No products in the cart.
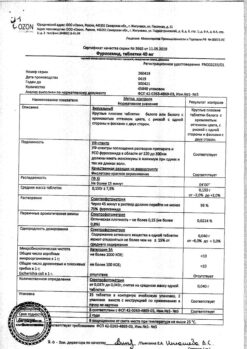
Furosemide, tablets 40 mg, 20 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
Description
“Loop” diuretic; causes rapid onset, strong and short-term diuresis. It blocks reabsorption of sodium and chlorine ions in both proximal and distal parts of renal tubules and in the thick segment of the ascending Gentlé loop. Furosemide has pronounced diuretic, natriuretic and chloruretic actions.
Due to an increase in sodium ion excretion, there is a secondary (mediated by osmotically bound water) enhanced excretion of water and increased secretion of potassium ions in the distal part of the renal tubule. At the same time, the excretion of calcium and magnesium ions increases. It has secondary effects due to release of intrarenal mediators and redistribution of intrarenal blood flow. Against the background of a course of treatment there is no weakening of the effect.
In heart failure, furosemide rapidly reduces preload (due to vein dilation), reduces pulmonary artery pressure and left ventricular filling pressure. It has antihypertensive effect due to increased excretion of sodium chloride and reduction of the response of vascular smooth muscle to vasoconstrictor effects and due to reduction of circulating blood volume.
After oral administration of 40 mg of furosemide, the diuretic effect begins within 60 min and lasts for about 3-6 h (with reduced renal function, up to 8 h). During the period of action, the excretion of sodium ions increases significantly, but after its cessation the excretion rate decreases below the initial level (“ricochet” or “withdrawal” syndrome).
The phenomenon is due to a sharp activation of the renin-angiotensin-aldosterone system and other antinatriuretic neurohumoral regulatory links in response to massive diuresis; it stimulates the arginine-vasopressive and sympathetic systems. Reduces plasma levels of atrial natriuretic factor, causes vasoconstriction. Due to the “ricochet” syndrome, once-daily administration may not cause significant effect on daily sodium ion excretion and blood pressure.
Indications
Indications
Edema syndrome:
Active ingredient
Active ingredient
Composition
Composition
Interaction
Interaction
Concomitant use with phenobarbital and phenytoin decreases the effect of furosemide.
Induces concentration and risk of nephro- and ototoxic effects of cephalosporins, chloramphenicol, etacrynic acid, cisplatin, amphotericin B (due to competitive renal excretion).
In concomitant use of aminoglycosides with furosemide the excretion of aminoglycosides is delayed and the risk of ototoxic and nephrotoxic effects increases. For this reason, the use of this drug combination should be avoided unless it is necessary for vital indications, in which case correction (reduction) of maintenance doses of aminoglycosides is required.
Enhances the effectiveness of diazoxide and theophylline, reduces the effectiveness of hypoglycemic agents, allopurinol.
Drugs that block tubular secretion increase the serum concentration of furosemide. Drugs with nephrotoxic effects – when combined with furosemide, the risk of their nephrotoxic effects increases.
The GKS and carbenoxolone in combination with furosemide increase the risk of hypokalemia.
Concomitant use with cardiac glycosides increases the risk of digitalis intoxication with water-electrolyte disturbances (hypokalemia or hypomagnesemia).
It increases neuromuscular blockade of depolarizing myorelaxants (suxamethonium) and weakens the effect of nondepolarizing myorelaxants (tubocurarin).
NSAIDs (including indomethacin and acetylsalicylic acid) in combination with furosemide may temporarily decrease creatinine clearance and increase serum potassium and reduce the diuretic and antihypertensive effects of furosemide. In patients with hypovolemia and dehydration (including against the background of furosemide) NSAIDs may cause acute renal failure. Furosemide may increase the toxic effects of salicylates (due to competitive renal excretion).
Sucralfate reduces absorption of furosemide and weakens its effect (these drugs should be taken at least 2 hours apart).
Combination with carbamazepine may increase the risk of hyponatremia.
Antihypertensive agents, diuretics, or other agents capable of lowering BP when combined with furosemide may lead to a more pronounced antihypertensive effect.
Prescribing ACE inhibitors to patients previously treated with furosemide may lead to excessive reduction of blood pressure with impairment of renal function, and in some cases to development of acute renal failure, therefore three days before starting treatment with ACE inhibitors or increasing their dose, it is recommended to either withdraw furosemide or decrease its dose.
Probenecid, methotrexate and other drugs that, like furosemide, are secreted in the renal tubules may reduce the effects of furosemide (the same renal secretion pathway); on the other hand, furosemide may lead to reduced renal excretion of these drugs.
