No products in the cart.
Equator, tablets 5 mg+10 mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Equator is a combined antihypertensive drug containing lisinopril and amlodipine.
Lisinopril is an ACE inhibitor, reduces blood levels of angiotensin II and aldosterone while increasing levels of bradykinin, a vasodilatory mediator. Effects on tissue renin-angiotensin systems. It decreases RPS and BP, pre- and post-load, pulmonary capillary pressure, has no effect on HR, while it may increase cardiac output and increase blood flow in the kidneys. Dilates arteries more than veins. Improves blood supply to ischemic myocardium.
Long-term use promotes reduction of myocardial hypertrophy and resistive artery walls. Increases myocardial tolerance to exercise in patients with chronic heart failure. Plays a role in restoring endothelial function damaged due to hyperglycemia.
Lengthens life expectancy in chronic heart failure. Slows the progression of left ventricular dysfunction after myocardial infarction not complicated by heart failure.
Hypotensive effect is observed 1 hour after oral administration of the drug, reaching a maximum after 6 hours. The duration of action depends on the dose and is 24 hours. With long-term treatment the efficacy does not decrease. There is no withdrawal syndrome with a sharp increase in BP when the treatment is stopped abruptly.
Despite the primary effect manifested in the effect on the RAAS, it is also effective in arterial hypertension with low levels of renin.
Lisinopril decreases albuminuria not only due to BP decrease, but also due to the changes in hemodynamics of glomerular apparatus and its tissue structure. It does not affect blood sugar levels in diabetic patients and does not increase the incidence of hypoglycemia.
Amlodipine is a III generation slow calcium channel blocker, has antianginal and hypotensive effect. It prevents calcium influx into myocardial cells and, to a greater extent, into smooth muscle cells of the vascular wall. It reduces the tone of arteriolar smooth muscle, OPPS and, therefore, BP.
It has an antianginal effect by dilating the arterioles and arteries and reducing the afterload. It reduces the need for oxygen and myocardial energy expenditure, as it does not cause reflex tachycardia. Probably due to the expansion of coronary arteries and arterioles it increases the supply of oxygen to the intact (especially in vasospastic angina) and ischemic areas of the myocardium. In angina improves exercise tolerance, prevents the development of an attack of angina and the formation of ischemic ST interval, reducing the frequency of angina attacks and the need for nitroglycerin use.
It does not affect myocardial conduction and contractility.
It has a long-lasting, dose-dependent hypotensive effect. Does not reduce the left ventricular ejection fraction. Reduces left ventricular hypertrophy. It has antiatherosclerotic and cardioprotective effect in CHD. Its usage along with digoxin, diuretics and ACE inhibitors does not increase the risk of death in patients with chronic heart failure (functional class III-IV according to NYHA classification).
Slow absorption, wide distribution in the body and slow excretion provides prolonged action, allowing to take the drug once/ For more than 24 hours provides significant clinically significant reduction of BP in sitting and lying position. The action develops gradually, 2-4 hours after administration and is not accompanied by arterial hypotension.
Inhibits platelet aggregation, increases glomerular filtration, has a weak natriuretic effect, in diabetic nephropathy it does not increase microalbuminuria.
It does not have adverse effects on metabolic processes, does not change the level of plasma lipids. It can be prescribed to patients with concomitant bronchial asthma, diabetes and gout.
Combining lisinopril with amlodipine in one drug prevents possible adverse effects caused by counterregulation of any of the active substances. For example, a slow calcium channel blocker, by directly dilating the arterioles, can lead to sodium and fluid retention in the body and, therefore, can activate the RAAS. The ACE inhibitor blocks this process and normalizes responses to salt load.
Indications
Indications
Essential arterial hypertension (if combined therapy is necessary).
