No products in the cart.
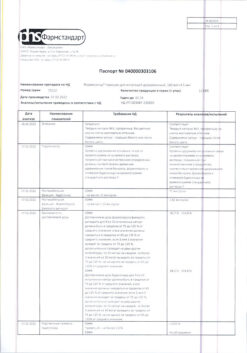
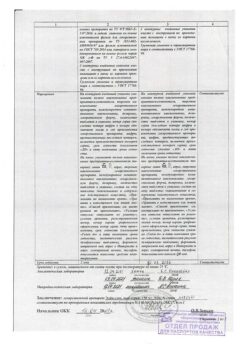
Foster, aerosol 100 mcg+6 mcg/dose 120 doses
€61.80 €51.50
Description
Foster contains beclomethasone dipropionate and formoterol, which have different mechanisms of action and have an additive effect in reducing the frequency of exacerbations of bronchial asthma.
Beclomethasone dipropionate is an inhaled GKS at recommended doses that has anti-inflammatory effects, reduces asthma symptoms, and decreases the frequency of exacerbations, with a lower frequency of side effects than systemic GKS.
Formoterol is a selective β2-adrenoreceptor agonist that causes relaxation of bronchial smooth muscle in patients with reversible airway obstruction. Bronchodilator effect comes on quickly, within 1-3 min after inhalation, and lasts for 12 h after inhalation of a single dose.
The addition of formoterol to beclomethasone dipropionate reduces the severity of bronchial asthma symptoms, improves measures of external respiratory function (ERF) and reduces the frequency of exacerbations of the disease.
In a clinical trial, it was shown that the effect on BPF of the fixed Foster combination was equal to that of the combination of beclomethasone dipropionate and formoterol monotherapy and exceeded that of beclomethasone dipropionate alone.
Pharmacokinetics
Pharmacokinetic parameters for the respective drugs were comparable after administration of beclomethasone dipropionate (BDP) and formoterol as monopreparations and as part of a combination drug.
For beclomethasone dipropionate, the AUC for its active metabolite beclomethasone-17-monopropionate and plasma Cmax values are slightly lower when administered as part of a combination drug, and absorption is faster than for beclomethasone dipropionate monopreparation.
For formoterol, when administered as part of the combination drug, the Cmax in plasma was the same as that of the monodrug, and the systemic effect was slightly higher than that of the monodrug.
There are no data regarding pharmacokinetic or pharmacodynamic interactions between BDP and formoterol: BDP is converted by esterase to the active metabolite beclomethasone-17-monopropionate (B-17 MP).
Inhaled BDP is rapidly absorbed by the lungs; its absorption is preceded by intense conversion of BDP to its active metabolite beclomethasone-17-monopropionate (B-17 MP). Systemic bioavailability (B-17 MP) is 36% due to the lungs and also due to gastrointestinal absorption of the swallowed portion of the inhaled dose. The bioavailability of ingested BDP is negligible; however, the presystemic conversion of BDP to B-17 MP results in 41% of BDP being absorbed by the body as B-17 MP. There is an almost linear increase in systemic action with increasing inhaled dose. The absolute bioavailability after inhalation is approximately 2% and 62% of the nominal dose relative to unchanged BDP u and B-17 MP, respectively.
The binding to plasma proteins is quite high.
Metabolism
BDP is characterized by a very high clearance rate from the great circle of the circulation due to the action of esterase present in most tissues. The main metabolic product of BDP is the active metabolite B-17 MP. Less active metabolites are beclomethasone 21 monopropionate (B-21 MP) and beclomethasone (BON), which are also produced by metabolism, but their role in the systemic effects of BDP is very minor.
The bulk of BDP is excreted in the feces as polar metabolites. Renal excretion of BDP and its metabolites is insignificant. T1/2 of BDP and B-17 MP is 0.5 and 2.7 h, respectively.
Pharmacokinetics in special clinical cases
. Hepatic insufficiency does not alter the pharmacokinetic properties and safety profile of BDP due to the fact that the latter undergoes rapid metabolism to the polar metabolites B-21 MP, BON and B-17 MP under the action of enzymes present in the gastrointestinal tract, blood plasma, lungs and liver.
