No products in the cart.
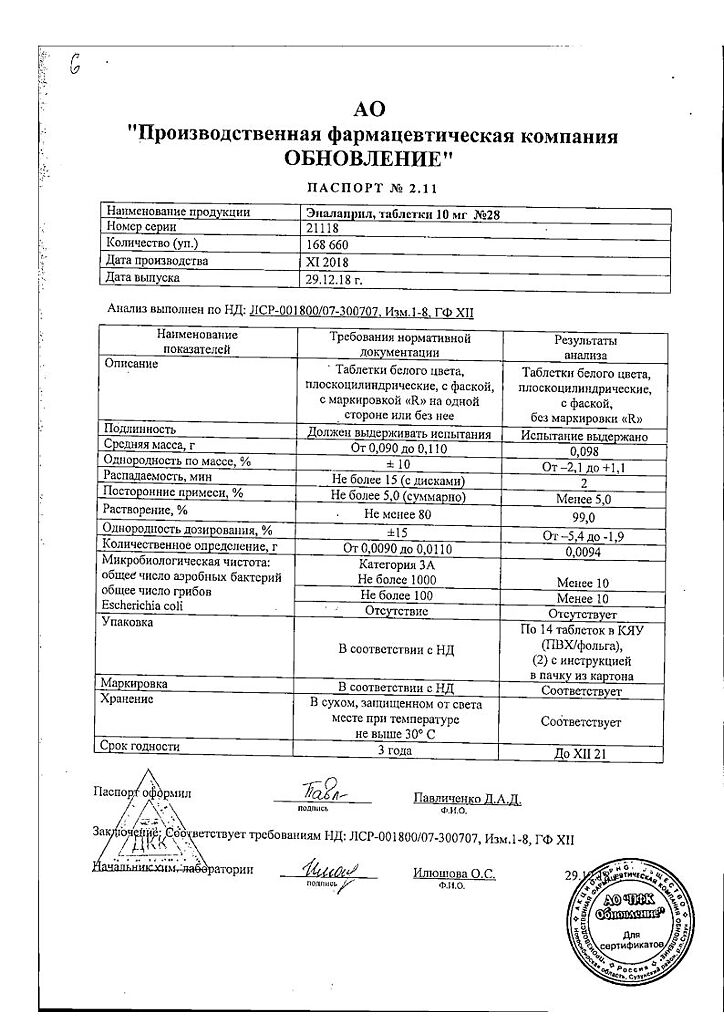
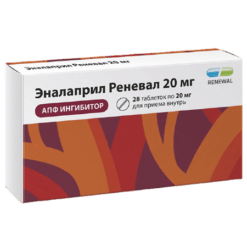
Enalapril Reneval, tablets 10 mg 28 pcs
€3.92 €3.56
Description
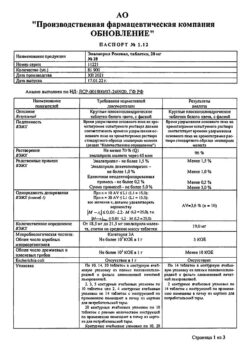
Pharmacotherapeutic group: angiotensin-converting enzyme (ACE) inhibitor. ATX code: C09AA02
Enalapril refers to drugs affecting the renin-angiotensin-aldosterone system (RAAS) – ACE inhibitors. Enalapril is used for treatment of essential hypertension (primary arterial hypertension (PH) of any severity and renovascular hypertension both in monotherapy and in combination with other hypotensive agents, in particular diuretics. Enalapril is also used to treat or prevent the development of heart failure (CHF).
Pharmacodynamics
Enalapril is a derivative of two amino acids, L-alanine and L-proline. After oral administration, enalapril is rapidly absorbed and hydrolyzed into enalaprilate, which is a highly specific and long-acting ACE inhibitor containing no sulfhydryl group.
The ACE (peptidyl dipeptidase A) catalyzes the conversion of angiotensin I into the pressor peptide angiotensin II. After absorption, enalapril is hydrolyzed to enalaprilate, which inhibits ACE. ACE inhibition leads to a decrease in plasma concentration of angiotensin II, which entails an increase in plasma renin activity (due to the elimination of negative feedback in response to renin release) and a decrease in aldosterone secretion.
