No products in the cart.
Frauxiparin, 9,500 anti-ha me/ml 0.3 ml syringes 10 pcs
€116.74 €97.29
Description
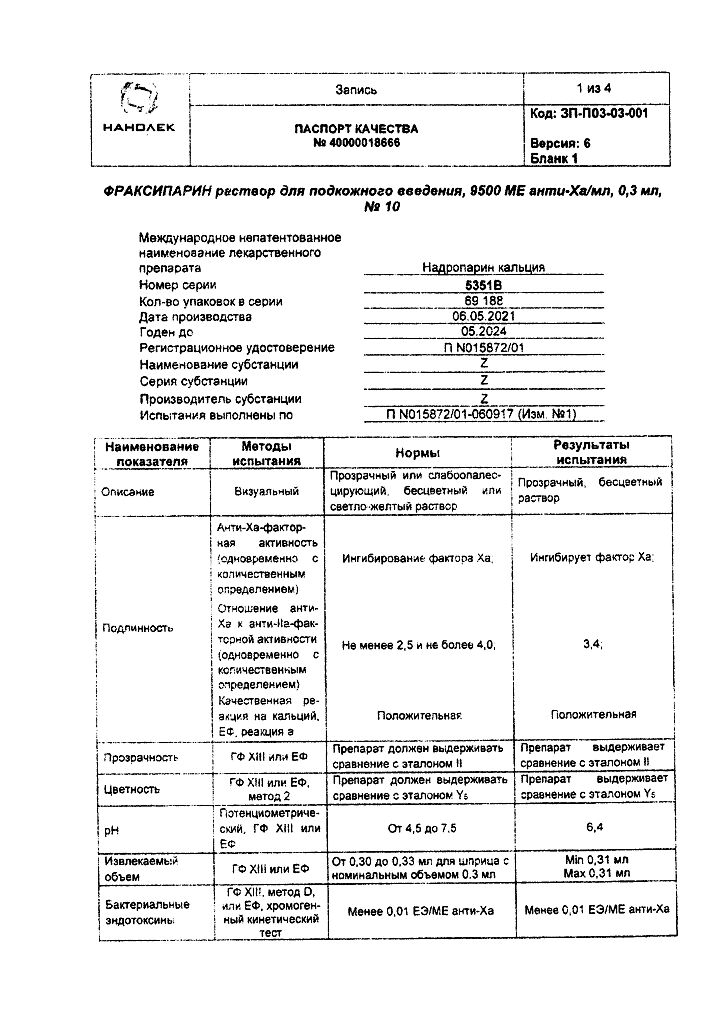
Fraxiparin is a low molecular weight heparin (LMWH) obtained by depolymerization from standard heparin and is a glycosoaminoglycan with an average molecular weight of 4300 daltons.
It exhibits a high ability to bind to the plasma protein antithrombin III (AT III). This binding leads to accelerated inhibition of factor Xa, which explains the high antithrombotic potential of nadroparin.
The other mechanisms providing the antithrombotic effect of nadroparin include activation of tissue factor conversion inhibitor (TFPI), activation of fibrinolysis by direct release of tissue plasminogen activator from endothelial cells and modification of blood rheological properties (decrease of blood viscosity and increase of permeability of membranes of platelets and granulocytes).
Nadroparin calcium is characterized by higher anti-Xa factor activity compared to anti-IIa factor or antithrombotic activity and has both immediate and prolonged antithrombotic activity. Compared with unfractionated heparin, nadroparin has less effect on platelet function and aggregation and little effect on primary hemostasis.
In prophylactic doses nadroparin does not cause a pronounced decrease in the BHRT. With a course of treatment during the period of maximum activity it is possible to increase the ABTV to a value of 1.4 times higher than the standard one. This prolongation reflects the residual antithrombotic effect of calcium nadroparin.
Indications
Indications
– Prevention of thromboembolic complications during surgical and orthopedic interventions in patients with a high risk of thrombosis (acute respiratory and/or heart failure in ICU conditions, unstable angina, myocardial infarction without a pathological Q wave on the ECG).
– Treatment of thromboembolism.
– Prevention of blood clotting during hemodialysis.