Lithium salts – Furosemide reduces lithium excretion, thereby increasing serum lithium concentrations and increasing the risk of lithium toxicity, including its damaging effects on the heart and nervous system. Therefore, monitoring of serum lithium concentrations is required when using this combination.
The concomitant use of cyclosporine A and furosemide increases the risk of gouty arthritis due to furosemide-induced hyperuricemia and disruption of urate excretion by cyclosporine.
Presor amines (epinephrine, norepinephrine) and furosemide mutually reduce efficacy.
The radiopaque agents – Patients at high risk for nephropathy on radiopaque drug administration who received furosemide had a higher incidence of renal dysfunction compared to patients at high risk for nephropathy on radiopaque drug administration who received intravenous hydration only before radiopaque drug administration.
Directions for use
Directions for use
The tablets should be taken on an empty stomach, without chewing and with plenty of fluid. When prescribing Furosemide, it is recommended to use the lowest dose sufficient to achieve the desired effect. The maximum daily dose for adults is 1500 mg.
The initial single dose in children is determined at the rate of 1-2 mg/kg body weight/day with possible increase in the dose to a maximum of 6 mg/kg/day, provided that the drug is not taken more than 6 hours later. The duration of treatment is determined by the physician individually, depending on the indications.
The dosage regimen in adults
Oedema syndrome in chronic heart failure
The initial dose is 20-80 mg/day. The required dose is adjusted depending on the diuretic response. It is recommended to divide daily dose into 2-3 doses.
Oedematous syndrome in chronic renal failure
In patients with chronic renal failure, careful dose selection is required by gradually increasing the dose so that fluid loss occurs gradually (at the beginning of treatment, fluid loss of approximately 2 kg body weight/day is possible). Recommended initial dose is 40-80 mg/day. The required dose is adjusted according to the diuretic response. The entire daily dose should be taken once or divided into two doses. In patients on hemodialysis the maintenance dose is usually 250-1500 mg/day.
Oedema in nephrotic syndrome
The initial dose is 40-80 mg/day. The required dose is adjusted depending on the diuretic response. The daily dose can be taken in one dose or divided into several doses.
Oedema syndrome in liver disease
Furosemide is indicated in addition to treatment with aldosterone antagonists in case of their insufficient effectiveness. To prevent development of complications such as poor orthostatic circulation regulation or disturbances of electrolyte or acid-base state, the dose should be chosen carefully, so that fluid loss is gradual (at the beginning of treatment the fluid loss is possible up to about 0.5 kg of body weight/day). The starting dose is 20-80 mg/day.
Arterial hypertension
Furosemide Sofarma may be used in monotherapy or in combination with other hypotensive agents. The usual maintenance dose is a dose of 20-40 mg/day. When furosemide is added to drugs already prescribed, their dose should be reduced by half. In arterial hypertension combined with chronic renal insufficiency, higher doses of the drug may be required.
Special Instructions
Special Instructions
Before starting therapy with Furosemide Sopharma, the presence of marked urine outflow disorders should be excluded; patients with partial urine outflow disorder should be closely monitored. During the course of treatment it is necessary to periodically monitor blood pressure, blood plasma electrolytes (including sodium, calcium, potassium, magnesium ions), acid-base balance, residual nitrogen, creatinine, uric acid, liver function and make, if necessary, corresponding correction of treatment.
The use of furosemide slows excretion of uric acid, which may provoke an exacerbation of the course of gout.
Patients with hypersensitivity to sulfonamides and sulfonylurea derivatives may have cross-sensitivity to furosemide.
Patients receiving high doses of furosemide should not limit their intake of table salt to avoid the development of hyponatremia and metabolic alkalosis. To prevent hypokalemia, concomitant administration of potassium preparations and potassium-saving diuretics is recommended, as well as adherence to a diet rich in potassium. Dosage regimen of patients with ascites with liver cirrhosis should be chosen under hospital conditions (disorders of water-electrolyte balance may lead to hepatic coma). Regular monitoring of plasma electrolyte content is indicated for this category of patients.
In case of appearance or worsening of azotemia and oliguria in patients with severe progressive renal disease, it is recommended to stop treatment.
In patients with diabetes mellitus or with reduced glucose tolerance, periodic monitoring of blood and urine glucose concentrations is required.
In unconscious patients with benign prostatic hyperplasia, ureteral narrowing, or hydronephrosis, monitoring of urine output is necessary due to the possibility of acute urinary retention.
The drug contains lactose monohydrate, so patients with rare hereditary problems of galactose intolerance, lactase lapp deficiency, or glucose-galactose malabsorption should not take this medication.
