No products in the cart.
Glucose, 5% 250 ml
€1.00
Out of stock
(E-mail when Stock is available)
Description
Glucose increases redox processes in the body, improves antitoxic function of the liver, enhances myocardial contractile activity, and is a source of easily digestible carbohydrates.
The pharmacodynamic properties of 5%, 10% and 20% solutions of dextrose are similar to those of glucose, the main source of energy of cellular metabolism.
The 5% solution of dextrose is an isotonic solution with an osmolarity of about 278 mOsm/L. The caloric intake of 5% dextrose solution is 200 kcal/L,
10% dextrose solution is a hypertonic solution with an osmolarity of about 555 mOsm/L. The caloric intake of a 10% dextrose solution is 400 kcal/L.
The 20% dextrose solution is a hypertonic solution with an osmolarity of approximately 1110 mOsm/L. The caloric intake of a 20% dextrose solution is 680 kcal/L.
In parenteral nutrition 5%, 10% and 20% solutions of dextrose are administered as a source of carbohydrates (alone or as part of parenteral nutrition if necessary).
The 5% and 10% solutions of dextrose allow replenishment of fluid deficiencies without simultaneous administration of ions.
The 20% dextrose solution provides the maximum amount of calories in the minimum amount of fluid.
Dextrose entering the tissues is phosphorylated into glucose-6-phosphate, which is actively involved in many parts of the body’s metabolism.
When dextrose solutions are used to dilute and dissolve parenterally administered medications, the pharmacodynamic properties of the solution will depend on the substance added.
Pharmacokinetics:
Glucose is metabolized by two different pathways: anaerobic and aerobic.
Dextrose breaks down into pyruvic acid or lactic acid (anaerobic glycolysis) and is metabolized to carbon dioxide and water with the release of energy.
When using dextrose solution to dilute and dissolve parenterally administered medications, the pharmacokinetic properties of the solution will depend on the substance added.
Indications
Indications
5% glucose solution:
– as a source of carbohydrates (separately or as part of parenteral nutrition if necessary);
– for rehydration in case of fluid loss, especially in patients with a high need for carbohydrates;
– for dilution and dissolution of parenterally administered drugs.
Pharmacological effect
Pharmacological effect
Glucose enhances redox processes in the body, improves the antitoxic function of the liver, enhances the contractile activity of the myocardium, and is a source of easily digestible carbohydrates.
The pharmacodynamic properties of 5%, 10% and 20% dextrose solutions are similar to the properties of glucose, the main source of energy for cellular metabolism.
5% dextrose solution is an isotonic solution with an osmolarity of approximately 278 mOsm/L. The calorie intake of a 5% dextrose solution is 200 kcal/l,
10% dextrose solution is a hypertonic solution with an osmolarity of approximately 555 mOsm/L. The calorie intake of a 10% dextrose solution is 400 kcal/l.
20% dextrose solution is a hypertonic solution with an osmolarity of approximately 1110 mOsm/L. The caloric intake of a 20% dextrose solution is 680 kcal/l.
As part of parenteral nutrition, 5%, 10%, and 20% dextrose solutions are administered as a source of carbohydrate (alone or as part of parenteral nutrition as needed).
5% and 10% dextrose solutions allow you to replenish fluid deficiency without the simultaneous administration of ions.
A 20% dextrose solution provides the maximum amount of calories in a minimum volume of liquid.
Dextrose, entering the tissues, is phosphorylated, turning into glucose-6-phosphate, which is actively involved in many parts of the body’s metabolism.
When using dextrose solutions to dilute and dissolve parenterally administered drugs, the pharmacodynamic properties of the solution will depend on the substance added.
Pharmacokinetics:
Glucose is metabolized in two different ways: anaerobic and aerobic.
Dextrose, breaking down into pyruvic or lactic acid (anaerobic glycolysis), is metabolized to carbon dioxide and water, releasing energy.
When using a dextrose solution to dilute and dissolve parenterally administered drugs, the pharmacokinetic properties of the solution will depend on the substance added.
Special instructions
Special instructions
Since glucose (dextrose) tolerance may be impaired in patients with diabetes mellitus, renal failure, or those in acute critical condition, their clinical and biological parameters should be especially carefully monitored, in particular the concentration of electrolytes in the blood plasma, including magnesium or phosphorus, and the concentration of glucose in the blood. If hyperglycemia is present, the rate of drug administration should be adjusted or short-acting insulin should be prescribed. Typically, glucose is completely absorbed by the body (normally it is not excreted by the kidneys), so the appearance of glucose in the urine can be a pathological sign.
In case of prolonged administration or use of dextrose in high doses, it is necessary to monitor the concentration of potassium in the blood plasma and, if necessary, administer additional potassium to avoid hypokalemia.
During episodes of intracranial hypertension, careful monitoring of blood glucose concentrations is necessary.