The pharmacokinetic properties of BDP in patients with renal impairment have not been studied. Taking into account that both BDP and its metabolites are practically not excreted with urine, there is no reason to assume increased systemic action of the drug in patients suffering from renal failure.
Formoterol
Intake and distribution
Inhaled formoterol is absorbed in the lungs and GI tract. The portion of the inhaled dose that is swallowed depends on the type of inhalation device. and inhalation technique. So when using a multi-dose inhaler, it can be up to 90%. Therefore, the swallowed fraction must be taken into account when using the inhalation technique.
No less than 65% of the oral dose of formoterol is absorbed through the gastrointestinal tract, with 70% of this volume undergoing presystemic metabolism. Cmax of unchanged formoterol in plasma is observed within 0.5-1 h after oral administration. The plasma protein binding of formoterol is 61-64%, with an affinity to albumin of 34%. No affinity is observed in the range of therapeutic doses. When administered orally, the T1/2 is 2-3 h. With inhalation of 12-96 mcg formoterol fumarate, the absorption of formoterol is linear.
Metabolism
The metabolism of formoterol is carried out, in particular, by direct conjugation of the phenol hydroxyl group.
Glucuronic acid conjugates are not active. The second significant pathway of formoterol metabolism is O-dimethylation by conjugation at the level of the phenol-2-hydroxyl group. The cytochrome P450 enzymes CYP2D6, CYP2C9, and CYP2C19 are involved in the O-demethylation of formoterol. There is reason to believe that the metabolism of formoterol takes place mainly in the liver. Formoterol does not inhibit CYP450 enzymes at therapeutically significant concentrations.
The total renal excretion of formoterol after inhalation of a single dose via a metered-dose powder inhaler increases linearly in the dose range of 12-96 mcg. The excretion rates of unchanged and total formoterol averaged 8% and 25%, respectively. Based on measurements of plasma concentrations of formoterol after its single inhalation at a dose of 120 mcg in 12 healthy volunteers, the T1/2 was determined to be 10 h. The ratio of (R,R)- and (S,S)-enantiomers of the unchanged drug in renal excretion was 40% and 60%, respectively. The relative ratios of these 2 parameters do not change over the range of doses studied; there is no evidence of accumulation of one enantiomer relative to the other after administration, repeated doses.
In healthy volunteers, after oral administration (40-80 mcg), 6-10% of the dose was detected in the urine as unchanged drug; 8% of the dose was present as glucuronides.
Only 67% of the oral dose of formoterol is excreted by the kidneys (mainly as metabolites); the rest of the dose is excreted through the intestine. Renal clearance of formoterol is 150 ml/min.
Indications
Indications
Basic therapy for bronchial asthma, involving the prescription of combination therapy (inhaled glucocorticosteroid and long-acting β 2 adrenergic agonist):
– Patients whose symptoms are not sufficiently controlled by inhaled glucocorticosteroids and short-acting β 2 adrenergic agonists.
– Patients receiving effective maintenance doses of inhaled glucocorticosteroids and long-acting β 2 adrenergic agonists.
Pharmacological effect
Pharmacological effect
Foster contains beclomethasone dipropionate and formoterol, which have different mechanisms of action and exhibit an additive effect in reducing the frequency of exacerbations of bronchial asthma.
Beclomethasone dipropionate is an inhaled corticosteroid, in recommended doses it has an anti-inflammatory effect, reduces the severity of symptoms of bronchial asthma and reduces the frequency of exacerbations of the disease, while having a lower frequency of side effects than systemic corticosteroids.
Formoterol is a selective β2-adrenergic receptor agonist that causes relaxation of bronchial smooth muscle in patients with reversible airway obstruction. The bronchodilator effect occurs quickly, within 1-3 minutes after inhalation, and persists for 12 hours after inhalation of a single dose.
The addition of formoterol to beclomethasone dipropionate reduces the severity of symptoms of bronchial asthma, improves respiratory function (RVP) and reduces the frequency of exacerbations of the disease.