The ACE is identical to the enzyme kininase II, so enalapril can also block the degradation of bradykinin, a peptide with a marked vasodilatory effect. The significance of this effect in the therapeutic effect of enalapril needs to be clarified.
While the primary mechanism by which enalapril lowers blood pressure (BP) is considered to be inhibition of the RAAS activity, which plays an important role in BP regulation, enalapril shows antihypertensive effect even in patients with AH and with decreased plasma renin activity.
The use of enalapril in patients with AH leads to a decrease in BP in both standing and lying position without a significant increase in heart rate (HR).
Symptomatic postural hypotension develops infrequently. In some patients, it may take several weeks of therapy to achieve optimal BP reduction. Interruption of therapy with enalapril does not cause a sharp rise in BP.
Effective inhibition of ACE activity usually develops 2-4 hours after a single oral dose of enalapril. Antihypertensive effect develops within 1 hour, the maximum BP reduction is observed 4-6 hours after taking the drug. The duration of action depends on the dose. However, when using the recommended doses, the antihypertensive effect and hemodynamic effects are maintained for 24 hours.
Enalapril hypotensive therapy leads to significant regression of left ventricular hypertrophy and preservation of systolic function.
In clinical studies of hemodynamics in patients with essential hypertension, a decrease in BP was accompanied by a decrease in total peripheral vascular resistance, an increase in cardiac output, and no or little change in HR. An increase in renal blood flow was observed after enalapril administration.
There was no change in glomerular filtration rate (GFR) and no evidence of sodium or fluid retention. However, in patients with initially decreased glomerular filtration its rate usually increased.
Long-term use of enalapril in patients with essential hypertension and renal insufficiency may result in improvement of renal function as indicated by increased GFR.
In short clinical trials in patients with renal insufficiency and with or without diabetes mellitus, a decrease in albuminuria, renal IgG excretion, and total protein in the urine after enalapril administration was observed.
When enalapril and thiazide diuretics are used concomitantly, a more pronounced antihypertensive effect is observed. Enalapril reduces or prevents the development of hypokalemia caused by taking thiazides.
Enalapril therapy is generally not associated with undesirable effects on plasma uric acid concentration.
Enalapril therapy is associated with favorable effects on plasma lipoprotein fraction ratios and no or favorable effects on total cholesterol concentrations.
In patients with CH patients on therapy with cardiac glycosides and diuretics, enalapril administration caused reduction of total peripheral resistance and BP. Cardiac output increased, while HR (usually elevated in patients with CH) decreased. Pulmonary capillary congestion pressure also decreased.
The exercise tolerance and severity of CH, as assessed by New York Heart Association (NYHA) criteria, improved. These effects were observed with long-term therapy.
In patients with mild to moderate CHF severity, enalapril delayed progression of cardiac dilatation and CHF, as indicated by decreased left ventricular end-diastolic and systolic volumes and improved left ventricular ejection fraction.
The clinical data showed that enalapril reduces the incidence of ventricular arrhythmias in patients with CHF, although the underlying mechanisms and clinical significance of this effect are not known.
Pharmacokinetics
Enalapril is rapidly absorbed in the gastrointestinal tract after oral administration. Maximum serum concentration of enalapril is reached within 1 hour after oral administration. The degree of absorption of enalapril when taken orally is approximately 60%. Food intake has no effect on the absorption of enalapril.
Enalapril is rapidly hydrolyzed after absorption to form the active metabolite enalaprilate, a potent ACE inhibitor. Maximum serum concentration of enalaprilat is observed approximately 4 hours after an oral dose of enalapril.
The duration of absorption and hydrolysis of enalapril is similar for various recommended therapeutic doses. In healthy volunteers with normal renal function, the equilibrium serum concentration of enalaprilat is reached by day 4 from the start of enalapril administration.
Distribution
In therapeutic dose range, binding of enalaprilat to plasma proteins does not exceed 60%.
Metabolism
There are no data on other significant pathways of metabolism of enalapril other than hydrolysis to enalaprilat.
Elevation
Elevation of enalapril is primarily via the kidneys. The main metabolites detected in the urine are enalaprilate, accounting for approximately 40% of the dose, and unchanged enalapril (approximately 20%).