Active ingredient
Active ingredient
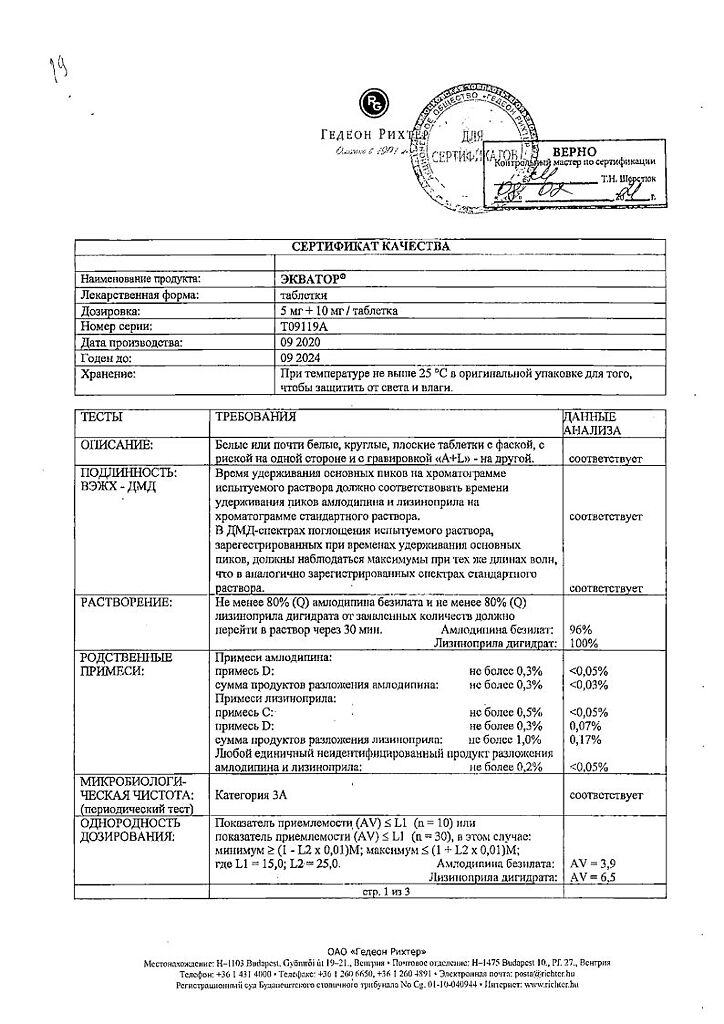
Composition
Composition
1 tablet contains:
lisinopril dihydrate 10.88 mg, which corresponds to the content of lisinopril 10 mg,
amlodipine besylate 6.94 mg, which corresponds to the content of amlodipine 5 mg.
Auxiliary substances:
Magnesium stearate 1 mg,
Sodium carboxymethyl starch (type A) 4 mg,
Microcrystalline cellulose 177.18 mg.
How to take, the dosage
How to take, the dosage
It is recommended for use in cases where taking drugs containing the active ingredients of Equator separately in the same doses does not provide the necessary control of BP. The drug is taken orally, regardless of meals.
For patients who are not receiving antihypertensives, the daily dose is 1 tablet.
In case of previous therapy with diuretics, the diuretic should be withdrawn 2-3 days before starting Equator. If diuretic withdrawal is not possible, the starting dose of Equator is 1/2 tablet/ After taking the drug, the patient should be medically monitored for several hours because of the possible development of symptomatic hypotension.
In cases of heart failure and severe arterial hypertension, the maintenance dose is 1 tablet.
In case of renal insufficiency and CK of 30-70 ml/min, half of the usual starting dose is prescribed (because lisinopril is excreted by kidneys). Maintenance dose depends on individual patient’s reaction; during therapy it is necessary to monitor renal function, potassium and sodium levels in blood regularly.
In patients with liver disease amlodipine excretion may slow down, therefore the initial dose of Equator is 1/2 tablet per day.
Interaction
Interaction
Lisinopril
Lysinopril Potassium-saving diuretics (e.g., spironolactone, amiloride, and triamterene), potassium supplements, potassium-containing salt substitutes, and other medications that can increase serum potassium levels (e.g., heparin) can lead to hyperkalemia when combined with ACE inhibitors, especially in patients with renal insufficiency and other renal diseases in the history.