During the clinical study, it was shown that the effect on FVD of the fixed combination Foster corresponds to that of the combination of beclomethasone dipropionate and formoterol monotherapy and exceeds the effect of beclomethasone dipropionate alone.
Pharmacokinetics
Pharmacokinetic parameters for the respective drugs were comparable after the administration of beclomethasone dipropionate (BDP) and formoterol in the form of single agents and as part of a combination drug.
For beclomethasone dipropionate, when administered as part of a combination drug, the AUC for its active metabolite beclomethasone-17-monopropionate and the Cmax value in plasma are slightly lower, and absorption is faster than that of the single drug beclomethasone dipropionate.
For formoterol, when administered as part of a combination drug, Cmax in plasma coincided with that for the single drug, and the systemic effect was slightly higher than that of the single drug.
No data have been obtained regarding the pharmacokinetic or pharmacodynamic interaction between BDP and formoterol: BDP is converted by esterase to the active metabolite beclomethasone-17-monopropionate (B-17 MP).
Inhaled BDP is quickly absorbed by the lungs; its absorption is preceded by intense conversion of BDP to its active metabolite beclomethasone-17-monopropionate (B-17 MP). Systemic bioavailability (B-17 MP) is ensured by 36% due to the lungs, as well as due to the absorption of the ingested part of the inhalation dose by the gastrointestinal tract. The bioavailability of ingested BDP is negligible; however, the presystemic conversion of BDP to B-17 MP results in 41% of BDP being absorbed by the body as B-17 MP. There is an almost linear increase in systemic effect with increasing inhalation dose. Absolute bioavailability after inhalation is about 2% and 62% of the nominal dose relative to unchanged BDP and B-17 MP, respectively.
Plasma protein binding is quite high.
Metabolism
BDP is characterized by a very high rate of clearance from the systemic circulation due to the action of esterase present in most tissues. The main metabolic product of BDP is the active metabolite B-17 MP. Less active metabolites are beclomethasone 21 monopropionate (B-21 MP) and beclomethasone (BON), which are also formed as a result of metabolism, but their role in the systemic effects of BDP is very minor.
Removal
The main part of BDP is excreted in the feces in the form of polar metabolites. Renal excretion of BDP and its metabolites is negligible. T1/2 of BDP and B-17 MP is 0.5 and 2.7 hours, respectively.
Pharmacokinetics in special clinical situations
Liver failure does not lead to a change in the pharmacokinetic properties and safety profile of BDP due to the fact that the latter undergoes rapid metabolism to polar metabolites B-21 MP, BON and B-17 MP under the action of enzymes present in the gastrointestinal tract, blood plasma, lungs and liver.
The pharmacokinetic properties of BDP in patients suffering from renal failure have not been studied. Taking into account that both BDP and its metabolites are practically not excreted in the urine, there is no reason to assume an increase in the systemic effect of the drug on the body of patients suffering from renal failure.
Formoterol
Suction and distribution
Inhaled formoterol is absorbed in the lungs and gastrointestinal tract. The portion of the inhalation dose that is swallowed depends on the type of inhalation device. and inhalation techniques. So, when using a multi-dose metered dose inhaler, it can be up to 90%. Therefore, the ingested fraction must be taken into account when administering the drug by inhalation.
At least 65% of an oral dose of frmoterol is absorbed through the gastrointestinal tract, with 70% of this volume undergoing first-pass metabolism. Cmax of unchanged formoterol in blood plasma is observed within 0.5-1 hour after oral administration. Formoterol’s binding to plasma proteins is 61-64%, while the affinity for albumin is 34%. In the therapeutic dose range, affinity saturation is not observed. When taken orally, T1/2 is 2-3 hours. When inhaled 12-96 mcg of formoterol fumarate, the absorption of formoterol is linear.
Metabolism
Formoterol is metabolized, in particular, through direct conjugation of the phenolhydroxyl group.
Glucuronic acid conjugates are not active. The second significant pathway of formoterol metabolism is O-dimethylation through conjugation at the level of the phenol-2-hydroxyl group. Cytochrome P450 of the enzymes CYP2D6, CYP2C9, CYP2C19 is involved in the O-demethylation of formoterol. There is reason to believe that formoterol is metabolized primarily in the liver. Formoterol does not inhibit CYP450 enzymes at therapeutically relevant concentrations.