The plasma concentration curve of enalaprilat has a prolonged terminal phase apparently due to its binding to ACE. The elimination half-life of enalaprilat with oral administration is 11 hours.
Pharmacokinetics in special patient groups
Patients with impaired renal function
The area under the concentration-time curve (AUC) of enalapril and enalaprilat is increased in patients with renal impairment. In patients with mild to moderate renal impairment (creatinine clearance (CK) 40-60 mL/min), the equilibrium AUC of enalaprilat was approximately 2-fold higher after administration of enalapril at a dose of 5 mg once daily than in patients with unchanged renal function.
In patients with severe renal impairment (CK of 30 ml/min or less), the AUC was increased approximately 8-fold. The effective elimination half-life of enalaprilat after repeated administration of enalapril in patients with severe renal impairment was prolonged and the onset of equilibrium concentration of enalaprilat was delayed (see section “Dosage and administration”).
Enalaprilat may be eliminated from the general bloodstream by hemodialysis procedures. Clearance in hemodialysis is 62 ml/min.
Breastfeeding
After a single oral administration of enalapril at a dose of 20 mg in postpartum patients, the mean maximum concentration of enalapril in breast milk was 1.7 µg/L (0.54 to 5.9 µg/L) 4-6 hours after administration.
The mean maximum concentration of enalaprilat was 1.7 µg/L (1.2 to 2.3 µg/L) and was observed at various times within 24 hours of administration. Taking into account data on maximum concentrations in breast milk, the estimated maximum intake of enalapril in the fully breastfed infant is 0.16% of the dose based on maternal body weight.
In a woman who took enalapril orally at a dose of 10 mg once daily for 11 months, maximum concentrations of enalapril in breast milk were 2 μg/L 4 hours after administration; maximum enalaprilate concentrations were 0.75 μg/L approximately 9 hours after administration.
The mean concentrations in breast milk at 24 hours after enalapril administration were 1.44 mcg/L and enalaprilat was 0.63 mcg/L. One woman who took enalapril at a dose of 5 mg once and two women who took enalapril at a dose of 10 mg once had breast milk concentrations below the detectable level (less than 0.2 µg/L) 4 hours after ingestion. Their enalapril concentrations were not detectable.
Indications
Indications
Essential hypertension of any severity;
renovascular hypertension;
heart failure of any severity:
in patients with clinical manifestations of HF, Enalapril is also indicated for: increasing patient survival, slowing the progression of HF, reducing the frequency of hospitalizations for HF;
prevention of the development of clinically significant heart failure:
in patients without clinical symptoms of HF with left ventricular dysfunction, Enalapril is indicated for: slowing the development of clinical manifestations of HF, reducing the frequency of hospitalizations for HF;
prevention of coronary ischemia in patients with left ventricular dysfunction:
Enalapril is indicated for: reducing the incidence of myocardial infarction, reducing the frequency of hospitalizations for unstable angina.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: angiotensin-converting enzyme (ACE) inhibitor. ATX code: C09AA02
Enalapril belongs to drugs that affect the renin-angiotensin-aldosterone system (RAAS) – ACE inhibitors. The drug Enalapril is used for the treatment of essential hypertension (primary arterial hypertension (AH)) of any severity and renovascular hypertension, both in monotherapy and in combination with other antihypertensive drugs, in particular with diuretics. Enalapril is also used to treat or prevent the development of heart failure (HF).
Pharmacodynamics
Enalapril is a derivative of two amino acids, L-alanine and L-proline. After oral administration, enalapril is rapidly absorbed and hydrolyzed into enalaprilat, which is a highly specific and long-acting ACE inhibitor that does not contain a sulfhydryl group.
ACE (peptidyl dipeptidase A) catalyzes the conversion of angiotensin I to the pressor peptide angiotensin II. After absorption, enalapril is hydrolyzed to enalaprilat, which inhibits ACE. ACE inhibition leads to a decrease in the concentration of angiotensin II in the blood plasma, which entails an increase in plasma renin activity (due to the elimination of negative feedback in response to renin release) and a decrease in aldosterone secretion.