The use of dextrose solutions can lead to hyperglycemia. Therefore, they are not recommended for administration after acute ischemic stroke, since hyperglycemia is associated with increased ischemic brain damage and impedes recovery.
Particularly careful clinical monitoring is required when starting intravenous administration of the drug.
For rehydration therapy, carbohydrate solutions should be used in combination with electrolyte solutions to avoid electrolyte imbalance (hyponatremia, hypokalemia).
It is necessary to monitor the concentration of glucose and the content of electrolytes in the blood, water balance, as well as the acid-base state of the body.
The solution should be inspected before use. Use only a clear solution without visible inclusions and if the packaging is not damaged. Administer immediately after connecting to the infusion system.
The solution should be administered using sterile equipment in compliance with the rules of asepsis and antisepsis.
To avoid air embolism, remove air from the infusion system using a solution.
Do not connect containers in series to avoid air embolism, which may occur due to air being drawn in from the first container before the solution is administered from the second container.
Delivering intravenous solutions contained in soft plastic containers under increased pressure to increase the flow rate may result in air embolism if residual air in the container is not completely removed before administration.
The use of an IV system with a gas outlet may result in an air embolism if the gas outlet is open. Soft plastic containers should not be used with these systems.
Added substances can be administered before infusion or during infusion through the injection site (if there is a special port for drug administration).
Adding other drugs to the solution or violating the administration technique may cause fever due to the possible entry of pyrogens into the body.
If adverse reactions develop, the infusion should be stopped immediately.
When adding other drugs before parenteral administration, it is necessary to check the isotonicity of the resulting solution.
Complete and thorough mixing under aseptic conditions is mandatory.
Solutions containing additional substances should be used immediately; their storage is prohibited.
If additional nutrients are administered, the osmolarity of the resulting mixture should be determined before infusion.
The resulting mixture must be administered through a central or peripheral venous catheter depending on the final osmolarity.
The compatibility of additionally administered drugs must be determined before they are added to the solution (similar to the use of other parenteral solutions). Assessing the compatibility of additionally administered drugs with the drug is the responsibility of the physician. It is necessary to check the resulting solution for changes in color and/or the appearance of sediment, insoluble complexes or crystals. You should study the instructions for use of the added medications.
From a microbiological point of view, the diluted drug should be used immediately. The exception is dilutions prepared under controlled and aseptic conditions. Otherwise, after preparing the solution, the timing and conditions of its storage before administration are the responsibility of the user.
Children
In newborns, especially those born prematurely or with low body weight, the risk of developing hypo- or hyperglycemia is increased, therefore, during the period of intravenous administration of dextrose solutions, careful monitoring of blood glucose concentrations is necessary to avoid long-term undesirable consequences. Hypoglycemia in newborns can lead to prolonged seizures, coma, and brain damage. Hyperglycemia has been associated with intraventricular hemorrhage, delayed bacterial and fungal infections, retinopathy of prematurity, necrotizing enterocolitis, bronchopulmonary dysplasia, prolonged hospitalization, and mortality.
To avoid potentially fatal overdose of intravenous drugs in neonates, special attention must be paid to the route of administration. For the treatment of “symptomatic” hypoglycemia, it is preferable to use a 10% glucose solution. In this case, it is necessary to constantly monitor glucose and blood levels and, if necessary, adjust them. It should be taken into account that newborns with different pathologies have different needs for exogenous glucose. Abrupt cessation of infusion can cause hypoglycemia, so the dose of glucose is reduced gradually, titration of the glucose solution is stopped if the child remains normoglycemia when glucose is administered at a rate of 4 mg/kg/min.
When using a syringe pump for intravenous administration of drugs to newborns, the container with the solution should not be left attached to the syringe.
When using an infusion pump, all clamps on the system must be closed before removing the system from the pump or turning it off, regardless of whether there is a device in the system that prevents the free flow of fluid.
IV infusion devices and other drug administration equipment should be monitored regularly.
If the drug contains dextrose derived from corn, the drug is contraindicated in patients with a known intolerance to corn or corn products, because The following manifestations of hypersensitivity are possible: anaphylactic reactions, chills and fever.
For drugs in containers:
Containers should be discarded after single use.
Any unused dose should be discarded.
Do not reconnect partially used containers.
Impact on the ability to drive vehicles. Wed and fur.:
Not applicable (due to the use of the drug exclusively in a hospital setting).
Active ingredient
Active ingredient
Dextrose
Composition
Composition
For 1 l:
active substances:
dextrose (glucose) monohydrate in terms of dextrose 50 g/100 g/200 g;
excipients:
sodium chloride 0.26 g, 0.1 M hydrochloric acid solution to pH 3.0-4.5, water for injection up to 1.0 l.
Theoretical osmolarity, mOsmol/l – 277/555/1110.