Pharmacological effect
Pharmacological effect
Fraxiparin, a low molecular weight heparin (LMWH), obtained by depolymerization from standard heparin, is a glycosaminoglycan with an average molecular weight of 4300 daltons.
Shows a high ability to bind to the blood plasma protein antithrombin III (AT III). This binding leads to accelerated inhibition of factor Xa, which accounts for the high antithrombotic potential of nadroparin.
Other mechanisms mediating the antithrombotic effect of nadroparin include activation of tissue factor converting inhibitor (TFPI), activation of fibrinolysis through direct release of tissue plasminogen activator from endothelial cells, and modification of blood rheological properties (decreasing blood viscosity and increasing platelet and granulocyte membrane permeability).
Nadroparin calcium is characterized by higher anti-Xa factor activity compared to anti-IIa factor or antithrombotic activity and has both immediate and prolonged antithrombotic activity. Compared with unfractionated heparin, nadroparin has a lesser effect on platelet function and aggregation and a less pronounced effect on primary hemostasis.
In prophylactic doses, nadroparin does not cause a significant decrease in aPTT. During a course of treatment during the period of maximum activity, it is possible to increase the aPTT to a value 1.4 times higher than the standard one. This prolongation reflects the residual antithrombotic effect of nadroparin calcium.
Special instructions
Special instructions
Particular attention should be paid to the specific instructions for use for each drug belonging to the class of low molecular weight heparins, because they may use different dosage units (IU or mg). Because of this, alternating Fraxiparine with other LMWHs during long-term treatment is unacceptable. It is also necessary to pay attention to which drug is used – Fraxiparine or Fraxiparine Forte, because this affects the dosage regimen. Graduated syringes are designed to select the dose depending on the patient’s body weight.
Fraxiparine is not intended for intramuscular administration. Since when using heparins there is a possibility of developing thrombocytopenia (heparin-induced thrombocytopenia), platelet levels must be monitored during the entire course of treatment with Fraxiparin.
Rare cases of thrombocytopenia, sometimes severe, have been reported, which could be associated with arterial or venous thrombosis, which is important to consider in the following cases: with thrombocytopenia; with a significant decrease in platelet levels (by 30-50% compared to normal values); with negative dynamics of thrombosis for which the patient is receiving treatment; with DIC syndrome. In these cases, treatment with Fraxiparine should be discontinued. Thrombocytopenia is immunoallergic in nature and is usually observed between days 5 and 21 of therapy, but may occur earlier if the patient has a history of heparin-induced thrombocytopenia.
If there is a history of heparin-induced thrombocytopenia (due to the use of conventional or low molecular weight heparins), Fraxiparine can be prescribed if necessary. However, strict clinical monitoring and, at a minimum, daily platelet count measurement are indicated in this situation.
If thrombocytopenia occurs, use of Fraxiparine should be discontinued immediately. If thrombocytopenia occurs against the background of heparins (regular or low molecular weight), then the possibility of prescribing anticoagulants of other groups should be considered. If other drugs are not available, another low molecular weight heparin may be used. In this case, the number of platelets in the blood should be monitored daily. If signs of initial thrombocytopenia continue to be observed after changing the drug, then treatment should be stopped as soon as possible.
It must be remembered that monitoring of platelet aggregation based on in vitro tests is of limited value in the diagnosis of heparin-induced thrombocytopenia. In elderly patients, renal function should be assessed before starting Fraxiparine therapy.
Heparins may suppress aldosterone secretion, which may lead to hyperkalemia, especially in patients with elevated blood potassium levels or in patients at risk of developing hyperkalemia (diabetes mellitus, chronic renal failure, metabolic acidosis, or concomitant use of drugs that can cause hyperkalemia during long-term therapy). In patients at increased risk of developing hyperkalemia, blood potassium levels should be monitored.
The risk of spinal/epidural hematomas increases in persons with installed epidural catheters or with concomitant use of other drugs that affect hemostasis (NSAIDs, antiplatelet agents, other anticoagulants).
The risk is also likely to increase with traumatic or repeated epidural or spinal taps. The issue of the combined use of neuraxial blockade and anticoagulants should be decided individually, after assessing the effectiveness/risk ratio. In patients already receiving anticoagulants, the need for spinal or epidural anesthesia should be justified. In patients undergoing elective surgery using spinal or epidural anesthesia, the need for anticoagulants should be justified.