ACE is identical to the enzyme kininase II, so enalapril can also block the destruction of bradykinin, a peptide that has a pronounced vasodilating effect. The significance of this effect in the therapeutic action of enalapril requires clarification.
Despite the fact that the main mechanism by which enalapril reduces blood pressure (BP) is considered to be the suppression of the activity of the RAAS, which plays an important role in the regulation of blood pressure, enalapril exhibits an antihypertensive effect even in patients with hypertension and with reduced plasma renin activity.
The use of enalapril in patients with hypertension leads to a decrease in blood pressure both in the standing and lying positions without a significant increase in heart rate (HR).
Symptomatic postural hypotension occurs infrequently. In some patients, achieving optimal blood pressure reduction may require several weeks of therapy. Interruption of enalapril therapy does not cause a sharp rise in blood pressure.
Effective inhibition of ACE activity usually develops 2-4 hours after a single oral dose of enalapril. The antihypertensive effect develops within 1 hour, the maximum decrease in blood pressure is observed 4-6 hours after taking the drug. The duration of action depends on the dose. However, when using recommended doses, the antihypertensive effect and hemodynamic effects persist for 24 hours.
Antihypertensive therapy with enalapril leads to a significant regression of left ventricular hypertrophy and preservation of its systolic function.
In clinical hemodynamic studies in patients with essential hypertension, a decrease in blood pressure was accompanied by a decrease in total peripheral vascular resistance, an increase in cardiac output, and no or minor changes in heart rate. An increase in renal blood flow was observed after taking enalapril.
At the same time, the glomerular filtration rate (GFR) did not change, and there were no signs of sodium or fluid retention. However, in patients with initially reduced glomerular filtration rate, its rate usually increased.
Long-term use of enalapril in patients with essential hypertension and renal failure may lead to improved renal function, as evidenced by an increase in GFR.
In short clinical studies in patients with renal failure and with or without diabetes mellitus, a decrease in albuminuria, renal excretion of IgG, and a decrease in total urinary protein was observed after taking enalapril.
With simultaneous use of enalapril and thiazide diuretics, a more pronounced antihypertensive effect is observed. Enalapril reduces or prevents the development of hypokalemia caused by taking thiazides.
Enalapril therapy is not usually associated with undesirable effects on plasma uric acid concentrations.
Enalapril therapy is accompanied by a beneficial effect on the ratio of lipoprotein fractions in the blood plasma and no effect or a beneficial effect on the concentration of total cholesterol.
In patients with heart failure during therapy with cardiac glycosides and diuretics, taking enalapril caused a decrease in total peripheral resistance and blood pressure. Cardiac output increased, while heart rate (usually elevated in patients with HF) decreased. Wedge pressure in the pulmonary capillaries also decreased.
Exercise capacity and HF severity, as assessed by New York Heart Association (NYHA) criteria, improved. These effects were observed with long-term therapy.
In patients with mild to moderate HF, enalapril slowed the progression of cardiac dilatation and HF, as demonstrated by a decrease in left ventricular end-diastolic and systolic volumes and an improvement in left ventricular ejection fraction.
Clinical data have shown that enalapril reduces the incidence of ventricular arrhythmias in patients with HF, although the underlying mechanisms and clinical significance of this effect are unknown.
Pharmacokinetics
Suction
After oral administration, enalapril is rapidly absorbed from the gastrointestinal tract. The maximum concentration of enalapril in the blood serum is achieved within 1 hour after oral administration. The degree of absorption of enalapril when taken orally is approximately 60%. Eating does not affect the absorption of enalapril.
After absorption, enalapril is rapidly hydrolyzed to form the active metabolite enalaprilat, a powerful ACE inhibitor. The maximum concentration of enalaprilat in the blood serum occurs approximately 4 hours after taking an oral dose of enalapril.
The duration of absorption and hydrolysis of enalapril is similar for various recommended therapeutic doses. In healthy volunteers with normal renal function, the equilibrium concentration of enalaprilat in the blood serum is achieved by 4 days from the start of taking enalapril.
Distribution
In the range of therapeutic doses, the binding of enalaprilat to plasma proteins does not exceed 60%.