Contraindications
Contraindications
Decompensated diabetes mellitus and diabetes insipidus; hyperosmolar coma; hemodilution and extracellular hyperhydration or hypervolemia; hyperglycemia and hyperlactatemia: severe renal failure (with oliguria or anuria); uncompensated heart failure; generalized edema (including pulmonary and cerebral edema) and cirrhosis of the liver with ascites; other known forms of glucose intolerance (eg metabolic stress); hypersensitivity to the components of the drug; administration of the solution within the first 24 hours after head injury; use of the same infusion system as for blood transfusion due to the risk of hemolysis and thrombosis; patients with a known intolerance to corn or corn products (when receiving corn dextrose); contraindications to any drugs added to a glucose solution.
With caution:
Diabetes mellitus, intracranial hypertension, hyponatremia, childhood.
Side Effects
Side Effects
Adverse reactions (AR) are grouped by systems and organs in accordance with the MedDRA dictionary and the WHO classification of the incidence of HP:
Very common (≥ 1/10)
Common (≥ 1/100 to < 1/10)
Uncommon (≥ 1/1000 to < 1/100)
Rare (≥ 1/10000 to < 1/1000)
Very rare (< 1/10000)
Frequency unknown – (frequency cannot be determined from available data).
From the immune system
Frequency unknown: anaphylactic reactions, hypersensitivity.
Metabolism and nutrition
Frequency unknown: water and electrolyte imbalance (hypokalemia, hypomagnesemia and hypophosphatemia), hyperglycemia, hemodilution, dehydration, hypervolemia.
From the side of the heart
Frequency unknown: acute left ventricular failure.
From the side of blood vessels
Frequency unknown: venous thrombosis, phlebitis.
From the skin and subcutaneous tissues
Frequency unknown: increased sweating.
From the kidneys and urinary tract
Frequency unknown: polyuria.
General and administration site disorders
Not known: chills, fever, injection site infection, injection site irritation, extravasation, injection site tenderness.
Laboratory and instrumental data
Frequency unknown: glycosuria,
Adverse reactions may be related to the drug that was added to the solution. The likelihood of other adverse reactions depends on the properties of the specific drug added.
If undesirable reactions occur, administration of the solution should be stopped, the patient’s condition should be assessed, and adequate measures should be taken.
Interaction
Interaction
The combined use of catecholamines and steroids reduces the absorption of dextrose (glucose).
When mixed with other drugs, it is necessary to visually check them for compatibility.
For dilution or dissolution of other drugs, the drug should be used only if there are instructions for dilution with dextrose solution in the instructions for use for this drug.
In the absence of information on compatibility, the drug should not be mixed with other drugs.
Before adding any drug, it must be ensured that it is soluble and stable in water within the pH range of the drug.
After adding a compatible drug to the preparation, the resulting solution should be administered immediately.
Medicines with known incompatibility should not be used.
When administering dextrose solutions through the same infusion system as for blood transfusion, there is a possible risk of hemolysis and thrombosis.
Overdose
Overdose
Symptoms: prolonged infusion of the drug can lead to hyperglycemia, glycosuria, hyperosmolarity, osmotic diuresis and dehydration. Rapid infusion can create fluid accumulation in the body with hemodilution and hypervolemia, and by increasing the body’s ability to oxidize glucose, rapid infusion can cause hyperglycemia. There may also be a decrease in potassium and inorganic phosphate in the blood plasma.
When dextrose infusion solution is used to dilute and dissolve other intravenous drugs, clinical signs and symptoms of overdose may be related to the properties of the drugs used.
Treatment: if symptoms of overdose appear, the administration of the solution should be stopped, the patient’s condition assessed, short-acting insulin administered, and, if necessary, supportive symptomatic therapy.
Storage conditions
Storage conditions
In a dry place, at a temperature of 5 to 30 °C.
Keep out of the reach of children.
Freezing of the drug is allowed provided the container remains sealed.
Shelf life
Shelf life
2 years.
