No products in the cart.
Flamadex, 25 mg 10 pcs
€13.50 €11.25
Description
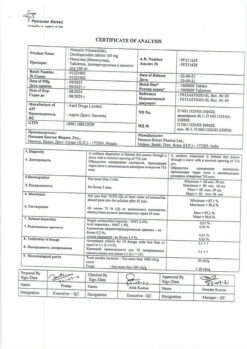
Pharmacoherapeutic group: non-steroidal anti-inflammatory drug CodeATX: M01AE17 Pharmacological action Pharmacodynamics
Dexketoprofen trometamol, the active substance of Flamadex? refers to non-steroidal anti-inflammatory drugs (NSAIDs) with analgesic, anti-inflammatory and antipyretic effects. The mechanism of action of Dexectoprofen is based on inhibition of proglacidin synthesis at the level of cyclooxygenase (COX-1 and COX-2).
The analgesic effect comes within 30 minutes after oral administration of the drug, therapeutic effect lasts for 4-6 hours.
Pharmacokinetics
Intake
The time of reaching the maximum concentration (TStah) of dexketoprofen in blood plasma after a single oral single dose is on average 30 min (15-60 min). Simultaneous intake of food slows down absorption of dexketoprofen. Areas under the curve “concentration-time” (AUC) after a single and repeated intake are similar, which indicates the absence of cumulation of the drug.
Distribution
Dexketoprofen is characterized by high degree of binding to plasma proteins (99 %). Mean volume of distribution (Vd) is less than 0.25 l/kg, period of half-distribution is approximately 0.35 h.
Metabolism and excretion
The main way of dexketoprofen metabolism is its conjugation with glucuronic acid with subsequent excretion by the kidneys. The potency period (Tie) of dexketoprofen is 1.65 h. In elderly patients there is prolongation of Tie up to 48 % and decrease of total clearance of the drug.
Indications
Indications
Musculoskeletal pain (mild or moderate), algodismenorrhea, toothache.
The drug is intended for symptomatic therapy, reducing pain and inflammation at the time of use.
Pharmacological effect
Pharmacological effect
Pharmacoherapeutic group: non-steroidal anti-inflammatory drug CodeATX: M01AE17 Pharmacological action Pharmacodynamics
Dexketoprofen trometamol, the active ingredient in Flamadex? refers to non-steroidal anti-inflammatory drugs (NSAIDs), which have analgesic, anti-inflammatory and antipyretic effects. The mechanism of action of dexketoprofen is based on inhibition of the synthesis of prosgaglacdins at the level of cyclooxygenases (COX-1 and COX-2).
The analgesic effect occurs 30 minutes after taking the drug orally, the duration of the therapeutic effect is 4-6 hours.
Pharmacokinetics
Suction
The time to reach the maximum concentration (TCmax) of dexketoprofen in the blood plasma after a single oral dose averages 30 minutes (15-60 minutes). Concomitant food intake slows down the absorption of dexketoprofen. The areas under the concentration-time curve (AUC) after single and repeated doses are similar, indicating the absence of drug accumulation.
Distribution
Dexketoprofen is characterized by a high degree of binding to plasma proteins (99%). The average volume of distribution (Vd) is less than 0.25 l/kg, the half-life is about 0.35 hours.
Metabolism and excretion
The main route of metabolism of dexketoprofen is its conjugation with glucuronic acid, followed by excretion by the kidneys. The elimination period (Tie) of dexketoprofen is 1.65 hours. In elderly people, an increase in Tie up to 48% and a decrease in the overall clearance of the drug are observed.
Special instructions
Special instructions
Undesirable side effects can be minimized when using the drug in the lowest effective dose with the minimum duration of use necessary to relieve pain.
The risk of complications from the gastrointestinal tract increases in patients with a history of ulcerative lesions of the gastrointestinal tract, in elderly patients, with an increase in the dose of NSAIDs; therefore, the use of Flamadex in this category of patients should begin with the lowest recommended dose.
Patients in the above categories, as well as patients who require simultaneous use of low doses of acetylsalicylic acid or other drugs that increase the risk of complications from the gastrointestinal tract, are recommended to additionally use gastroprotectors (misoprostol or proton pump blockers).
In patients simultaneously taking antiplatelet agents or anticoagulants, glucocorticosteroids, the risk of gastrointestinal bleeding also increases.
Patients with gastrointestinal disorders or a history of gastrointestinal diseases should be under close medical supervision. In case of gastrointestinal bleeding or ulcerative lesions, use of the drug Flamadex? should be stopped.
The drug Flamadex? should be used with caution in patients with a history of gastrointestinal diseases (ulcerative colitis, Crohn’s disease), since exacerbation of these diseases is possible.