Metabolism
There is no data on other significant pathways of metabolism of enalapril other than hydrolysis to enalaprilat.
Removal
Enalapril is excreted primarily through the kidneys. The main metabolites detected in urine are enalaprilat, accounting for approximately 40% of the dose, and unchanged enalapril (approximately 20%).
The plasma concentration curve of enalaprilat has a long terminal phase, apparently due to its binding to ACE. The half-life of enalaprilat during a course of oral administration of the drug is 11 hours.
Pharmacokinetics in special groups of patients
Patients with impaired renal function
The area under the concentration-time curve (AUC) of enalapril and enalaprilat is increased in patients with renal impairment. In patients with mild to moderate renal failure (creatinine clearance (CC) 40-60 ml/min) after taking enalapril at a dose of 5 mg 1 time per day, the steady-state AUC value of enalaprilat was approximately 2 times higher than in patients with unchanged renal function.
In patients with severe renal failure (creatinine clearance less than 30 ml/min), the AUC value increased approximately 8-fold. The effective half-life of enalaprilat after repeated use of enalapril in patients with severe renal impairment increased, and the onset of steady-state enalaprilat concentrations was delayed (see section “Dosage and Administration”).
Enalaprilat can be removed from the general circulation using hemodialysis. Clearance during hemodialysis is 62 ml/min.
Breast-feeding
After a single oral administration of enalapril at a dose of 20 mg in postpartum patients, the average maximum concentration of enalapril in breast milk was 1.7 μg/L (from 0.54 to 5.9 μg/L) 4-6 hours after administration.
The mean maximum concentration of enalaprilat was 1.7 mcg/L (range 1.2 to 2.3 mcg/L) and was observed at various times within 24 hours after dosing. Based on data on maximum concentrations in breast milk, the estimated maximum intake of enalapril for a fully breastfed infant is 0.16% of the dose calculated based on maternal body weight.
In a woman who took enalapril orally at a dose of 10 mg once daily for 11 months, the maximum concentrations of enalapril in breast milk were 2 μg/L 4 hours after dosing, the maximum concentrations of enalaprilat were 0.75 μg/L approximately 9 hours after dosing.
The average concentration in breast milk within 24 hours after taking enalapril was 1.44 mcg/l and enalaprilat – 0.63 mcg/l. One woman who took a single dose of enalapril 5 mg and two women who took a single dose of enalapril 10 mg had breast milk concentrations of enalaprilat below detectable levels (less than 0.2 mcg/L) 4 hours after dosing. Their enalapril concentration was not determined.
Special instructions
Special instructions
Symptomatic hypotension
Symptomatic hypotension is rarely observed in patients with uncomplicated hypertension. In patients with hypertension taking enalapril, arterial hypotension develops more often against the background of dehydration, which occurs, for example, as a result of diuretic therapy, limiting salt intake, in patients on dialysis, as well as in patients with diarrhea or vomiting.
Symptomatic arterial hypotension has been observed in patients with CHF with or without chronic renal failure.
Hypotension is more likely to occur in patients with more severe heart failure with hyponatremia or impaired renal function who are treated with higher doses of loop diuretics. In such patients, treatment with enalapril should be initiated under medical supervision, which should be especially careful when changing the dose of enalapril and/or diuretic.
Likewise, patients with coronary artery disease or cerebrovascular disease, in whom an excessive decrease in blood pressure may lead to the development of myocardial infarction or stroke, should be monitored.
If arterial hypotension develops, the patient should be placed in a horizontal position and, if necessary, administered a 0.9% sodium chloride solution. Transient arterial hypotension when taking enalapril is not a contraindication to further use and increasing the dose of enalapril, which can be continued after fluid replenishment and blood pressure normalization.
In some patients with CHF and with normal or reduced blood pressure, enalapril may cause an additional decrease in blood pressure. This reaction to taking enalapril is expected and is not a reason to stop treatment. In cases where arterial hypotension becomes stable, the dose should be reduced and/or discontinued use of the diuretic and/or enalapril.
Aortic stenosis / mitral stenosis / hypertrophic obstructive cardiomyopathy
Like all drugs that have a vasodilating effect, ACE inhibitors should be used with caution in patients with left ventricular outflow tract obstruction.