Removal
Cumulative renal excretion of formoterol following single dose inhalation via a metered dose inhaler increases linearly over the dose range of 12-96 mcg. Excretion rates of unchanged and total formoterol average 8% and 25%, respectively. Based on measurements of plasma concentrations of formoterol after a single inhalation at a dose of 120 mcg in 12 healthy volunteers, T1/2 was determined, which was 10 hours. The ratio of (R,R)- and (S,S)-enantiomers of the unchanged drug during renal excretion is 40% and 60%, respectively. The relative ratio of these 2 indicators does not change in the range of dosages studied; there is no evidence of accumulation of one enantiomer relative to the other after administration or repeated dosing.
In healthy volunteers, after oral administration (40-80 mcg), 6-10% of the dose was found in the urine as unchanged drug; 8% of the dose was present as glucuronides.
Only 67% of the oral dose of formoterol is excreted by the kidneys (mainly in the form of metabolites), the rest of the dose is excreted through the intestines. The renal clearance of formoterol is 150 ml/min.
Special instructions
Special instructions
If patients have concomitant diseases such as coronary artery disease, myocardial infarction, exacerbation of arterial hypertension, cardiac arrhythmias, chronic heart failure, diabetes mellitus, prostatic hypertrophy, glaucoma, special care must be taken when choosing the dose of Foster.
Precautions should be taken when treating patients with a prolonged QTc interval (QTc >0.44 sec.). Taking formoterol may cause a prolongation of the QTc interval. Foster should only be used in patients with tachyarrhythmia if special precautions are taken, such as ECG monitoring.
Special precautions should be taken in patients with unstable bronchial asthma using short-acting bronchodilators to relieve attacks during exacerbation of severe bronchial asthma, because risk
the development of hypokalemia increases against the background of hypoxia and in other conditions when the likelihood of developing a hypokalemic effect increases. In such cases, it is recommended to monitor serum potassium levels.
Inhalation of high doses of formoterol may lead to increased blood glucose levels. During treatment, blood glucose concentrations should be monitored in patients with diabetes mellitus. If anesthesia is planned
preparations of halogenated hydrocarbons, it is necessary to warn the patient not to use Foster for 12 hours before starting anesthesia.
As with the appointment of other corticosteroids, the need for use and dose of Foster should be reconsidered in patients with active or inactive forms of pulmonary tuberculosis, fungal, viral or bacterial infections of the respiratory system.
Due to the risk of exacerbation, treatment with Foster should not be stopped abruptly; the dose of the drug should be reduced gradually and under the supervision of a physician.
When patients are already undergoing this course of treatment (inhaled or oral corticosteroids), it should be continued without any changes, even if improvement in symptoms is observed.
The persistence of symptoms of bronchial asthma or the need to increase the dose of Foster may indicate a worsening of bronchial asthma and the need to review treatment. To relieve acute attacks of bronchospasm, patients are recommended to constantly carry short-acting beta2-adrenergic agonists with them.
Treatment with Foster should not be prescribed during an exacerbation of bronchial asthma.
As with any other inhalation therapy, paradoxical bronchospasm may occur with immediate
increased wheezing after taking a dose of the drug. In this regard, Foster therapy should be discontinued, treatment tactics should be reconsidered and, if necessary, alternative therapy should be prescribed.
Any inhaled GCS can cause systemic effects, especially with long-term use in high doses; It should be noted, however, that the likelihood of developing such symptoms is much lower than with treatment with oral corticosteroids. Possible systemic effects include adrenal suppression, growth retardation in children and adolescents, decreased bone mineral density, cataracts, and glaucoma. Considering the above, the dose of inhaled GCS should be titrated to the minimum that will ensure the maintenance of effective control.