The serum potassium concentration should be monitored when prescribing a potassium-affecting drug concomitantly with lisinopril. Therefore, concomitant administration must be carefully justified and should be performed with extreme caution and regular monitoring of both serum potassium levels and renal function.
Kalium-saving diuretics may be taken together with Equator only under medical supervision. If a diuretic is prescribed to a patient receiving Equator, the hypotensive effect tends to increase. Therefore, extreme caution should be exercised when taking Equator® in combination with diuretics. Lisinopril mitigates potassium diuretic effect. concomitant use of other antihypertensive drugs may increase the hypotensive effect of the drug Equator.
Concomitant use with nitroglycerin, other nitrates or vasodilators may cause greater BP reduction.
Concomitant use with ACE inhibitors of tricyclic antidepressants/antipsychotics, general anesthetic agents, opioid analgesics: greater BP reduction may be possible.
Ethanol increases the hypotensive effect of the drug. Allopurinol, procainamide, cytostatics or immunosuppressants (systemic GCS) may increase the risk of leukopenia when combined with ACE inhibitors.
Aitacids and colestiramine decrease the bioavailability of ACE inhibitors concomitantly.
Sympathomimetics may decrease the hypotensive effect of ACE inhibitors; the desired effect should be carefully controlled. Concomitant use of ACE inhibitors and hypoglycemic drugs (insulin and hypoglycemic agents for oral administration) may increase the probability of decreased blood glucose concentration and the risk of hypoglycemia. This phenomenon is most often observed during the first week of combined treatment and in patients with renal insufficiency. With long-term use of NSAIDs, including acetylsalicylic acid in high doses, the effectiveness of ACE inhibitors may decrease.
Additive effect when taking NSAIDs and ACE inhibitors is manifested by increased serum potassium levels and may lead to worsening of renal function. These effects are usually reversible. Very rarely, acute renal failure may develop, especially in elderly patients and patients in a state of dehydration.
The excretion of lithium may be delayed during concomitant use with ACE inhibitors and therefore serum lithium concentration should be monitored during this period. Co-administration with lithium preparations may increase manifestation of their neurotoxicity (nausea, vomiting, diarrhea, ataxia, tremor, tinnitus).
In concomitant use of ACE inhibitors and gold drugs (sodium aurothiomalate) by IV has described a symptom complex including facial hyperemia, nausea, vomiting and arterial hypotension.
Amlodipine
Studies in elderly patients have shown that diltiazem inhibits the metabolism of amlodipine, probably through inhibition of the CYP3A4 isoenzyme (plasma concentrations are increased by almost 50% and amlodipine effects are increased).
The possibility cannot be excluded that stronger inhibitors of CYP3A4 isoenzyme (i.e. ketoconazole, itraconazole, ritonavir) can increase the plasma concentration of amlodipine to a greater extent than diltiazem. Simultaneous use should be used with caution.
Concomitant use with inducers of CYP3A4 isoenzyme – with antiepileptic drugs (e.g., carbamazepshum, phenobarbital, phenytoin, fosphenytoin, primidone), rifampicin, herbal drugs containing St. John’s wort – may decrease the plasma concentration of amlodipine. Clinical monitoring with possible correction of amlodipine dose during treatment with CYP3A4 isoenzyme inducers and after their withdrawal is indicated. Concomitant use should be performed with caution.
. As monotherapy, amlodipine has been well combined with thiazide and “loop” diuretics, general anesthetics, beta-adrenoblockers, ACE inhibitors, long-acting nitrates, sublingual nitroglycerin, Digoxin, warfarin, atorvastatin, sildenafil, antacids (aluminum hydroxide, magnesium hydroxide), simethicone, cimetidine, NSAIDs, antibiotics and oral hypoglycemic drugs.
Amlodipine has no significant effect on the pharmacokinetics of ethanol. Calcium preparations may reduce the effect of slow calcium channel blockers. Amlodipine does not cause significant changes in the pharmacokinetics of cyclosporine. The hypotensive effect of Equator may be reduced when concomitantly administered with estrogens, adrenostimulants. When concomitant use with the drug Equator® procainamide, quinidine and other drugs that prolong the QT interval may contribute to its significant prolongation.