Renal dysfunction
In patients with impaired renal function (creatinine clearance <80 ml/min), the initial dose and/or frequency of enalapril should be reduced depending on the creatinine clearance. In such cases, renal function (creatinine and potassium levels in the blood) should be regularly monitored during the first few weeks of treatment.
In some patients, hypotension that develops after initiation of treatment with ACE inhibitors may lead to deterioration of renal function. Cases of the development of oliguria, progressive azotemia and acute renal failure (including fatal outcomes) have been described with the use of ACE inhibitors, mainly in patients with chronic heart failure or concomitant kidney disease (including renal artery stenosis).
With timely detection and appropriate treatment, acute renal failure caused by the use of ACE inhibitors is usually reversible.
In some patients without signs of kidney disease before treatment, the use of enalapril in combination with diuretics caused an increase in serum urea and creatinine concentrations. In such cases, it may be necessary to reduce the dose and/or discontinue the diuretic and/or enalapril.
It is recommended to conduct an appropriate examination, since these abnormalities may be a sign that the patient has previously unrecognized renal artery stenosis.
Renovascular hypertension
Patients with bilateral renal artery stenosis or stenosis of the artery of a solitary kidney have an increased risk of developing arterial hypotension and renal failure when using ACE inhibitors. Renal failure may initially manifest itself as only slight changes in plasma creatinine levels. The use of enalapril drugs in such patients should be started with low doses, under close medical supervision and monitoring of renal function.
Kidney transplant
There is no experience with the use of enalapril in patients who have recently undergone kidney transplantation. Therefore, the use of enalapril in such patients is not recommended.
Liver dysfunction
The use of ACE inhibitors in rare cases has been accompanied by the development of a syndrome starting with cholestatic jaundice or hepatitis and progressing to fulminant liver necrosis, sometimes with death. The mechanism of development of this syndrome is unknown.
If jaundice appears or a significant increase in the activity of “liver” transaminases during the use of the drug, you should stop taking enalapril and prescribe appropriate auxiliary therapy. The patient should be under appropriate supervision.
Neutropenia / agranulocytosis / thrombocytopenia / anemia
Cases of neutropenia/agranulocytosis, thrombocytopenia and anemia have been reported in patients taking ACE inhibitors. In patients with normal renal function and no other complicating factors, neutropenia rarely occurs.
Enalapril should be used with extreme caution in patients with systemic connective tissue diseases (systemic lupus erythematosus, scleroderma and others) taking immunosuppressive therapy, allopurinol or procainamide, or a combination of these complicating factors, especially if there are impaired renal function.
Some patients developed serious infectious diseases, which in some cases did not respond to intensive antibiotic therapy.
When using enalapril in patients with a high risk of neutropenia/agranulocytosis, regular monitoring of the number of leukocytes in the blood is recommended. Patients should be warned to seek immediate medical attention if any signs of an infectious disease (eg, fever, sore throat) occur.
Hypersensitivity reactions/angioedema
Rare cases of angioedema of the face, extremities, lips, tongue, vocal folds and/or larynx have been observed with the use of ACE inhibitors, including enalapril. Angioedema may develop at any time during treatment.
In such cases, you should immediately stop taking enalapril and carefully monitor the patient’s condition in order to monitor and correct clinical symptoms. Even in cases where only swelling of the tongue is observed without the development of respiratory distress syndrome, patients may require long-term observation, since therapy with antihistamines and corticosteroids may not be sufficient.
Angioedema, associated with swelling of the larynx and tongue, can be fatal in very rare cases. Swelling of the tongue, vocal folds, or larynx can lead to airway obstruction, especially in patients who have undergone respiratory surgery.
If airway obstruction develops, appropriate treatment should be immediately prescribed, including subcutaneous administration of 0.3-0.5 ml of a 0.1% solution of epinephrine (adrenaline) and/or ensuring airway patency (intubation or tracheostomy).
In rare cases, intestinal edema (angioedema of the intestine) develops during therapy with ACE inhibitors. In this case, patients experience abdominal pain as an isolated symptom or in combination with nausea and vomiting, in some cases without previous angioedema of the face and with normal levels of C1-esterase.
