No products in the cart.
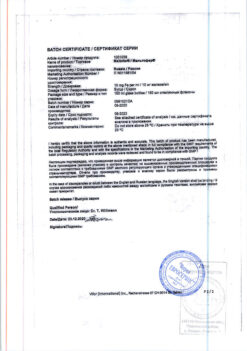
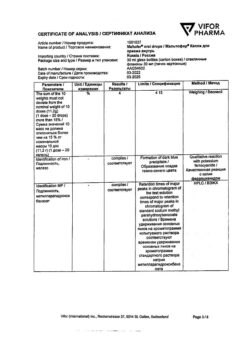
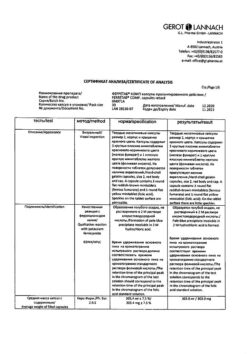
Eralphon,. 10000 me 1 ml syringe
€113.71 €94.76
Description
Epoetin alpha is a glycoprotein that specifically stimulates erythropoiesis, activates mitosis and erythrocyte maturation from erythrocyte progenitor cells.
The recombinant epoetin alpha is synthesized in mammalian cells which contain the gene encoding human erythropoietin. By its composition, biological and immunological properties epoetin alpha is identical to natural human erythropoietin. Introduction of epoetin alfa leads to increase of hemoglobin and hematocrit levels, improvement of blood supply to tissues and heart work.
The most pronounced effect of epoetin alfa is observed in anemia caused by chronic renal failure.
In very rare cases with long-term use of erythropoietin for therapy of anemic conditions the formation of neutralizing antibodies to erythropoietin with the development of partial red cell aplasia or without it may be observed.
Indications
Indications
anemia in patients with chronic renal failure, incl. those on hemodialysis;
prevention and treatment of anemia in patients with solid tumors, whose anemia was a consequence of antitumor therapy;
prevention and treatment of anemia in patients infected with the human immunodeficiency virus (HIV) caused by the use of zidovudine, with endogenous erythropoietin levels less than 500 IU/ml;
prevention and treatment of anemia in patients with multiple myeloma, low-grade non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis;
treatment and prevention of anemia in premature babies born with low body weight (up to 1.5 kg);
as part of a predeposit program before major surgery in patients with a hematocrit level of 33–39%, to facilitate the collection of autologous blood and reduce the risk associated with the use of allogeneic blood transfusions if the expected need for transfusion exceeds the amount that can be obtained by autologous collection without the use of epoetin alfa;
before major surgery with an expected blood loss of 900–1800 ml in adult patients without anemia or with mild to moderate anemia (hemoglobin level 100–130 g/l), to reduce the need for allogeneic blood transfusions and facilitate restoration of erythropoiesis.
Pharmacological effect
Pharmacological effect
Epoetin alfa is a glycoprotein that specifically stimulates erythropoiesis, activates mitosis and maturation of erythrocytes from erythrocyte precursor cells.
Recombinant epoetin alfa is synthesized in mammalian cells into which the gene encoding human erythropoietin is integrated. In its composition, biological and immunological properties, epoetin alfa is identical to natural human erythropoietin. The administration of epoetin alfa leads to an increase in hemoglobin and hematocrit levels, improving blood supply to tissues and heart function.
The most pronounced effect of the use of epoetin alfa is observed in anemia caused by chronic renal failure.
In very rare cases, with long-term use of erythropoietin for the treatment of anemic conditions, the formation of neutralizing antibodies to erythropoietin may be observed with or without the development of partial red cell aplasia.
Special instructions
Special instructions
During treatment, it is necessary to monitor blood pressure weekly and perform a complete blood count (including platelets, hematocrit, ferritin). In the pre- and postoperative period, hemoglobin levels should be monitored more often if the initial level was
In patients with controlled arterial hypertension or a history of thrombotic complications, an increase in the dose of antihypertensive drugs and/or anticoagulants may be required, respectively. When prescribed to patients with liver failure, a slowdown in the metabolism of epoetin alfa and a pronounced increase in erythropoiesis are possible. The safety of the drug in this category of patients has not been established. Although the drug stimulates erythropoiesis, the possibility of epoetin alfa affecting the growth of certain types of tumors, including bone marrow.
The possibility that a preoperative increase in hemoglobin levels may predispose to the development of thrombotic complications should be considered. Before undergoing elective surgery, patients should receive adequate prophylactic antiplatelet therapy. In the pre- and postoperative period, the drug is not recommended for use in patients with an initial hemoglobin level of more than 150 g/l.
In adult patients with chronic renal failure, clinically significant coronary artery disease or chronic heart failure, the hemoglobin level should not exceed 100–120 g/l.
Before starting treatment, possible causes of an inadequate reaction to the drug should be excluded (deficiency of iron, folic acid, cyanocobalamin, severe poisoning with aluminum salts, concomitant infections, inflammatory processes and injuries, hidden bleeding, hemolysis, bone marrow fibrosis of various etiologies) and, if necessary, adjust the treatment.
