracorporeal circulation systems (extracorporeal circulation during heart surgery, hemosorption, cytapheresis) and during hemodialysis;
processing of peripheral venous catheters.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Direct acting anticoagulant
ATX code
B01AB01
Pharmacodynamics:
The mechanism of action of sodium heparin is based primarily on its binding to antithrombin III, which is a natural inhibitor of activated blood coagulation factors – IIa (thrombin) IXa XIa and XIIa. Sodium heparin binds to antithrombin III and causes conformational changes in its molecule. As a result, the binding of antithrombin III to blood coagulation factors IIa (thrombin) IXa XIa and XIIa is accelerated and their enzymatic activity is blocked. The binding of heparin sodium to antithrombin III is electrostatic in nature and largely depends on the length and composition of the molecule (binding of heparin to antithrombin III requires a pentasaccharide sequence containing 3-0-sulfated glucosamine).
Of greatest importance is the ability of sodium heparin in combination with antithrombin III to inhibit coagulation factors IIa (thrombin) and Xa. The ratio of the activity of sodium heparin against factor Xa to its activity against factor IIa is 09-11.
Sodium heparin reduces blood viscosity, reduces vascular permeability stimulated by bradykinin, histamine and other endogenous factors, and thus prevents the development of stasis. Sodium heparin is able to adsorb on the surface of endothelial membranes and blood cells, increasing their negative charge, which prevents platelet adhesion and aggregation. Sodium heparin slows down smooth muscle hyperplasia, activates lipoprotein lipase and thus has a hypolipidemic effect and prevents the development of atherosclerosis.
Sodium heparin binds some components of the complement system, reducing its activity, prevents the cooperation of lymphocytes and the formation of immunoglobulins, binds histamine, serotonin (i.e., has an antiallergic effect). Heparin increases renal blood flow increases cerebral vascular resistance reduces the activity of brain hyaluronidase reduces the activity of surfactant in the lungs suppresses excessive synthesis of aldosterone in the adrenal cortex binds adrenaline modulates the ovarian response to hormonal stimuli increases the activity of parathyroid hormone. As a result of interaction with enzymes, heparin can increase the activity of brain tyrosine hydroxylase pepsinogen DNA polymerase and reduce the activity of myosin ATPase pyruvate kinase RNA polymerase pepsin. The clinical significance of these effects of heparin remains uncertain and poorly understood.
In acute coronary syndrome without persistent ST segment elevation on the ECG (unstable angina, myocardial infarction without ST segment elevation), sodium heparin in combination with acetylsalicylic acid reduces the risk of myocardial infarction and mortality. In myocardial infarction with ST segment elevation on the ECG, sodium heparin is effective in primary percutaneous coronary revascularization in combination with glycoprotein IIb/IIIa receptor inhibitors and in thrombolytic therapy with streptokinase (increasing the frequency of revascularization).
In high doses, sodium heparin is effective for pulmonary embolism and venous thrombosis; in small doses, it is effective for the prevention of venous thromboembolism, incl. after surgical operations.
After intravenous administration, the effect of the drug occurs almost immediately no later than 10-15 minutes and does not last long – 3-6 hours. After subcutaneous administration, the effect of the drug begins slowly – after 40-60 minutes but lasts 8 hours. A deficiency of antithrombin III in the blood plasma or at the site of thrombosis can reduce the anticoagulant effect of sodium heparin.
Pharmacokinetics:
The maximum concentration (Cmax) after intravenous administration is achieved almost immediately after subcutaneous administration after 2-4 hours. Bonding with plasma proteins – up to 95%, the volume of distribution is very small – 006 l / kg (does not leave the vascular bed due to strong binding to plasma proteins). Does not penetrate the placenta or into breast milk.
It is intensively captured by endothelial cells and cells of the mononuclear-macrophage system (cells of the reticuloendothelial system) and is concentrated in the liver and spleen.
Metabolized in the liver with the participation of N-desulfamidase and platelet heparinase, which is involved in the metabolism of heparin at later stages. Participation in the metabolism of platelet factor IV (antiheparin factor) as well as the binding of heparin to the macrophage system explains the rapid biological inactivation and short duration of action. Desulfated molecules are converted into low molecular weight fragments by the action of kidney endoglycosidase. T1/2 – 1-6 hours (on average – 15 hours); increases with obesity, liver and/or kidney failure; decreases with pulmonary embolism, infections of malignant tumors.