With chronic use of excessive doses of beclomethasone dipropionate, its systemic effect may occur: significant suppression of the adrenal cortex may occur, up to an adrenal crisis. Adrenal crisis is manifested by anorexia, abdominal pain, weight loss, fatigue, headache, nausea, vomiting, hypotension, hypoglycemia, accompanied by confusion and/or convulsions. Situations that may trigger an acute adrenal crisis include trauma, surgery, infection, or
rapid reduction in the dose of beclomethasone included in Foster. In case of chronic overdose, it is recommended to monitor the reserve function of the adrenal cortex.
If there is reason to believe that adrenal function has been impaired due to previous systemic GCS therapy, precautions should be taken when transferring patients to treatment with Foster.
The benefits of inhaled therapy generally minimize the need for oral corticosteroids, but patients who discontinue oral corticosteroids may experience long-term adrenal insufficiency. Patients who in the past required acute use of high doses of corticosteroids or received long-term treatment with high-dose inhaled corticosteroids may also be at this risk.
It is necessary to provide additional administration of GCS during periods of stress or surgery.
It is recommended to instruct the patient to rinse the mouth with water after inhaling maintenance doses in order to prevent the risk of developing candidiasis of the oral and pharyngeal mucosa.
The cylinder is under pressure: do not expose it to high temperatures, do not pierce it, do not throw it into fire, even when empty. Use within 3 months from the start of use.
Active ingredient
Active ingredient
Beclomethasone, Formoterol
Composition
Composition
1 dose of the drug contains:
Pregnancy
Pregnancy
There is no clinical data on the use of Foster during pregnancy. No embryotoxic or teratogenic effects were detected in animal studies.
During pregnancy, Foster should be used only in cases where the benefits of using the drug outweigh the potential risk to the fetus. It is recommended to prescribe the minimum dose that provides effective control of asthma symptoms.
There is no data on the penetration of Foster into women’s breast milk. Foster can be prescribed to nursing women only in cases where the expected therapeutic effect for the mother outweighs the potential risk for the child.
Contraindications
Contraindications
Hypersensitivity to Foster’s components, children under 18 years of age.
With caution:
Pregnancy, lactation, pulmonary tuberculosis, fungal, viral or bacterial infections of the respiratory system, thyrotoxicosis, pheochromocytoma, diabetes mellitus, uncontrolled hypokalemia, idiopathic hypertrophic subaortic stenosis, third degree atrioventricular block, severe arterial hypertension, aneurysm of any location or other severe cardiovascular diseases (acute infarction myocardium, coronary heart disease, tachyarrhythmia, decompensated chronic heart failure, prolonged QTc interval (taking formoterol may cause prolongation of the QTc interval)).
Side Effects
Side Effects
Foster contains beclomethasone dipropionate and formoterol fumarate, and therefore it is expected that it may cause side effects characteristic of these components. There is no evidence that their simultaneous use causes additional side effects.
Side effects associated with the use of beclomethasone dipropionate and formoterol as a fixed combination (Foster) are presented below.
From the side of the central nervous system: often – headache.
From the respiratory system: often – hoarseness; less often – rhinitis, dysphonia, cough, mild irritation in the throat, bronchospasm.
From the cardiovascular system: less often – palpitations, prolongation of the QT interval, ECG changes.
From the musculoskeletal system: tremor, muscle cramps.
From the hematopoietic system: granulocytopenia, increased platelet count.
From the digestive system: dry mouth, burning sensation in the lips, dysphagia, dyspepsia, diarrhea.
From the immune system: allergic dermatitis; increase in C-reactive protein.
Metabolic disorders: hypokalemia.
Infections: pharyngitis, influenza, candidiasis of the oral mucosa, pharynx and esophagus, vaginal candidiasis, gastroenteritis, sinusitis.
Among the most common side effects associated with taking formoterol, those typical of beta2-agonists are described, such as hypokalemia, headache, tremor, palpitations, cough, muscle cramps, and prolongation of the QTc interval.
Side effects characteristic of beclomethasone dipropionate: candidiasis of the oral mucosa and pharynx, irritation in the throat.
Like other inhaled drugs, Foster can cause paradoxical bronchospasm.