Special Instructions
Special Instructions
Arterial hypotension: marked BP decrease with the development of clinical symptoms may be observed in patients with decreased BOD and/or sodium content due to diuretics, fluid loss or for other reasons, such as profuse sweating, prolonged vomiting and/or diarrhea. In case of arterial hypotension, the patient should be laid down and fluid loss replenished (intravenous infusion of 0.9% sodium chloride solution) if necessary. Preferably, recovery of fluid and/or sodium loss should be performed before starting Equator therapy. BP should be monitored after the initial dose.
Aortic and mitral stenosis: As with all vasodilators, Equator® should be administered with caution in patients with left ventricular outflow tract obstruction and mitral valve stenosis.
Renal dysfunction: in some patients with arterial hypertension without pronounced manifestations of renovascular disease an increase in serum creatinine and urea was observed, in most cases minimal or transient, more pronounced when concomitant use of ACE inhibitors and diuretic. This is most common in patients with a history of renal disease.
The angioedema of the face, extremities, lips, tongue, vocal folds and/or larynx have been reported in patients who have taken an ACE inhibitor, including lisinopril. In these cases, Equator should be stopped immediately and the patient should be closely monitored until the symptoms completely disappear. Swelling of the face, lips and extremities usually goes away on its own, however, antihistamines should be used to reduce the severity of symptoms. Angioedema with laryngeal edema may be fatal. If swelling of the tongue, pharynx or larynx is suspected of causing airway obstruction, emergency measures should be initiated promptly. Appropriate measures include: p/v injection of 0.3-0.5 mg or a slow intravenous injection of 0.1 mg of 0.1% epinephrine (adrenaline) solution, followed by intravenous GCS and antihistamine drugs, with monitoring of vital functions.
In patients taking ACE inhibitors, gastrointestinal wall edema was rare. These patients complained of abdominal pain (with or without nausea and vomiting); in some cases, no prior facial edema was observed and C-1 esterase activity was within normal limits. Angioneurotic edema was diagnosed by gastrointestinal computed tomography, or after ultrasound examination, or by surgery; symptoms disappeared after discontinuation of ACE inhibitor. Gastrointestinal wall edema should be included in the differential diagnostic series of abdominal pain in patients taking ACE inhibitors.
Anaphylactic reactions in patients on hemodialysis: cases of anaphylactic shock have been reported in patients who have had hemodialysis through a polyacrylonitrile membrane (e.g., AN 69) and who simultaneously received ACE inhibitors, so this combination should be avoided. Patients are advised to use either another type of dialysis membrane or a different class of hypotensive drug.
Anaphylactic reactions in patients during LDL apheresis: Rarely, patients receiving ACE inhibitors during LDL apheresis with dextran sulfate have developed life-threatening anaphylactic reactions. These reactions were prevented by discontinuing ACE inhibitors before each apheresis procedure.
Desensitization with wasp or bee venom: occasionally patients taking ACE inhibitors developed anaphylactic reactions when desensitized with venom of hymenoptera (e.g., wasps or bees). These life-threatening situations can be avoided by timely withdrawal of ACE inhibitors.
Hepatotoxicity: In rare cases, administration of ACE inhibitors has been accompanied by a syndrome that began with cholestatic jaundice or hepatitis and progressed to fulminant liver necrosis and has been fatal in several cases. The mechanism of this syndrome is unclear. Patients receiving Equator® who develop jaundice or have increased hepatic enzyme activity should discontinue Equator with follow-up monitoring.
Hepatic impairment: In patients with hepatic impairment, the T1/2 of amlodipine is prolonged. No dosing recommendations have been developed at this time, so Equator should be prescribed with caution, having previously evaluated the expected benefit and potential risk of treatment.
Hematological toxicity: neutropenia, agranulocytosis, thrombocytopenia and anemia have been reported in rare cases in patients receiving ACE inhibitors. Neutropenia is rare in patients with normal renal function and in the absence of other aggravating factors. Neutropenia and agranulocytosis are reversible and disappear after ACE inhibitor withdrawal.