Before starting treatment, iron reserves in the body should be assessed. In most patients with chronic renal failure, cancer and HIV-infected patients, plasma ferritin concentration decreases simultaneously with an increase in hematocrit level. Ferritin concentrations must be determined throughout the course of treatment. If it is less than 100 ng/ml, oral iron replacement therapy is recommended at a rate of 200–300 mg/day (100–200 mg/day for children). In premature infants, oral iron therapy at a dose of 2 mg/day should be prescribed as early as possible. Patients donating autologous blood and in the pre- or postoperative period should also receive adequate amounts of iron orally at a dose of 200 mg/day.
In patients with chronic renal failure, correction of anemia may result in improved appetite and increased absorption of potassium and protein. Periodic adjustments of dialysis parameters may be required to maintain blood urea, creatinine, and potassium concentrations within normal limits.
In patients with chronic renal failure, it is necessary to monitor the level of electrolytes in the blood serum.
According to available data, the use of epoetin alfa in predialysis patients does not accelerate the progression of chronic renal failure. Due to increased hematocrit, it is often necessary to increase the dose of heparin during hemodialysis. With inadequate heparinization, blockage of the dialysis system and thrombosis of the vascular access are possible, especially in patients with a tendency to hypotension or complications of an arteriovenous fistula (including stenosis, aneurysm). In such patients, thrombosis prophylaxis is recommended.
When used in women of reproductive age with anemia due to chronic renal failure, menstruation may resume. The patient should be warned about the possibility of pregnancy and the need to use reliable methods of contraception before starting therapy. Experimental studies on rats and rabbits did not reveal a teratogenic effect when administered intravenously in doses up to 500 IU/kg/day; at higher doses, a weak, statistically insignificant decrease in fertility was noted.
Considering the possible more pronounced effect of the drug, its dose should not exceed the dose of recombinant erythropoietin used in the previous course of treatment. During the first 2 weeks, the dose is not changed, the dose/response ratio is assessed. After this, the dose can be reduced or increased (see “Dosage and Administration”).
Impact on the ability to drive vehicles and operate machinery. During the treatment period, until the optimal maintenance dose is established, patients with chronic renal failure must be careful when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions (increased risk of increased blood pressure at the beginning of therapy).
Active ingredient
Active ingredient
Epoetin alfa
Composition
Composition
1 syringe (1 ml) contains:
Contraindications
Contraindications
hypersensitivity to the drug Eralfon or its components;
partial red cell aplasia after previous therapy with any erythropoietin;
uncontrolled arterial hypertension;
inability to carry out adequate anticoagulant therapy;
severe occlusive diseases of the coronary, carotid, cerebral and peripheral arteries and their consequences, including acute and recent myocardial infarction and acute cerebrovascular accident (as part of a pre-deposit blood collection program before surgery).
With caution: malignant neoplasms; epileptic syndrome, incl. in the anamnesis; thrombocytosis, thrombosis (history); sickle cell anemia; iron, B12 or folate deficiency conditions; porphyria; chronic liver failure.
Side Effects
Side Effects
At the beginning of treatment, flu-like symptoms may be observed: dizziness, drowsiness, fever, headache, myalgia, arthralgia.
From the cardiovascular system: dose-dependent increase in blood pressure, worsening of arterial hypertension (most often in patients with chronic renal failure), in some cases – hypertensive crisis, a sharp increase in blood pressure with symptoms of encephalopathy (headache, confusion) and generalized tonic-clonic convulsions.
From the hematopoietic organs: thrombocytosis, in some cases – thrombosis of the shunt or arteriovenous fistula (including patients on hemodialysis with a tendency to arterial hypotension or with an aneurysm, stenosis), aplasia of the erythrocyte lineage.
Allergic reactions: skin rash (mild or moderate), eczema, urticaria, itching, angioedema.
Local reactions: hyperemia, burning, mild or moderate pain at the injection site (more often occur with subcutaneous administration).
From the laboratory parameters: decrease in serum ferritin concentration, with uremia – hyperkalemia, hyperphosphatemia.
Other: complications associated with respiratory failure or decreased blood pressure, immune reactions (induction of antibody formation), exacerbation of porphyria.
Interaction
Interaction
Reduces the concentration of cyclosporine due to an increase in the degree of its binding to red blood cells (it may be necessary to adjust the dose of cyclosporine).
Pharmaceutically incompatible with solutions of other drugs.
Overdose
Overdose
Symptoms: increased side effects.
Storage conditions
Storage conditions
At 2–8 °C
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
PharmFirma Sotex, Russia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | At 2-8 °C |
| Manufacturer | PharmFirm Sotex, Russia |
| Medication form | solution |
| Brand | PharmFirm Sotex |
Other forms…
Related products
Buy Eralphon,. 10000 me 1 ml syringe with delivery to USA, UK, Europe and over 120 other countries.