If the patient is undergoing a lumbar puncture or spinal or epidural anesthesia, a sufficient time interval should be maintained between the administration of Fraxiparine and the insertion or removal of the spinal/epidural catheter or needle. Careful monitoring of the patient is necessary to identify signs and symptoms of neurological disorders. If disturbances are detected in the patient’s neurological status, urgent appropriate therapy is required.
When preventing or treating venous thromboembolism, as well as when preventing blood coagulation in the extracorporeal circulatory system during hemodialysis, co-administration of Fraxiparine with drugs such as acetylsalicylic acid, other salicylates, NSAIDs and antiplatelet agents is not recommended, because this may increase the risk of bleeding.
Fraxiparine should be prescribed with caution to patients receiving oral anticoagulants, systemic corticosteroids and dextrans. When prescribing oral anticoagulants to patients receiving Fraxiparine, its use should be continued until the prothrombin time stabilizes to the required value.
Active ingredient
Active ingredient
Nadroparin calcium
Composition
Composition
1 syringe contains nadroparin calcium 2850 IU
Pregnancy
Pregnancy
Currently, there is only limited data on the penetration of nadroparin through the placental barrier in humans.
Therefore, the use of Fraxiparine during pregnancy is not recommended, unless the potential benefit to the mother outweighs the risk to the fetus.
Currently, there are only limited data on the excretion of nadroparin in breast milk.
In this regard, the use of nadroparin during lactation (breastfeeding) is not recommended.
Experimental studies on animals did not reveal a teratogenic effect of nadroparin calcium.
Contraindications
Contraindications
– Thrombocytopenia with the use of nadroparin in the anamnesis.
– Signs of bleeding or increased risk of bleeding associated with impaired hemostasis (except for disseminated intravascular coagulation not caused by heparin).
– Organic diseases with a tendency to bleeding (for example, acute gastric or duodenal ulcers).
– Injuries or surgical interventions on the brain, spinal cord or eyes.
– Intracranial hemorrhage.
– Acute septic endocarditis.
– Severe renal failure (creatinine clearance less than 30 ml/min) in patients receiving Fraxiparine for the treatment of thromboembolism, unstable angina and non-Q wave myocardial infarction.
– Children and adolescence (up to 18 years).
– Hypersensitivity to nadroparin or any other components of the drug.
Fraxiparine should be prescribed with caution in situations associated with an increased risk of bleeding: with liver failure, with renal failure, with severe arterial hypertension, with a history of peptic ulcers or other diseases with an increased risk of bleeding, with circulatory disorders in the choroid and retina of the eye, in the postoperative period after operations on the brain, spinal cord or eyes, in patients weighing less than 40 kg, with a duration of therapy, exceeding the recommended (10 days), in case of non-compliance with the recommended treatment conditions (especially increasing the duration and dose for course use), when combined with drugs that increase the risk of bleeding.
Side Effects
Side Effects
The most common side effect is the formation of a subcutaneous hematoma at the injection site. In some cases, the appearance of dense nodules is observed, which does not indicate heparin encapsulation, which disappear after a few days.
Large doses of Fraxiparine can provoke bleeding of various localizations and mild thrombocytopenia (type I), which usually disappears with further therapy. A temporary moderate increase in the level of liver enzymes (ALT, AST) is possible.
Skin necrosis and allergic reactions occur rarely. Several cases of anaphylactic reactions and immune thrombocytopenia (type II) associated with arterial and/or venous thrombosis or thromboembolism have been reported.
Interaction
Interaction
Increased risk of developing hyperkalemia with simultaneous use of Fraxiparine: the risk of developing hyperkalemia increases with the use of Fraxiparine in patients receiving potassium salts, potassium-sparing diuretics, ACE inhibitors, angiotensin II receptor antagonists, NSAIDs, heparins (low molecular weight or unfractionated), cyclosporine and tacrolimus, trimethoprim.
