No products in the cart.
Erythromycin, lyophilizate 100 mg 50 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Bacterial infections caused by susceptible pathogens: diphtheria (including Bacterial infections caused by susceptible pathogens: diphtheria (including bacteriocarriage) whooping cough trachoma brucellosis legionnaire’s disease erythrax listeriosis scarlet fever amebic dysentery gonorrhea; urogenital infections in pregnant women caused by Chlamydia trachomatis; primary syphilis (in penicillin-allergic patients) ENT-organ infections (tonsillitis otitis sinusitis); infections of biliary tract (cholecystitis); infections of upper and lower respiratory tract (tracheitis bronchitis pneumonia); infections of skin and soft tissue (infected wounds decubitus burns II-III degree trophic ulcers).
The prevention of infectious complications during medical and diagnostic procedures (including preoperative preparation of the intestine, dental interventions, endoscopy in patients with cardiac defects).
Gastroparesis (including gastroparesis after vagotomy surgery diabetic gastroparesis and gastroparesis associated with progressive systemic sclerosis).
Active ingredient
Active ingredient
Composition
Composition
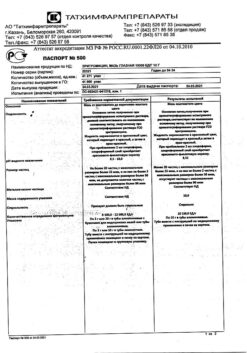
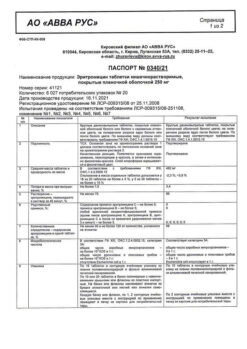
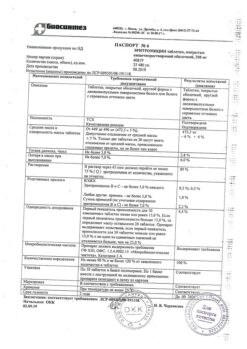
Composition per 1 vial:
Active substance:
Eritromycin phosphate – 113.35 mg; 226.70 mg (in terms of erythromycin – 100 mg; 200 mg).
How to take, the dosage
How to take, the dosage
Intravenously slowly (over 3-5 minutes) or by drip. Intravenous drip administration of the drug is preferred and safer.
The single dose of the drug for adults is 0.2 g, daily 0.6 g. In severe course of infection daily dose may be increased up to 1 g. Then the drug is administered 4 times a day (every 6 hours). For children aged 4 months to 18 years, depending on age, body weight and severity of infection, the dose is 30-50 mg/kg/day (for 2-4 injections); for children in the first 3 months of life, it is 20-40 mg/kg/day. In case of severe infections the dose may be doubled.
For intravenous injection the drug is dissolved in water for injection or 0.9% sodium chloride solution at the rate of 5 mg per 1 ml of the solvent.
For intravenous drip administration the drug is dissolved in 0.9% sodium chloride solution or 5% dextrose solution to a concentration of 1 mg/ml and administered at a rate of 60-80 drops/min. It is administered intravenously for 5-6 days (until a clear therapeutic effect) with subsequent transition to oral administration.
In case of good tolerance and absence of phlebitis and periphlebitis the course of intravenous administration can be prolonged up to 2 weeks (not more).
In case of renal insufficiency, there is no need to adjust the dose of the drug.
Interaction
Interaction
Reduces the bactericidal effect (antagonism) of beta-lactam antibiotics (penicillins, cephalosporins, carbapenems), lincomycin, clindamycin, chloramphenicol, streptomycin, tetracyclines, colistin.
Enhances theophylline concentration in blood: Theophylline dose may need to be reduced. At the same time, erythromycin concentrations may decrease, which may lead to subtherapeutic concentrations of erythromycin and a reduction in its effect.
It enhances nephrotoxicity of cyclosporine (especially in patients with concomitant renal failure).
Limits the clearance of triazolam and midazolam, and therefore may increase the pharmacological effects of benzodiazepines.
Delays elimination (enhances the effect) of methylprednisolone, felodipine and coumarin-type anticoagulants.
The risk of rhabdomyolysis increases when combined with lovastatin and other HMG-CoA reductase inhibitors.
Increases the bioavailability of digoxin.
Decreases the effectiveness of hormonal contraception.
Drugs (drugs) that block tubular secretion prolong the T1/2 of erythromycin.
Because erythromycin is an isoenzyme inhibitor and CYP3A substrate, when concomitant use with drugs metabolized in the liver (acenocoumarol, astemizole, cilostazol, cyclosporine, dihydroergotamine, ergotamine, omeprazole, quinidine, rifabutin, tacrolimus, terfenadine, vinblastine, carbamazepine, valproic acid, hexobarbital, phenytoin, alfentanil, disopyramide, lovastatin, bromocriptine, antifungal drugs such as fluconazole, ketoconazole and itraconazole), plasma concentrations of these drugs may be increased.
Drugs that are inducers of CYP3A4 isoenzymes (such as rifampicin, phenytoin, carbamazepine, phenobarbital, St. John’s wort) may induce erythromycin metabolism that may lead to subtherapeutic concentration of erythromycin and reduction of its effect. The interaction persists for 2 weeks after discontinuation of treatment with CYP3A4 inducers.