Equator should be used with particular caution in patients with vascular collagenosis, during immunosuppressive therapy, during treatment with allopurinol or procainamide or when these aggravating factors are combined, especially if there is a prior renal impairment. Some of these patients have developed serious infectious diseases, which in several cases have not been corrected by antibiotic therapy. When prescribing Equator, it is advisable to periodically monitor the white blood cell count in these patients, and to caution them to report the first signs of infectious disease.
Cough: Coughing has often been reported during the use of ACE inhibitors. As a rule, cough is non-productive, persistent and ceased after discontinuation of the drug. In the differential diagnosis of cough, the cough caused by the use of ACE inhibitors must also be considered.
Surgery/general anesthesia: In patients undergoing major surgery or during general anesthesia with drugs leading to arterial hypotension, lisinopril may block angiotensin II formation after compensatory renin release. If arterial hypotension develops, probably as a result of the above mechanism, it may be corrected by increasing the RBC.
In elderly patients with impaired renal function, the dose of Equator should be adjusted.
Hyperkalemia: Increased serum potassium levels have been observed in some patients receiving ACE inhibitors. The risk group for development of hyperkalemia includes patients with renal insufficiency, diabetes mellitus, acute heart failure, dehydration, metabolic acidosis or concomitant use of potassium saving diuretics, potassium supplements, potassium containing salt substitutes or any other medical drugs leading to increase in serum potassium level (such as heparin). Serum potassium concentrations should be monitored if concomitant administration with the above drugs is necessary.
Patients of low body weight, short stature, and patients with significant hepatic impairment may require dose reduction.
Equator has no adverse effect on metabolism and plasma lipids and can be used in the treatment of patients with bronchial asthma, diabetes mellitus and gout.
Body weight control and monitoring by a dentist is required during treatment (to prevent soreness, bleeding and gum hyperplasia).
Impact on the ability to drive and operate machinery:
Equator may affect the ability to drive vehicles and operate complex machinery. Predominantly at the beginning of treatment transient arterial hypotension and dizziness may occur. Therefore, at the beginning of treatment, patients are advised to avoid driving vehicles, operating machinery and performing other work requiring concentration.
Contraindications
Contraindications
– history of angioedema, including caused by the use of other ACE inhibitors;
– hereditary or idiopathic angioedema;
– hemodynamically significant stenosis of the aorta or mitral valve;
– hypertrophic obstructive cardiomyopathy;
– severe arterial hypotension;
– cardiogenic shock;
– pregnancy;
– lactation period;
– children and adolescents under 18 years of age (due to absence of the data about efficiency and safety of the preparation in this age group);
– hypersensitivity to the components of the preparation or to other dihydropyridine derivatives.
With caution when using Equator in case of cerebrovascular diseases (including insufficiency of cerebral circulation), CHD, expressed bradycardia, tachycardia, chronic heart failure in decompensation stage, in mild or moderate arterial hypotension, CSSU, severe autoimmune diseases (including scleroderma).including scleroderma, SLE), inhibition of medullary hematopoiesis, diabetes, hyperkalemia, conditions after renal transplantation, renal failure, sodium-restricted diet, elderly patients, liver failure.
In acute myocardial infarction and within one month after it.
Side effects
Side effects
The adverse reactions that occur are usually mild and transient, and withdrawal of treatment is rarely required.
Side effects caused by the combined drug do not occur more often than in cases of taking each component separately. The most common are: headache (8%), dry cough (5%) and dizziness (3%). Possible: weakness, diarrhea, nausea, vomiting, orthostatic hypotension, skin itching, skin rash, swelling of the ankles of the feet, facial redness, chest pain, arthralgia (1-3%). The frequency of other side effects is less than 1%.
In case of hypersensitivity, angioedema of the face, extremities, lips, tongue, epiglottis and larynx may develop (0.1%). In such cases the treatment should be stopped immediately and the patient should be observed until all symptoms have disappeared.
Laboratory findings: hyperkalemia, increased creatinine, urea nitrogen, liver enzymes activity and blood bilirubin, especially in renal disease, diabetes mellitus and renovascular hypertension.
