No products in the cart.
Flixotide, aerosol 250 mcg/dose 60 doses
€56.70 €49.14
Description
Flixotide is a glucocorticoid drug for inhalation use.
In recommended doses it has a pronounced anti-inflammatory effect, which helps to reduce the severity of symptoms, frequency and severity of exacerbations of diseases accompanied by airway obstruction (bronchial asthma, chronic bronchitis, emphysema).
The systemic effect of the drug is minimal. In therapeutic doses Flixotide has practically no effect on the hypothalamic-pituitary-adrenal system.
Indications
Indications
– basic anti-inflammatory therapy for bronchial asthma (including in severe cases of the disease and dependence on systemic corticosteroids) in adults and children over 1 year of age
– treatment of chronic obstructive pulmonary disease (including chronic bronchitis and emphysema).
Pharmacological effect
Pharmacological effect
FLIXOTIDE is a glucocorticoid drug for inhalation use.
In recommended doses, it has a pronounced anti-inflammatory effect, which helps reduce the severity of symptoms, frequency and severity of exacerbations of diseases accompanied by airway obstruction (bronchial asthma, chronic bronchitis, emphysema).
The systemic effect of the drug is minimal. In therapeutic doses, Flixotide has virtually no effect on the hypothalamic-pituitary-adrenal system.
Special instructions
Special instructions
Flixotide is intended for the long-term treatment of bronchial asthma, and not for the relief of attacks. To relieve attacks, patients should be prescribed short-acting inhaled bronchodilators.
If the effectiveness of short-acting bronchodilators decreases or if more frequent use is necessary, the patient should consult a doctor.
An increased need for the use of short-acting inhaled beta2-adrenergic agonists indicates a worsening of the disease. In such cases, it is recommended to reconsider the patient’s treatment plan.
A sudden and progressive deterioration of bronchial asthma can pose a threat to the patient’s life, so in such situations it is necessary to urgently address the issue of increasing the dose of GCS.
Abruptly stopping treatment with Flixotide is not recommended.
Particular care should be taken when treating patients with active or inactive forms of pulmonary tuberculosis with inhaled corticosteroids.
In case of severe exacerbation of bronchial asthma or insufficient effectiveness of the therapy, the dose of inhaled fluticasone propionate should be increased and, if necessary, a drug from the group of systemic corticosteroids and/or an antibiotic should be prescribed if the infection develops.
It is recommended to check whether the patient knows how to use the inhaler correctly.
With long-term use of any inhaled corticosteroids, especially in high doses, systemic effects may be observed, but the likelihood of their development is much lower than when taking corticosteroids orally. Possible systemic effects include decreased adrenal function, osteoporosis, growth retardation in children, cataracts, and glaucoma. Therefore, it is especially important that when a therapeutic effect is achieved, the dose of inhaled corticosteroids is reduced to the minimum effective dose that controls the course of the disease.
The transfer of patients suffering from hormone-dependent bronchial asthma from systemic corticosteroids to inhaled fluticasone requires special attention, since restoration of adrenal function takes a long time. Adrenal cortex function should be regularly monitored and caution should be exercised when reducing the dose of systemic corticosteroids.
A gradual reduction in the dose of systemic corticosteroids can begin approximately one week after the appointment of fluticasone. With a maintenance dose of prednisolone (or other corticosteroids in an equivalent dose) less than 10 mg/day. the dose reduction should not exceed 1 mg/day. and should be carried out at intervals of at least 1 week. With a maintenance dose of prednisolone more than 10 mg/day. (calculated per day) – in high doses, also at intervals of at least 1 week.
Some patients, during the period of reducing the dose of systemic corticosteroids, complain of general malaise against the background of stabilization or even improvement of respiratory function indicators. If there are no objective signs of adrenal insufficiency, patients should be persuaded to continue switching to inhaled GCS and gradual withdrawal of systemic GCS.
In some cases, individual high sensitivity to inhaled corticosteroids may be observed. The function of the adrenal cortex when prescribing fluticasone propionate in recommended doses, as a rule, remains within normal limits. The advantages of inhaled fluticasone propionate minimize the need for systemic corticosteroids. However, there may remain a possibility of developing side effects in patients who have previously received or periodically take GCS orally. During resuscitation or surgery, consultation with a specialist may be required to determine the degree of adrenal insufficiency. In such stressful situations, one should always take into account possible adrenal insufficiency and, if necessary, additionally prescribe corticosteroids.
Due to possible adrenal insufficiency, special caution should be exercised and regular monitoring of adrenal function indicators when transferring patients who have taken oral corticosteroids to treatment with inhaled fluticasone propionate. Discontinuation of systemic corticosteroids during inhaled fluticasone propionate should be gradual, and patients should carry a card indicating that they may require additional corticosteroids during periods of stress.