Diagnosis is made using abdominal computed tomography, ultrasound, or surgery. Symptoms disappeared after stopping the ACE inhibitors. The possibility of developing intestinal edema must be taken into account when carrying out the differential diagnosis of abdominal pain in patients taking ACE inhibitors.
Patients with a history of angioedema not associated with ACE inhibitors may be at greater risk of developing angioedema during ACE inhibitor therapy.
In black patients taking ACE inhibitors, angioedema was observed more often than in representatives of other races.
An increased risk of developing angioedema has been observed in patients concomitantly taking ACE inhibitors and drugs such as mTOR inhibitors (temsirolimus, sirolimus, everolimus),
dipeptidyl peptidase type IV (sitagliptin, saxagliptin, vildagliptin, linagliptin), estramustine, neutral endopeptidase inhibitors (racecadotril).
Anaphylactoid reactions during desensitization with an allergen from Hymenoptera venom
In rare cases, patients taking ACE inhibitors have developed life-threatening anaphylactoid reactions during desensitization with hymenoptera venom allergen.
Adverse reactions can be avoided if you temporarily stop taking the ACE inhibitor before starting desensitization. The use of enalapril should be avoided in patients receiving bee venom immunotherapy.
Anaphylactoid reactions during low-density lipoprotein apheresis (LDL apheresis)
Life-threatening anaphylactoid reactions have rarely been observed in patients taking ACE inhibitors during LDL apheresis using dextran sulfate. The development of these reactions can be prevented by temporarily discontinuing the ACE inhibitor before each LDL apheresis procedure.
Hemodialysis using high-flow membranes
Anaphylactoid reactions have been observed in patients on dialysis using high-flux polyacrylonitrile membranes (such as AN69®) and concomitantly receiving ACE inhibitor therapy. In such cases, it is necessary to use a different type of dialysis membrane or use antihypertensive drugs of other classes.
Diabetes mellitus
When using enalapril drugs in patients with diabetes mellitus who are receiving oral hypoglycemic agents or insulin, it is necessary to regularly monitor the concentration of glucose in the blood. Patients taking oral hypoglycemic agents or insulin should be informed before starting the use of ACE inhibitors of the need to regularly monitor blood glucose concentrations (hypoglycemia), especially during the first month of simultaneous use of these drugs.
Cough
Cases of cough occurring during therapy with ACE inhibitors have been observed. As a rule, the cough is non-productive, constant and stops after discontinuation of the drug. Cough associated with the use of ACE inhibitors should be considered in the differential diagnosis of dry cough.
Surgical interventions / general anesthesia
During major surgical procedures or during general anesthesia with the use of agents with antihypertensive effects, enalaprilat blocks the formation of angiotensin II caused by the compensatory release of renin. If a pronounced decrease in blood pressure develops, explained by a similar mechanism, it can be corrected by increasing the volume of circulating blood.
Hyperkalemia
Hyperkalemia may develop during therapy with ACE inhibitors, including enalapril. Risk factors for the development of hyperkalemia are renal failure, old age (over 65 years), diabetes mellitus, some concomitant conditions (decrease in volumetric volume, acute heart failure in the decompensation stage, metabolic acidosis), simultaneous use of potassium-sparing diuretics (such as spironolactone, eplerenone, triamterene or amiloride), as well as potassium supplements, potassium-containing substitutes for table salt and other drugs that help increase potassium levels in the blood plasma (such as heparin, tacrolimus, cyclosporine; drugs containing co-trimoxazole [trimethoprim + sulfamethoxazole]).
The use of potassium supplements, potassium-sparing diuretics, or potassium-containing table salt substitutes, especially in patients with impaired renal function, can lead to a significant increase in serum potassium levels. Hyperkalemia can cause serious heart rhythm disturbances, sometimes fatal.
If it is necessary to use enalapril simultaneously and the drugs listed above containing potassium or increasing the potassium content in the blood plasma, caution should be exercised and the potassium content in the blood serum should be regularly monitored.
Hypokalemia
When using ACE inhibitors simultaneously with thiazide diuretics, the risk of hypokalemia cannot be excluded, therefore, in such cases, regular monitoring of potassium levels in the blood during therapy should be carried out.