It is excreted by the kidneys mainly in the form of inactive metabolites and only with the administration of high doses is it possible to excrete (up to 50%) unchanged. Not excreted by hemodialysis.
Special instructions
Special instructions
Treatment with large doses is recommended in a hospital setting. Platelet count monitoring should be carried out before starting treatment on the first day of treatment and at short intervals throughout the entire period of administration of heparin sodium, especially between 6 and 14 days after the start of treatment. Treatment should be stopped immediately if there is a sharp decrease in the platelet count (see “Side effects”).
A sharp decrease in platelet count requires further investigation to identify heparin-induced immune thrombocytopenia. If this occurs, the patient should be advised that he should not be prescribed heparin in the future (even low molecular weight heparin). If there is a high likelihood of heparin-induced immune thrombocytopenia, heparin should be discontinued immediately.
If heparin-induced thrombocytopenia develops in patients receiving heparin for thromboembolic disease or in the event of thromboembolic complications, other antithrombotic agents should be used. Patients with heparin-induced immune thrombocytopenia (white thrombus syndrome) should not undergo heparinized hemodialysis. If necessary, they should use alternative methods of treatment for renal failure.
To avoid overdose, it is necessary to constantly monitor clinical symptoms indicating possible bleeding (bleeding of the mucous membranes, hematuria, etc.). In individuals who do not respond to heparin or require high doses of heparin, antithrombin III levels should be monitored.
Resistance to sodium heparin is often observed in cases of fever, thrombosis, thrombophlebitis, infectious diseases, myocardial infarction, malignant neoplasms, as well as after surgical interventions and with antithrombin III deficiency. In such situations, more careful laboratory monitoring (aPTT monitoring) is required.
Although sodium heparin does not cross the placental barrier and is not detected in breast milk, when administered in therapeutic doses, pregnant women and nursing mothers should be carefully monitored.
Particular care should be taken within 36 hours after birth.
It is necessary to carry out appropriate control laboratory tests (blood clotting time, activated partial thromboplastin time and thrombin time).
In women over 60 years of age, heparin can increase bleeding, and therefore the dose of heparin sodium in this category of patients should be reduced.
When using heparin in patients with arterial hypertension, blood pressure should be constantly monitored.
Before initiating sodium heparin therapy, a coagulation profile should always be performed, unless low doses are used.
In patients transitioning to oral anticoagulant therapy, sodium heparin should be continued until clotting time and APTT results are within the therapeutic range. Intramuscular injections should be excluded when prescribing sodium heparin for therapeutic purposes. Needle biopsies of infiltration and epidural anesthesia and diagnostic lumbar punctures should also be avoided if possible.
If massive bleeding occurs, sodium heparin should be discontinued and coagulation parameters should be examined. If the test results are within normal limits, then the likelihood of this bleeding due to the use of sodium heparin is minimal. Changes in the coagulogram tend to normalize after discontinuation of heparin.
Physical and chemical stability after dilution of heparin in the above solutions for infusion is maintained for 48 hours at room temperature (25 ± 2 ° C). If the drug is not used immediately, it can be used no later than 24 hours after dilution; however, it can be stored during this period at a temperature of 2 to 8 ° C only if aseptic conditions are observed when diluting it.
Impact on the ability to drive vehicles. Wed and fur.:
Studies have not been conducted to evaluate the effect of heparin on the ability to drive vehicles and engage in potentially hazardous activities.
Active ingredient
Active ingredient
Heparin sodium
Composition
Composition
1 ml contains:
Active substance: sodium heparin 5000 IU.
Excipient: water for injection up to 1 ml.
Pregnancy
Pregnancy
Heparin sodium does not penetrate the placental barrier. To date, there is no data indicating the possibility of fetal malformations due to the use of sodium heparin during pregnancy; There are also no results of animal experiments that would indicate the embryo- or fetotoxic effect of sodium heparin. However, there is evidence of an increased risk of premature birth and spontaneous abortion associated with bleeding. It is necessary to take into account the likelihood of complications when using sodium heparin in pregnant women with concomitant diseases, as well as in pregnant women receiving additional treatment.
Daily use of high doses of heparin sodium for more than 3 months may increase the risk of osteoporosis in pregnant women. Therefore, continuous use of high doses of sodium heparin should not exceed 3 months. Epidural anesthesia should not be used in pregnant women undergoing anticoagulant therapy. Anticoagulant therapy is contraindicated when there is a risk of bleeding, such as a threatened abortion.