All NSAIDs can inhibit platelet aggregation and prolong bleeding time by inhibiting prostaglandin synthesis. In this regard, the use of the drug Flamadex? It is not recommended for patients simultaneously taking drugs that affect the hemostatic system, such as warfarin, coumarin derivatives and heparins. Like other NSAIDs, is Flamadex? may lead to increased concentrations of creatinine and nitrogen in the blood plasma. Like other prostaglandin synthesis inhibitors, Flamadex? may have side effects on the urinary system, which can lead to the development of glomerulonephritis, interstitial nephritis, papillary necrosis, nephrotic syndrome and acute renal failure. Caution should be exercised when using the drug in patients concomitantly using diuretics and patients who may develop hypovolemia, due to the increased risk of nephrotoxicity.
As with the use of other NSAIDs, during therapy with Flamadex? There may be a slight transient increase in the activity of liver enzymes. In elderly patients, monitoring of liver and kidney function is necessary. In case of a significant increase in the corresponding indicators, the use of Flamadex* should be discontinued.
Like other NSAIDs, dexketoprofen may mask the symptoms of infectious diseases. If signs of infection or deterioration in health are detected while using the drug Flamadex?, the patient should immediately consult a doctor.
The drug can cause fluid retention in the body, so Flamadex* should be used with extreme caution in patients with arterial hypertension, renal and/or heart failure. Should the condition worsen, use the drug Flamadex? must be stopped.”
In patients with uncontrolled arterial hypertension, coronary artery disease, congestive heart failure, peripheral arterial disease and/or cerebrovascular disease, the drug should be used with caution. A similar approach is applicable to patients with risk factors for advanced cardiovascular diseases (arterial hypertension, hyperlipidemia, diabetes mellitus, smoking).
Do you need to be careful when prescribing Flamadex? patients with a history of cardiovascular disease, especially patients with heart failure, due to the possible risk of progression. Clinical studies and epidemiological data suggest that NSAIDs, especially in high doses and with long-term use, may lead to a small risk of acute myocardial infarction or stroke. There is insufficient data to exclude the risk of these events when using dexketoprofen.
Elderly patients are especially susceptible to adverse reactions when using NSAIDs, including the risk of life-threatening gastrointestinal bleeding and perforation, and decreased kidney, liver, and heart function. When using the drug Flamadex? This category of patients requires proper clinical monitoring.
There is evidence of rare cases of skin reactions (such as exopiative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis) with the use of NSAIDs. At the first manifestations of a skin rash, damage to the mucous membranes or other signs of an allergic reaction, should you take Flamadex? you should stop immediately and consult a doctor.
Effect on the ability to drive vehicles and operate machinery Due to the possible occurrence of dizziness and drowsiness during the period of use of dexketoprofen, the ability to concentrate and the speed of psychomotor reactions in patients may decrease, especially in the first hour after administration. Therefore, while using the drug Flamadex? Care should be taken when driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Dexketoprofen
Composition
Composition
Active ingredient: dexketoprofen trometamol – 36.9 mg, in terms of dexketoprofen – 25 mg;
excipients: microcrystalline cellulose, pregelatinized starch, sodium carboxymethyl starch (sodium starch glycolate), magnesium stearate;
shell composition: titanium dioxide, hypromellose (tpromellose 2910), polydextrose, macrogol.
Pregnancy
Pregnancy
The use of Flamadex during pregnancy and during difficult feeding is contraindicated.
Contraindications
Contraindications
hypersensitivity to dexketoprofen, other components of the drug and other NSAIDs;
complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid or other NSAIDs (including a history);
—erosive and ulcerative lesions of the gastrointestinal tract in the acute stage;
—a history of gastrointestinal bleeding or perforation, including those associated with previous use of NSAIDs;
gastrointestinal bleeding and other active bleeding (including suspected intracranial hemorrhage);
inflammatory bowel diseases (Crohn’s disease, ulcerative colitis) in the acute stage;
—severe liver failure (10-15 points on the Child-Pugh scale);
progressive kidney disease, confirmed tipercapemia;
chronic kidney disease: stage 3 (glomerular filtration rate (GFR) 45-59 ml/min/1.73 m2), 36 (GFR 30-44 ml/min/1.73 m2) and 4 (GFR < 30 ml/min/1.73 m2);
period after coronary artery bypass surgery;
—severe heart failure (III-IV class according to the NYHA classification);
hemorrhagic diathesis and other blood clotting disorders;
age under 18 years (due to lack of data on effectiveness and safety); —pregnancy and breastfeeding period.