In rare cases, when transferring patients from taking systemic corticosteroids to inhaled therapy, conditions accompanied by hypereosinophilia (for example, Churg-Strauss syndrome) may occur. As a rule, this occurs during dose reduction or withdrawal of systemic corticosteroids, but a direct cause-and-effect relationship has not been established.
When transferring patients from taking systemic corticosteroids to inhalation therapy, concomitant allergic diseases (for example, allergic rhinitis, eczema), which were previously suppressed by systemic drugs, may also worsen. In such situations, it is recommended to carry out symptomatic treatment with antihistamines and/or topical drugs, incl. GCS for local use.
To prevent the development of candidiasis, you should rinse your mouth after using Flixotide; If necessary, local antifungal therapy can be prescribed throughout the entire treatment period.
To prevent hoarseness, it is recommended to rinse your mouth and throat with water immediately after inhalation.
If paradoxical bronchospasm develops, you should immediately stop administering Flixotide, assess the patient’s condition, conduct the necessary examination and, if necessary, prescribe other medications. Paradoxical bronchospasm should be treated immediately with a fast-acting inhaled bronchodilator.
There are very rare reports of increased blood glucose levels, and this should be kept in mind when prescribing fluticasone propionate to patients with diabetes mellitus.
Like most other inhalation aerosol products, this product may be less effective if the canister is refrigerated.
Use in pediatrics
The growth dynamics of children receiving inhaled corticosteroids for a long time should be regularly monitored.
Impact on the ability to drive vehicles and operate machinery
The effect of fluticasone propionate on the ability to drive a car and operate machinery is unlikely.
Active ingredient
Active ingredient
Fluticasone
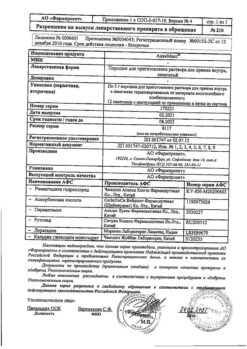
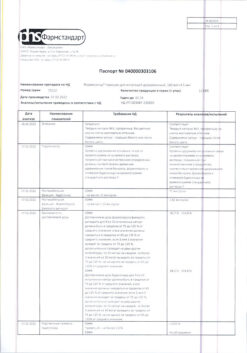
Composition
Composition
1 dose contains fluticasone 250 mcg,
excipients:
propellant tetrafluoroethane GR106642X (the product does not contain freon).
Contraindications
Contraindications
Hypersensitivity to the components of the drug.
Side Effects
Side Effects
Candidiasis of the oral cavity and pharynx, hoarseness (after inhalation it is necessary to rinse the mouth and throat with water), paradoxical bronchospasm (requires discontinuation of the drug and continuation of therapy with other means);
rarely – the development of allergic reactions (skin rash, angioedema, dyspnea or bronchospasm, anaphylactic reactions); Possible decreased function of the adrenal cortex, osteoporosis, growth retardation in children, cataracts, increased intraocular pressure.
Interaction
Interaction
Since fluticasone propionate plasma concentrations are very low when administered via inhalation, interaction with other drugs is unlikely.
With the simultaneous use of fluticasone propionate and CYP3A4 enzyme inhibitors (for example, ketoconazole, ritonavir), the systemic effect of Flixotide may be enhanced (the use of such a combination requires caution).
Overdose
Overdose
An acute overdose of the drug can lead to a temporary decrease in the function of the adrenal cortex, which usually does not require emergency treatment, because the function of the adrenal cortex is restored within a few days.
If Flixotide is taken in high doses for a long time, significant suppression of adrenal function is possible. Very rare reports have been received of the development of adrenal crisis in children receiving fluticasone propionate at a dose of 1 mg/day. and higher for several months or years. Such patients experienced hypoglycemia, depression of consciousness and convulsive states.
Acute adrenal crisis can develop against the background of the following conditions: severe trauma, surgery, infection, sharp reduction in the dose of fluticasone propionate.
In cases where the patient receives a dose higher than recommended, it should be gradually reduced.
Storage conditions
Storage conditions
In a place protected from light, at a temperature not exceeding 25°C.
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
Glaxo Wellcome S.A., Spain
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a place protected from light, at a temperature not exceeding 25°C. |
| Manufacturer | Glaxo Wellcome S.A., Spain |
| Medication form | metered aerosol for inhalation |
| Brand | Glaxo Wellcome S.A. |
Other forms…
Related products
Buy Flixotide, aerosol 250 mcg/dose 60 doses with delivery to USA, UK, Europe and over 120 other countries.