Heparin sodium is not excreted in breast milk. Daily use of high doses of heparin sodium for more than 3 months may increase the risk of osteoporosis in breastfeeding women.
If it is necessary to use it during the specified periods, it is necessary to weigh the benefit/risk.
Contraindications
Contraindications
– Hypersensitivity to heparin and other components of the drug.
– Heparin-induced thrombocytopenia (with or without thrombosis) in history or currently.
– Bleeding (unless the benefits of sodium heparin outweigh the potential risks).
– Heparin sodium in a therapeutic dose should not be prescribed if it is not possible to ensure regular laboratory monitoring of blood clotting.
– Pregnancy and breastfeeding period.
With caution:
Patients with polyvalent allergies (including bronchial asthma).
In pathological conditions associated with an increased risk of bleeding such as:
– Diseases of the cardiovascular system: acute and subacute infective endocarditis, severe uncontrolled arterial hypertension, aortic dissection, cerebral aneurysm.
– Erosive and ulcerative lesions of the gastrointestinal tract, varicose veins of the esophagus with cirrhosis of the liver and other diseases, long-term use of gastric and small intestinal drainages, ulcerative colitis, hemorrhoids.
– Diseases of the hematopoietic organs of the blood and lymphatic system: leukemia hemophilia thrombocytopenia hemorrhagic diathesis.
– Diseases of the central nervous system: hemorrhagic stroke, traumatic brain injury.
– Malignant neoplasms.
– Congenital deficiency of antithrombin III and replacement therapy with antithrombin III drugs (smaller doses of heparin must be used to reduce the risk of bleeding).
Other physiological and pathological conditions: period of menstruation, threat of miscarriage, early postpartum period, severe liver diseases with impaired protein-synthetic function, chronic renal failure, recent surgery on the eyes of the brain or spinal cord, recent spinal (lumbar) puncture or epidural anesthesia, proliferative diabetic retinopathy, vasculitis, older age (over 60 years old, especially women).
Side Effects
Side Effects
Allergic reactions: skin hyperemia, drug fever, urticaria, rhinitis, skin itching and a feeling of heat in the soles, bronchospasm, collapse, anaphylactic shock. Other potential side effects include dizziness headache nausea decreased appetite vomiting diarrhea joint pain increased blood pressure and eosinophilia.
At the beginning of heparin treatment, transient thrombocygopenia may sometimes be observed with platelet counts ranging from 80 x 109/L to 150 x 109/L. Usually this situation does not lead to the development of complications and heparin treatment can be continued. In rare cases, severe thrombocytopenia (white blood clot syndrome), sometimes fatal, may occur. This complication should be assumed if the platelet count decreases below 80×109/l or by more than 50% of the initial level; in such cases, heparin administration is immediately stopped. Patients with severe thrombocytopenia may develop consumptive coagulopathy (fibrinogen depletion).
Against the background of heparin-induced thrombocytopenia: skin necrosis, arterial thrombosis accompanied by the development of gangrene, myocardial infarction, stroke.
With long-term use: osteoporosis, spontaneous bone fractures, soft tissue calcification, hypoaldosteronism, transient alopecia, priapism.
During heparin therapy, changes in biochemical blood parameters may be observed (increased activity of hepatic transaminases of free fatty acids and thyroxine in the blood plasma; hyperkalemia; recurrent hyperlipidemia during discontinuation of sodium heparin; false increase in blood glucose levels and errors in the results of Bromsofa and the new test).
Local reactions: irritation, pain, hyperemia, hematoma and ulceration at the injection site, bleeding.
Bleeding: typical – from the gastrointestinal tract and urinary tract at the site of drug administration in areas exposed to pressure from surgical wounds; hemorrhages in various organs (including adrenal glands, corpus luteum, retroperitoneal space).
If any of the side effects indicated in the instructions get worse or you notice any other side effects not listed in the instructions, tell your doctor.