With caution
Peptic ulcer of the stomach and duodenum, ulcerative colitis, Crohn’s disease, history of liver disease, hepatic porphyria, chronic kidney disease, stage 2 (GFR 60-89 ml/min/1.73 m2), chronic heart failure, arterial hypertension, significant decrease in circulating blood volume (including after surgery), elderly patients over 65 years of age (in including those receiving diuretics, weakened patients and those with low body weight), bronchial asthma, simultaneous use of glucocorticosteroids (including prednisone), anticoagulants (including warfarin), antiplatelet agents (including acetylsalicylic acid, cpopidotrel), selective serotonin reuptake inhibitors (including citalopram, fluoxetine, paroxetine, sertraline), coronary heart disease, cerebrovascular diseases, dyslipidemia/hyperlipidemia, diabetes mellitus, peripheral arterial disease, smoking, Helicobacter pylori infection, systemic lupus erythematosus (SLE) and other systemic connective tissue diseases, long-term use of non-geroid anti-inflammatory drugs, tuberculosis, severe osteoporosis, alcoholism, severe somatic diseases.
Side Effects
Side Effects
Possible side effects are listed in accordance with the World Health Organization classification in descending order of frequency: very common (21/10), common (a 1/100, <1/10), uncommon (a 1/1000, <1/100), rare (a 1/10000, <1/1000), very rare (<1/10000), including isolated reports.
Blood and lymphatic system disorders: very rarely – neutropenia, thrombocytopenia.
Immune system disorders: rarely – laryngeal edema; very rarely – anaphylactic reactions, including anaphylactic shock.
Nervous system disorders: uncommon – headache, dizziness, drowsiness; rarely – paresthesia, syncope (transient short-term fainting).
Mental disorders: infrequently – insomnia, anxiety. Violations of the organ of the lungs and labyrinthine disorders: infrequently – vertigo; very rarely – tinnitus.
Visual disorders: very rarely – blurred vision.
Disorders of the cardiovascular system: infrequently – palpitations, feeling of heat, hyperemia of the skin; rarely – increased blood pressure; very rarely – tachycardia, decreased blood pressure. Respiratory system disorders: rarely – bradypnea; very rarely – bronchospasm, shortness of breath.
Gastrointestinal tract disorders: often—nausea, vomiting, abdominal pain, dyspepsia, diarrhea; uncommon—gastritis, constipation, dry mouth, flatulence; rarely – erosive and ulcerative lesions of the gastrointestinal tract (GIT), bleeding from an ulcer or its perforation; very rarely – damage to the pancreas. Disorders of the liver and biliary tract: rarely – hepatitis, increased activity of liver enzymes, including aspartate aminotransferase and alanine aminotransferase (AST and APT); very rarely – liver damage.
Disorders of the kidneys and urinary tract: rarely – polyuria, acute renal failure; very rarely – nephritis or nephrotic syndrome. Reproductive system disorders: rarely – in women – menstrual irregularities, in men – transient dysfunction of the prostate gland with long-term use.
Disorders of the musculoskeletal system: rarely – back pain. Disorders of the skin and subcutaneous tissues: infrequently – skin rash; rarely – urticaria, acne, increased sweating; very rarely – severe skin reactions (Stevens-Johnson syndrome, toxic epidermal necrolysis (Lyell’s syndrome)), angioedema of the face, allergic dermatitis, photosensitivity, itching.
Metabolic disorders: rarely – anorexia.
General disorders: infrequently – increased fatigue, asthenia, chills, general malaise; very rarely – peripheral edema.
As with the use of other NSAIDs, the following side effects may develop: aseptic meningitis, which develops mainly in patients with systemic lupus erythematosus or other systemic connective tissue diseases, hematological disorders (thrombocytopenic purpura, aplastic and hemolytic anemia, in rare cases, agranulocytosis and bone marrow lchpoplasia). Overdose
Symptoms: nausea, anorexia, abdominal pain, headache, dizziness, disorientation, insomnia.
Treatment: symptomatic therapy, if necessary, gastric lavage, taking activated charcoal, hemodialysis is ineffective.
Interaction
Interaction
The following interactions are common to all NSAIDs.
Undesirable combinations
With other NSAIDs, including salicylates in high doses (more than 3 g/day): simultaneous use of several NSAIDs due to a synergistic effect increases the risk of gastrointestinal bleeding and ulcers.
With anticoagulants: dexketoprofen, like other NSAIDs, may enhance the effect of anticoagulants such as warfarin due to its high degree of protein binding
blood plasma, inhibition of platelet aggregation and damage to the mucous membrane of the gastrointestinal tract. If simultaneous use is necessary, careful monitoring of the patient’s condition and regular monitoring of laboratory parameters is necessary.