The drug contains wheat starch in amounts that are safe for use in patients with celiac disease (gluten enteropathy).
Patients with wheat allergy (other than celiac disease) should not use this medicine.
Impact on driving and operating machinery
At the time of treatment with Furosemide Sofarma, potentially hazardous activities requiring increased attention and rapid psychomotor reactions (driving and operating machinery) should be avoided.
Features
Features
Absorption is high, Cmax is noted in plasma when administered orally after 1 hour.
The bioavailability is 60-70%. Relative Vd – 0.2 l/kg. Binding to plasma proteins is 98%. It penetrates through the placental barrier and is excreted with breast milk. It is metabolized in liver with formation of 4-chloro-5-sulfamoylanthranilic acid. It is secreted into the lumen of renal tubules through the anion transport system existing in the proximal nephron. It is excreted mainly (88%) by the kidneys unchanged and as metabolites; the rest is excreted by the intestine. T1/2 – 1-1.5 h.
Peculiarities of pharmacokinetics in certain groups of patients
In renal insufficiency, excretion of furosemide is slower, and T1/2sub>1/2 is increased; in severe renal insufficiency, the final T1/2 may increase up to 24 h.
In nephrotic syndrome, decreased plasma protein concentrations result in increased concentrations of unbound furosemide (its free fraction), increasing the risk of ototoxic effects. On the other hand,
the diuretic effect of furosemide in these patients may be reduced due to binding of furosemide to albumin in the tubules and decreased tubular secretion of furosemide.
In hemodialysis, peritoneal dialysis and continuous ambulatory peritoneal dialysis, furosemide is slightly excreted.
In hepatic insufficiency, the T1/2 of furosemide is increased by 30-90% mainly due to increased relative volume of distribution. Pharmacokinetic parameters in this category of patients may vary greatly.
In heart failure, severe arterial hypertension, and in elderly patients, excretion of furosemide is delayed due to decreased renal function.
Contraindications
Contraindications
Side effects
Side effects
Cardiovascular system disorders: pronounced BP decrease, collapse, tachycardia, arrhythmias, susceptibility to thrombosis, decreased circulating blood volume.
Central nervous system: dizziness, headache, muscle weakness, calf cramps (tetany), paresthesias, apathy, adynamia, weakness, drowsiness, drowsiness, confusion.
Sensory organs: visual and hearing impairment, tinnitus.
In the digestive system: anorexia, dry mouth, thirst, nausea, vomiting, diarrhea, constipation, cholestatic jaundice, pancreatitis (exacerbation), hepatic encephalopathy.
Urogenital system disorders: oliguria, acute retention of urine (in patients with benign prostatic hyperplasia), interstitial nephritis, hematuria, decreased potency.
Endocrine system: decreased glucose tolerance, manifestation of latent diabetes mellitus.
Allergic reactions: purpura, urticaria, exfoliative dermatitis, erythema multiforme exudative, vasculitis, necrotizing angiitis, skin itching, chills, fever, photosensitization, anaphylactic shock, Stevens-Johnson syndrome, bullous pemphigoid, toxic epidermal necrolysis.
Hematopoietic disorders: leukopenia, thrombocytopenia, agranulocytosis, aplastic anemia, eosinophilia.
Water-electrolyte metabolism: hypovolemia, dihydration (risk of thrombosis and thromboembolism), hypokalemia, hyponatremia, hypochloremia, hypocalcemia, hypomagnesemia, metabolic alkalosis.
Laboratory parameters: hyperglycemia, hypertriglyceridemia, hypercholesterolemia, hyperuricemia, glucosuria, hypercalciuria, increased liver transaminases activity, eosinophilia.
Overdose
Overdose
Symptoms: marked BP decrease, collapse, shock, hypovolemia, dehydration, hemoconcentration, arrhythmias (including AV block, ventricular fibrillation), acute renal failure with anuria, thrombosis, thromboembolism, drowsiness, confusion, flaccid paralysis, apathy.
Treatment: correction of water-electrolyte balance and acid-base balance, replenishment of circulating blood volume, gastric lavage, activated charcoal, symptomatic treatment. There is no specific antidote.
Additional information
| Shelf life | 5 years. Do not use after the expiration date printed on the package. |
|---|---|
| Conditions of storage | In a dry place protected from light, at a temperature not exceeding 25 ° C. Keep out of reach of children! |
| Manufacturer | Sofarma JSC, Bulgaria |
| Medication form | pills |
| Brand | Sofarma JSC |
Other forms…
Related products
Buy Furosemide, tablets 40 mg, 20 pcs. with delivery to USA, UK, Europe and over 120 other countries.