Interaction
Interaction
Pharmaceutical interactions: sodium heparin solution is compatible only with 09% sodium chloride solution. Heparin sodium solution is incompatible with the following drug solutions: alteplase amikacin sulfate amiodarone ampicillin sodium benzylpenicillin sodium ciprofloxacin cytarabine dacarbazine danorubicin diazepam dobutamine doxorubicin hydrochloride droperidol erythromycin gentamicin sulfate haloperidol lactate hyaluronidase hydrocortisone sodium succinate dextrose fat emulsions idarubicin kanamycin sulfate methicillin sodium netilmicin sulfate opioids oxytetracycline hydrochloride polymyxin B promazine sulfate hydrochloride promethazine hydrochloride streptomycin sulfate sulfafurazole diethanolamine tetracycline hydrochloride tobramycin sulfate cephalothin sodium cephaloridine vancomycin hydrochloride vinblastine sulfate labetalol hydrochloride nicardipine hydrochloride.
Pharmacokinetic interaction: sodium heparin displaces phenytoin, quinidine propranolol and benzodiazepine derivatives from the sites of their binding to plasma proteins, which can lead to increased pharmacological action of these drugs. Sodium heparin binds and is inactivated by sodium protamine, alkaline polypeptides and tricyclic antidepressants.
Pharmacodynamic interaction: the anticoagulant effect of sodium heparin is enhanced when used simultaneously with other drugs that affect hemostasis, including. with antiplatelet drugs (acetylsalicylic acid clopidogrel prasugrel ticlopidine dipyridamole) indirect anticoagulants (warfarin phenylin sincumar) thrombolytic drugs (alteplase streptokinase urokinase) non-steroidal anti-inflammatory drugs (including phenylbutazone ibuprofen indomethacin diclofenac) glucocorticosteroids and dextran, resulting in an increased risk of bleeding. In addition, the anticoagulant effect of sodium heparin may be enhanced when combined with hydroxychloroquine, sulfinpyrazone, probenecid, ethacrynic acid, cytostatics, cefamandole, cefotetan, valproic acid, propylthiouracil.
The anticoagulant effect of sodium heparin is reduced when used simultaneously with ACTH, antihistamines, ascorbic acid, ergot alkaloids, nicotine, nitroglycerin, cardiac glycosides, thyroxine, tetracycline and quinine.
Heparin sodium may reduce the pharmacological effect of adrenocorticotropic hormone, glucocorticosteroids and insulin.
Overdose
Overdose
Symptoms: signs of bleeding.
Treatment: for minor bleeding caused by an overdose of heparin, it is enough to stop using it. In case of extensive bleeding, excess heparin is neutralized with protamine sulfate (1 mg of protamine sulfate per 100 IU of heparin). A 1% solution of protamine sulfate is administered intravenously very slowly. Every 10 minutes, do not administer more than 50 mg (5 ml) of protamine sulfate. Given the rapid metabolism of heparin sodium, the required dose of protamine sulfate decreases over time. To calculate the required dose of protamine sulfate, we can assume that T1/2 of sodium heparin is 30 minutes. When using protamine, severe anaphylactic reactions with a fatal outcome were observed, and therefore the drug should be administered only in a department equipped to provide emergency medical care for anaphylactic shock. Hemodialysis is ineffective.
Storage conditions
Storage conditions
In a place protected from light at a temperature not exceeding 25 ° C.
Keep out of the reach of children.
Shelf life
Shelf life
4 years.
Do not use after the expiration date indicated on the package.
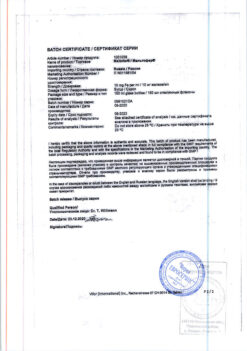
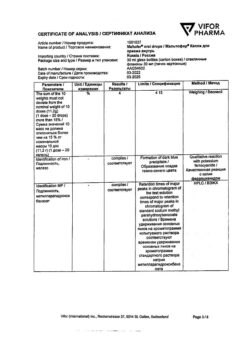
Manufacturer
Manufacturer
Velfarm LLC, Russia
Additional information
| Shelf life | 4 years. Do not use after the expiration date on the package. |
|---|---|
| Conditions of storage | In the dark place at a temperature not exceeding 25 °С. Store out of the reach of children. |
| Manufacturer | Welfarm, Russia |
| Medication form | solution |
| Brand | Welfarm |
Other forms…
Related products
Buy Heparin sodium,. 5000 units/ml 5 ml 5 pcs with delivery to USA, UK, Europe and over 120 other countries.