Other side effects characteristic of formoterol: thrombocytopenia, angioedema, hyperglycemia, increased blood levels of insulin, free fatty acids, glycerol and ketone derivatives, sleep disturbances, hallucinations, fatigue, anxiety, changes in taste (dysgeusia), tachycardia, tachyarrhythmia, ventricular extrasystole, angina pectoris, atrial fibrillation, arterial hypertension, arterial hypotension, exacerbation of bronchial asthma, shortness of breath, nausea, itching, skin rash, urticaria, hyperhidrosis, myalgia, nephritis, peripheral edema.
Systemic effects of corticosteroids (including beclomethasone dipropionate) occur when high doses are prescribed for a long time. These include: adrenal suppression, decreased bone mineral density, growth retardation in children and adolescents, glaucoma and cataracts.
Hypersensitivity reactions include: itching, skin rash, erythema and swelling of the eyes, face, lips and throat.
Interaction
Interaction
Beta-adrenergic blockers may reduce the effect of formoterol. Foster should not be prescribed simultaneously with beta-blockers (including eye drops), except in cases of emergency.
When taken together, Foster and other beta-adrenergic drugs may increase the side effects of formoterol.
Co-administration of Foster and quinidine, disopyramide, procainamide, phenothiazines, antihistamines (terfenadine), MAO inhibitors and tricyclic antidepressants may prolong the QTc interval and increase the risk of ventricular arrhythmias.
In addition, levodopa, levothyroxine, oxytocin and alcohol can reduce the tolerance of the heart muscle to beta2-agonists.
Co-administration of MAO inhibitors, as well as drugs with similar properties, such as furazolidone and procarbazine, may cause an increase in blood pressure.
There is an increased risk of developing arrhythmias in patients undergoing general anesthesia with halogenated hydrocarbon preparations.
As a result of the use of beta2-adrenergic agonists, hypokalemia may occur, which may increase with concomitant treatment with xanthine derivatives, mineral derivatives of corticosteroids, and diuretics. Hypokalemia may increase the susceptibility to the development of arrhythmias in patients taking cardiac glycosides.
Due to the small amount of ethanol contained, an interaction may occur in hypersensitive patients taking disulfiram or metronidazole.
Overdose
Overdose
Symptoms: in case of overdose, symptoms typical of beta2-adrenergic agonists occur due to formoterol, such as nausea, vomiting, headache, tremor, drowsiness, palpitations, tachycardia, ventricular arrhythmia, prolongation of the QTc interval, metabolic acidosis, hypokalemia, hyperglycemia.
Treatment: symptomatic treatment. In severe cases, hospitalization. The use of cardioselective beta-blockers may be considered with caution as these agents may cause bronchospasm. It is necessary to monitor the level of potassium in the blood plasma.
Inhalation of doses of beclomethasone dipropionate higher than recommended may cause temporary inhibition of adrenal function. This usually does not require any emergency measures, since in most cases normal adrenal function is restored within a few days. It is recommended to monitor plasma cortisol levels.
With chronic use of excessive doses of beclomethasone dipropionate, its systemic effect may occur: significant suppression of the adrenal cortex may occur, up to an adrenal crisis. Acute adrenal crisis is characterized by hypoglycemia, accompanied by confusion and/or convulsions. Situations that can serve as triggers for acute adrenal crisis include trauma, surgery, infection, or a rapid reduction in the dose of beclomethasone included in Foster. In case of chronic overdose, it is recommended to monitor the reserve function of the adrenal cortex.
Storage conditions
Storage conditions
In a place protected from direct sunlight, away from heating devices, at a temperature of 2–8 °C
Shelf life
Shelf life
18 months
Manufacturer
Manufacturer
Chiesi Pharmaceuticals S.p.A., Italy
Additional information
| Shelf life | 18 months |
|---|---|
| Conditions of storage | Protected from direct sunlight, away from heaters, at 2-8 °C |
| Manufacturer | Chiesi Pharmaceutici S.p.A., Italy |
| Medication form | metered aerosol for inhalation |
| Brand | Chiesi Pharmaceutici S.p.A. |
Related products
Buy Foster, aerosol 100 mcg+6 mcg/dose 120 doses with delivery to USA, UK, Europe and over 120 other countries.