With heparin: with simultaneous use, the risk of bleeding increases (due to inhibition of platelet aggregation and damaging effects on the mucous membrane of the gastrointestinal tract). If simultaneous use is necessary, careful monitoring of the patient’s condition and regular monitoring of laboratory parameters is necessary.
With glucocorticosteroids: with simultaneous use, the risk of ulcerative lesions of the gastrointestinal tract and bleeding increases.
With lithium preparations: NSAIDs increase the concentration of lithium in the blood plasma up to toxic levels, and therefore this indicator must be monitored when used simultaneously with dexketoprofen, changing the dosage, and also after discontinuation of NSAIDs.
With methotrexate in high doses (15 mg/week or more): an increase in the hematological toxicity of methotrexate is possible due to a decrease in its renal clearance with simultaneous use of NSAIDs.
With hydantoins and sulfonamides: their toxic effect may be enhanced. Combinations requiring caution
With diuretics, angiotensin-converting enzyme (ACE) inhibitors, aminoglycoside antibiotics, angiotensin II receptor antagonists: simultaneous use with NSAIDs is associated with the risk of acute renal failure in dehydrated patients (decreased glomerular filtration rate due to reduced prostaglandin synthesis). When used concomitantly, NSAIDs may reduce the antihypertensive effect of some drugs. When using dexketoprofen and diuretics simultaneously, it is necessary to ensure that the patient has no signs of dehydration, and also monitor renal function at the beginning of simultaneous use.
With methotrexate in low doses (less than 15 mg/week): an increase in the hematological toxicity of methotrexate is possible due to a decrease in its renal clearance during simultaneous use with NSAIDs. A blood cell count is necessary when coadministration is initiated. If there is even mild renal impairment, as well as in elderly people, careful medical supervision is necessary.
With pvntoxifylline: there may be an increased risk of bleeding. Close clinical monitoring and regular checking of bleeding time (blood clotting time) are necessary.
With zidovudine: there is a risk of increased toxicity to red blood cells due to effects on reticulocytes, with the development of severe anemia one week after starting NSAID use. It is necessary to conduct a general blood test with counting the number of reticulocytes 1-2 weeks after starting NSAID therapy.
With oral hypoglycemic agents: NSAIDs may enhance the hypoglycemic effect of sulfonylureas due to the displacement of sulfonylurea from sites of binding to plasma proteins.
Combinations that need to be taken into account With β-blockers: when used simultaneously with NSAIDs, the antihypertensive effect of β-blockers may be reduced due to inhibition of prostaglandin synthesis.
With cyclosporine and tacrolimus: NSAIDs may increase nephrotoxicity, which is mediated by the action of renal prostaglandins. With simultaneous use, it is necessary to monitor renal function.
With thrombolytics: the risk of bleeding increases.
The risk of bleeding from the gastrointestinal tract increases when used simultaneously with serotonin reuptake inhibitors (citalopram, fluoxetine, sertraline) and anticoagulants.
With probenecid: an increase in the concentration of NSAIDs in the blood plasma is possible, which may be due to the inhibitory effect of probenecid on renal tubular secretion and/or conjugation with glucuronic acid; NSAID dose adjustment may be required.
With cardiac glycosides: simultaneous use with NSAIDs may lead to an increase in the concentration of cardiac glycosides in the blood plasma.
With mifepristone: due to the theoretical risk of changes in the effectiveness of mifepristone under the influence of prostaglandin synthesis inhibitors, NSAIDs should not be used earlier than 8-12 days after discontinuation of mifepristone.
With quinolones: data obtained from experimental studies in animals indicate a high risk of developing seizures when NSAIDs are used concomitantly with quinolones in high doses.
If it is necessary to use the drug Flamadex simultaneously? with the above medications, you should consult your doctor.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 ° C.
Keep out of the reach of children.
Shelf life
Shelf life
2 years.
Do not use after the expiration date stated on the package.
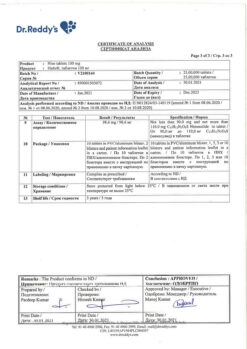
Manufacturer
Manufacturer
Rapharma JSC, Russia
Additional information
| Shelf life | 2 years. Do not use after the expiration date stated on the package. |
|---|---|
| Conditions of storage | Store in a dry place protected from light at a temperature not exceeding 25 °С. Keep out of reach of children. |
| Manufacturer | Rapharma AO, Russia |
| Medication form | pills |
| Brand | Rapharma AO |
Other forms…
Related products
Buy Flamadex, 25 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.