Erythromycin alters the metabolism of misolastin.
When combined with pimozide, arrhythmia (ventricular fibrillation and flutter), pirouette-type ventricular tachycardia, cardiac arrest, up to and including death may occur.
Protease inhibitors inhibit erythromycin metabolism; monitoring of plasma erythromycin concentrations is necessary.
Simultaneous use with terfenadine or astemizole may cause arrhythmias (ventricular fibrillation and flutter, ventricular tachycardia, up to death), with dihydroergotamine or dihydrogenated ergot alkaloids – vasoconstriction to spasm, dysesthesia.
The simultaneous use of erythromycin with sildenafil may result in a moderate increase in the maximum concentration of sildenafil in the blood.
Elevated cisapride levels may cause prolongation of the QTc interval, and arrhythmias (ventricular fibrillation and torsade de pointes) and pirouette-type ventricular tachycardia may develop.
When co-administered with verapamil and other slow calcium channel blockers, hypotension, bradyarrhythmia and lactoacidosis have been observed.
Cimetidine inhibits erythromycin metabolism, which may lead to increased plasma concentrations of erythromycin.
Erythromycin decreases the clearance of zopiclone and thus may increase the pharmacodynamic effects of this drug.
The concomitant use of erythromycin increases the toxicity of colchicine.
Special Instructions
Special Instructions
It is a reserve antibiotic in case of penicillin allergy.
Long-term therapy requires monitoring of laboratory parameters of liver function.
The symptoms of cholestatic jaundice may develop within a few days after the start of therapy, but the risk of development increases after 7-14 days of continuous therapy. The likelihood of developing ototoxic effects is higher in patients with renal and or hepatic impairment, as well as in elderly patients.
May interfere with determination of urinary catecholamines and blood “hepatic” transaminase activity (colorimetric determination with diphenylhydrazine).
In co-administration with statins, rhabdomyolysis and pseudomembranous colitis are possible.
Impact on driving, operating machinery
When treating with Erythromycin, caution should be exercised when driving vehicles, operating machinery, and engaging in other hazardous activities requiring special attention and quick reactions.
Contraindications
Contraindications
Hypersensitivity to erythromycin, significant hearing loss, concomitant administration of terfenadine or astemizole, breastfeeding period. Simultaneous use of pimozide, cisapride, ergotamine and dihydroergotamine.
With caution
Arrhythmias (history), prolonged QT interval, jaundice (history), hepatic and/or renal failure, myasthenia gravis, concomitant use of hepatotoxic drugs.
Side effects
Side effects
Immune system disorders: urticaria, other forms of skin rash (erythema multiforme, Stevens-Johnson syndrome, Lyell syndrome), angioedema, eosinophilia, anaphylactic shock.
Digestive system disorders: Anorexia, nausea, vomiting, gastralgia, abdominal pain, tenesmus, diarrhea, dysbacteriosis, candidiasis of the oral mucosa, pseudomembranous colitis, liver function disorders, hepatocellular hepatitis, hepatomegaly, cholestatic jaundice, increased activity of “liver” transaminases, pancreatitis.
Hearing organ: ototoxicity – decreased hearing and/or tinnitus (when used in high doses – more than 4 g/day, usually reversible).
Cardiovascular system disorders: decreased blood pressure, tachycardia, prolonged QT interval on electrocardiogram, atrial fibrillation and/or flutter (in patients with prolonged QT interval on electrocardiogram); ventricular arrhythmias, including ventricular tachycardia and torsade des pointes (prolonged QT interval syndrome).
Nervous system disorders: convulsions, hallucinations, vertigo, confusion, development of myasthenic syndrome or exacerbation of myasthenia gravis.
Urinary system disorders: interstitial nephritis.
General disorders and disorders at the site of injection: chest pain, fever, malaise, phlebitis at the site of intravenous injection.
If any of the side effects listed in the instructions worsen, or if you notice any other side effects not listed in the instructions, tell your doctor.
Overdose
Overdose
Symptoms: nausea diarrhea discomfort in the stomach area; dizziness (especially in patients with hepatic or renal failure); impaired liver function up to acute liver failure rarely – hearing loss.
The treatment: close monitoring of the state of respiratory system (if necessary – carrying out artificial lung ventilation) acid-base state and electrolyte metabolism ECG. Symptomatic therapy should be administered. Hemodialysis peritoneal dialysis and forced diuresis are ineffective.
Pregnancy use
Pregnancy use
Prenatal use of the drug is possible only in cases when the estimated benefit to the mother exceeds the potential risk to the fetus.
If it is necessary to use the drug during lactation, discontinuation of breastfeeding should be considered.
Similarities
Similarities
Additional information
| Weight | 0.832 kg |
|---|---|
| Shelf life | 4 years. Do not use after the expiration date printed on the package. |
| Conditions of storage | In a dry place protected from light at a temperature not exceeding 25 ° C. Store out of the reach of children. |
| Manufacturer | Sintez OAO, Russia |
| Medication form | lyophilizate |
| Brand | Sintez OAO |
Other forms…
Related products
Buy Erythromycin, lyophilizate 100 mg 50 pcs with delivery to USA, UK, Europe and over 120 other countries.