Potentiation of action when using fraxiparine: Fraxiparine can potentiate the effect of drugs that affect hemostasis, such as acetylsalicylic acid and other NSAIDs, vitamin K antagonists, fibrinolytics and dextran, platelet aggregation inhibitors (except acetylsalicylic acid as an analgesic and antipyretic drug, i.e. in a dose of more than 500 mg; NSAIDs): abciximab, acetylsalicylic acid as an antiplatelet agent (i.e. at a dose of 50-300 mg) for cardiac and neurological indications, beraprost, clopidogrel, eptifibatide, iloprost, ticlopidine, tirofiban increase the risk of bleeding.
Overdose
Overdose
Symptoms: the main sign of overdose is bleeding; it is necessary to monitor the number of platelets and other parameters of the blood coagulation system.
Treatment: minor bleeding does not require special therapy (usually it is enough to reduce the dose or delay subsequent administration). Protamine sulfate has a pronounced neutralizing effect on the anticoagulant effects of heparin, however, in some cases, anti-Xa activity may be partially restored.
The use of protamine sulfate is necessary only in severe cases. It should be taken into account that 0.6 ml of protamine sulfate neutralizes about 950 anti-Xa ME of nadroparin.
The dose of protamine sulfate is calculated taking into account the time elapsed after the administration of heparin, with a possible reduction in the dose of the antidote.
Storage conditions
Storage conditions
The drug should be stored out of the reach of children, away from heating devices at a temperature not exceeding 30°C;
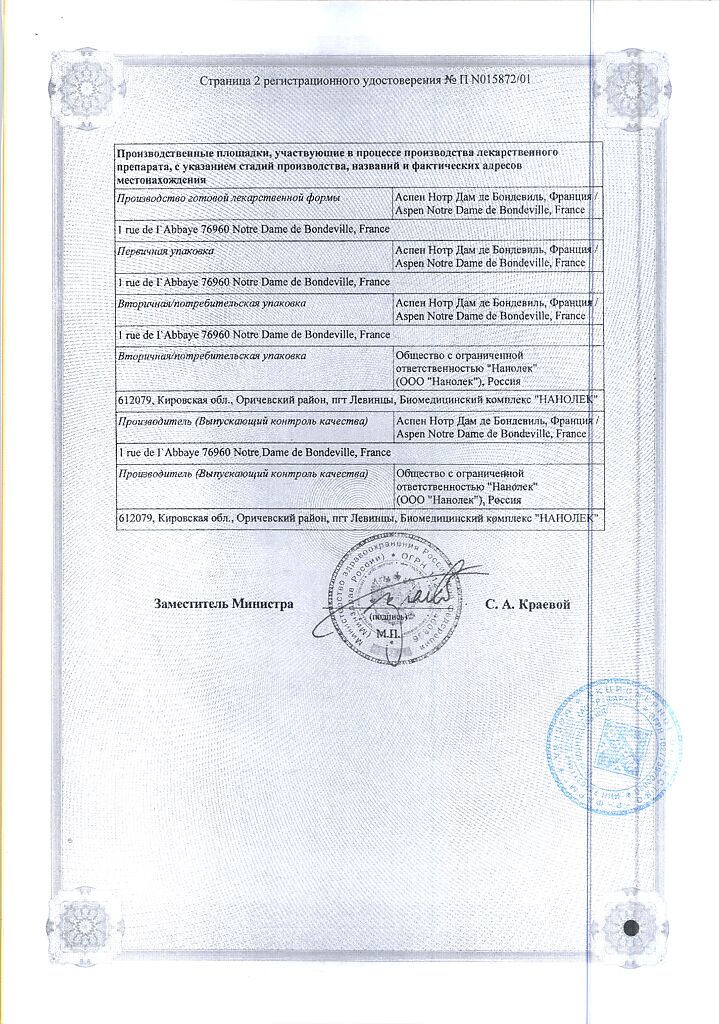
Manufacturer
Manufacturer
Aspen Pharma Trading Limited, Ireland
Additional information
| Conditions of storage | The drug should be kept out of reach of children, away from heaters at a temperature not exceeding 30°C; |
|---|---|
| Manufacturer | Aspen Pharma Trading Limited, Ireland |
| Medication form | solution |
| Brand | Aspen Pharma Trading Limited |
Related products
Buy Frauxiparin, 9,500 anti-ha me/ml 0.3 ml syringes 10 pcs with delivery to USA, UK, Europe and over 120 other countries.