Hematopoietic organs: leukopenia, neutropenia, agranulocytosis (effect of ACE inhibitor), thrombocytopenia, erythrocytopenia, with long-term treatment a slight decrease of hemoglobin concentration and hematocrit may occur.
Other rare adverse reactions:
Cardiovascular system: arrhythmias, increased palpitations, tachycardia, probably as a result of excessive BP reduction in patients at high risk of myocardial infarction, cerebrovascular stroke.
Gastrointestinal tract: intestinal dysfunction, dry mouth, abdominal pain, pancreatitis, hepatocellular or cholestatic jaundice, hepatitis, gum hyperplasia, decreased appetite.
Skin disorders: urticaria, increased sweating, itching, alopecia.
Hypersensory system disorders: impaired renal function, frequent urination, oliguria, anuria, acute renal failure, uremia, proteinuria, impotence.
Immune system disorders: syndrome with the appearance of antinuclear antibodies, accelerated sedimentation rate and arthralgia; myalgia; erythema multiforme; fever.
CNS disorders: increased somnolence, muscle fasciculation of extremities and lips, asthenia, mood lability, confusion.
Overdose
Overdose
Symptoms: excessive peripheral vasodilation with a marked decrease in BP, acute vascular failure, impaired water-electrolyte balance, renal failure, hyperventilation, tachycardia, bradycardia, dizziness, anxiety, cough.
The treatment: symptomatic therapy, control of cardiac activity, BP, diuresis and water-electrolyte balance, and its correction, if necessary. In a pronounced BP decrease, the patient should be placed in the supine position, lower extremities should be elevated; if therapeutic response to IV fluid administration is unsatisfactory, administration of dopamine may be required.