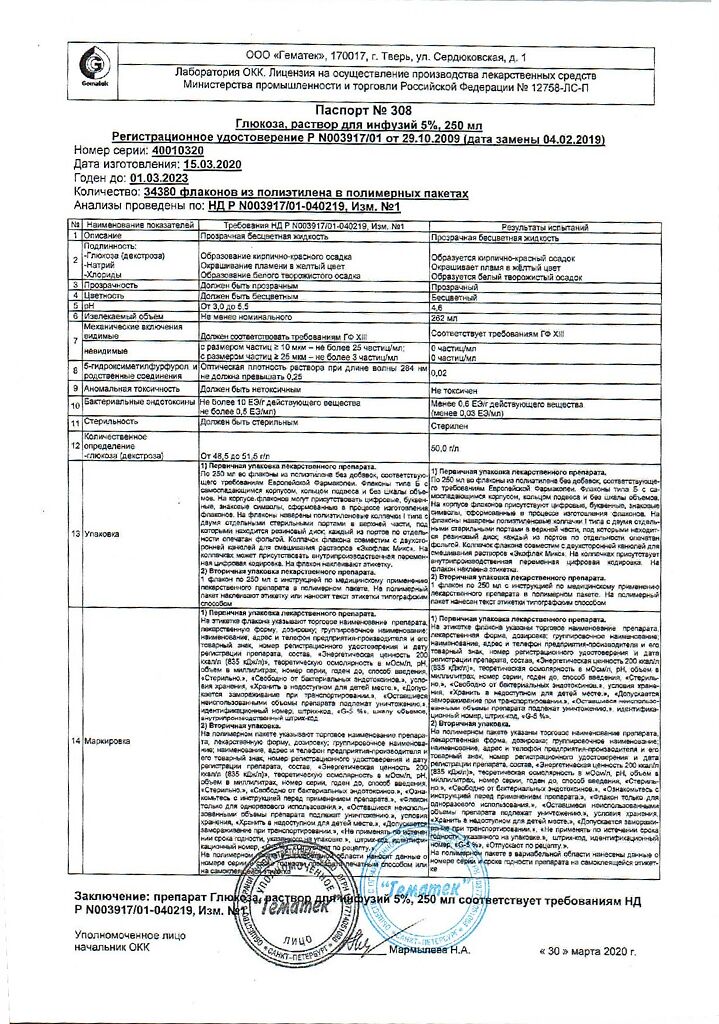
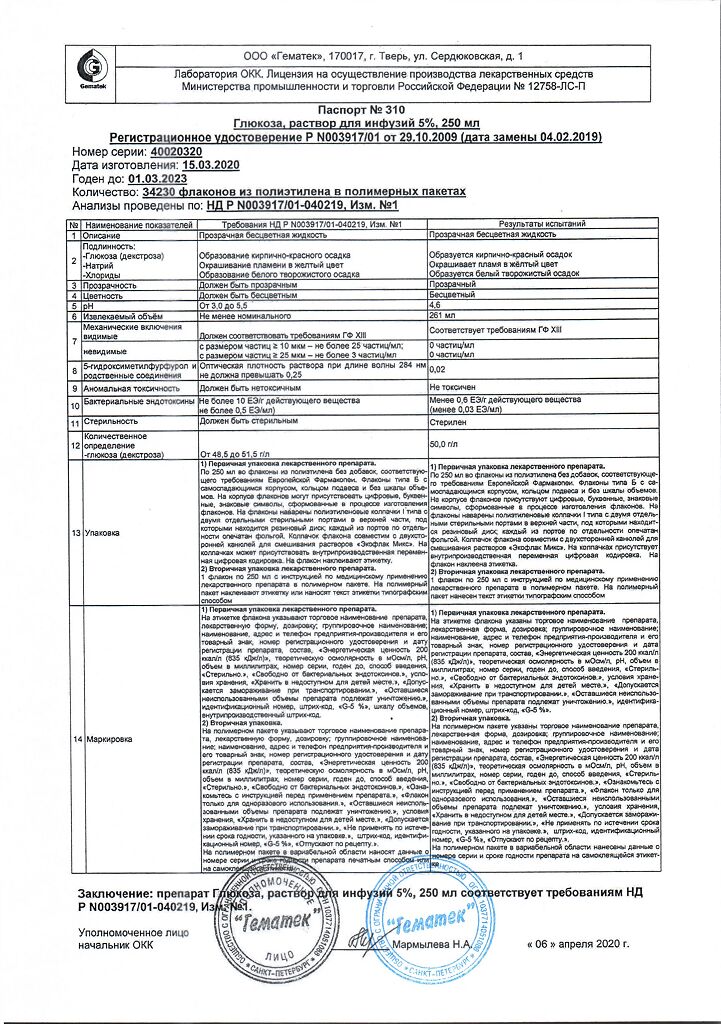
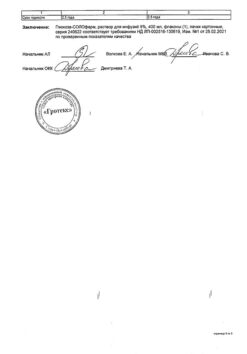
Manufacturer
Manufacturer
Gematek, Russia
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | In a dry place at a temperature of 5 to 30 ° C. Store out of reach of children. Freezing of the drug is allowed as long as the container remains airtight. |
| Manufacturer | Hematec, Russia |
| Medication form | solution for infusion |
| Brand | Hematec |
Other forms…
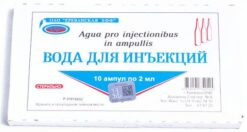
Related products
Buy Glucose, 5% 250 ml with delivery to USA, UK, Europe and over 120 other countries.