Calcium gluconate may be administered intravenously to stop the effects of amlodipine. If necessary, intravenous administration of angiotensin II. Due to slow absorption of amlodipine in some cases the stomach is washed, activated charcoal is used. Lisinopril is excreted by hemodialysis; the strong degree of binding to blood proteins makes dialysis of amlodipine ineffective.
Pregnancy use
Pregnancy use
The drug is contraindicated in pregnancy. If pregnancy is detected, treatment should be discontinued as soon as possible.
Administration of lisinopril in the second and third trimesters of pregnancy may cause damage and death of the fetus due to the effect on the kidneys
(arterial hypotension, renal failure, hyperkalemia). Reduced amniotic fluid can lead to skull and facial deformities, impaired limb development, pulmonary hypoplasia and fetal death. There are no data on such and other effects earlier in pregnancy.
The drug is contraindicated during lactation due to excretion of amlodipine with breast milk. There are no data indicating penetration of lisinopril into breast milk.
Similarities
Similarities
Additional information
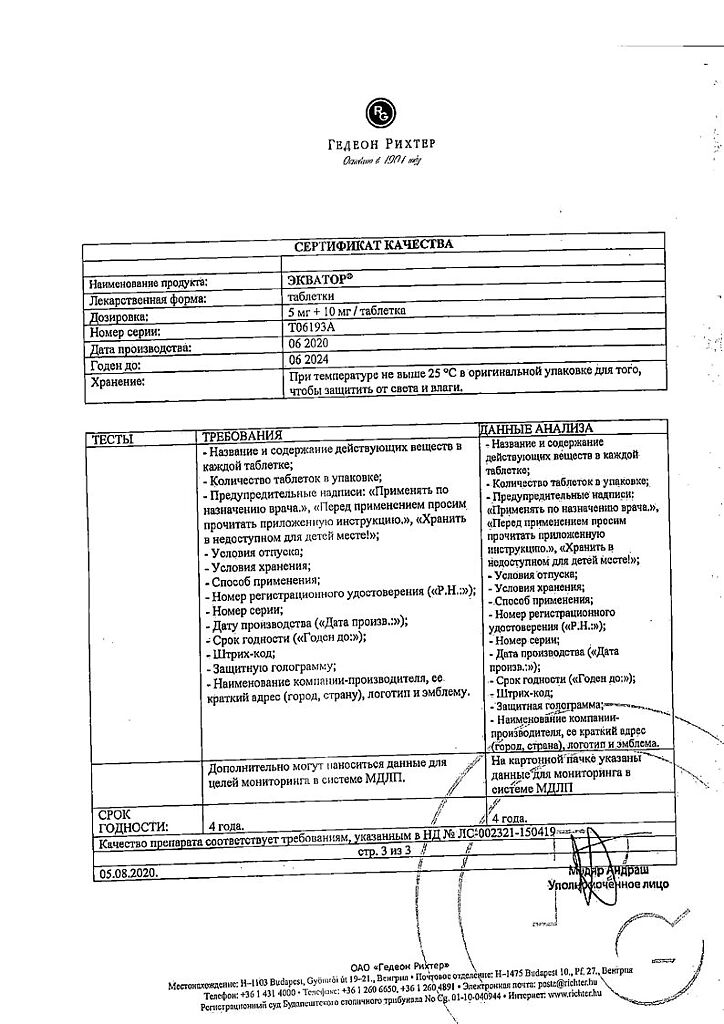
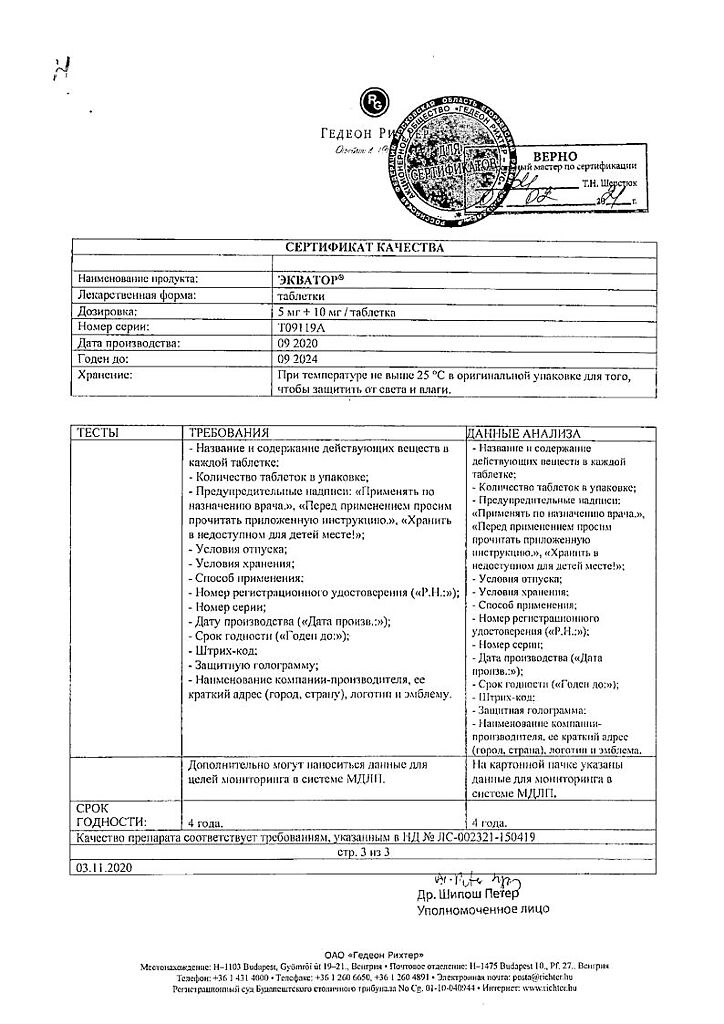
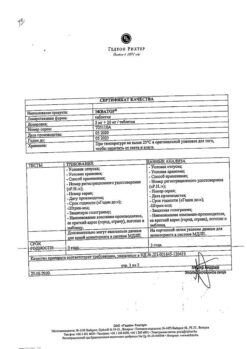
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | Gedeon Richter, Hungary |
| Medication form | pills |
| Brand | Gedeon Richter |
Other forms…
Related products
Buy Equator, tablets 5 mg+10 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.