Dual blockade of the renin-angiotensin-aldosterone system (RAAS)
Hypotension, syncope, stroke, hyperkalemia and renal dysfunction (including acute renal failure) have been reported in susceptible patients, especially when combined therapy with drugs that affect the RAAS is used.
The simultaneous use of ACE inhibitors with medicinal products containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
Concomitant use of ACE inhibitors with angiotensin II receptor antagonists is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
In cases where the simultaneous administration of two drugs acting on the RAAS is necessary, their use should be carried out under the supervision of a physician with extreme caution and with regular monitoring of renal function, blood pressure and electrolyte levels in the blood plasma.
Lithium preparations
The simultaneous use of enalapril and drugs containing lithium is not recommended.
Alcohol
During the treatment period, it is not recommended to drink alcoholic beverages, since ethanol enhances the antihypertensive effect of ACE inhibitors.
Use in elderly patients
Clinical studies of the efficacy and safety of enalapril were similar in older and younger patients with hypertension.
Ethnic differences
Enalapril, like other ACE inhibitors, has a less pronounced antihypertensive effect in black patients compared to representatives of other races, which may be explained by a higher prevalence of conditions with low plasma renin activity in black patients with arterial hypertension.
Discontinuation of therapy
Sudden cessation of taking enalapril usually does not lead to the development of withdrawal syndrome.
Impact on the ability to drive vehicles and machinery
The effect of Enalapril on the ability to drive vehicles and operate machinery has not been studied. However, some undesirable effects (for example, dizziness) that were observed while taking Enalapril may affect the ability to drive vehicles and operate machines (see section “Side effects”).
Active ingredient
Active ingredient
Enalapril
Composition
Composition
Active ingredient: enalapril maleate – 5.0 mg, 10.0 mg, 20.0 mg; excipients: lactose monohydrate, potato starch, povidone K 30, calcium stearate
Pregnancy
Pregnancy
Pregnancy
The use of Enalapril during pregnancy is not recommended. If pregnancy is diagnosed, Enalapril should be discontinued immediately unless the drug is considered essential for the mother.
A published retrospective epidemiologic study of infants whose mothers took ACE inhibitors during the first trimester of pregnancy reported an increased risk of major congenital malformations compared with infants whose mothers did not take ACE inhibitors during the first trimester of pregnancy.
The incidence of birth defects was low and the results of this study have not been reconfirmed.
ACE inhibitors may cause disease or death of the fetus or newborn when used by pregnant women during the second and third trimesters of pregnancy.
The use of ACE inhibitors during these periods was accompanied by a negative effect on the fetus and newborn, which manifested itself in the form of arterial hypotension, renal failure, hyperkalemia and/or hypoplasia of the skull bones in the newborn. Prematurity, intrauterine growth restriction, and patent ductus arteriosus have also been reported, but it is unclear whether these cases were associated with ACE inhibitors.
It is possible that the development of oligohydramnios occurs due to a decrease in fetal renal function. This complication can lead to contracture of the limbs, deformation of the bones of the skull, including its facial part, and hypoplasia of the fetal lungs. When prescribing Enalapril during pregnancy, the patient must be informed of the potential risk to the fetus.
These undesirable effects on the embryo and fetus do not appear to be the result of intrauterine exposure to ACE inhibitors during the first trimester of pregnancy.
In those rare cases where the use of an ACE inhibitor during pregnancy is considered necessary, periodic ultrasound examinations should be performed to assess the amniotic fluid index.
If oligohydramnios is detected during an ultrasound examination, it is necessary to stop taking Enalapril, unless the drug is considered vital for the mother. However, both the patient and the physician should be aware that oligohydramnios occurs when the fetus is irreversibly damaged.
If ACE inhibitors are used during pregnancy and oligohydramnios develops, depending on the week of pregnancy, a stress test, a non-stress test, or a fetal biophysical profile may be necessary to assess fetal function.
Newborns whose mothers took Enalapril during pregnancy should be carefully monitored for hypotension, oliguria and hyperkalemia.
With the development of oliguria, special attention should be paid to maintaining blood pressure and renal perfusion. Enalapril penetrates the placental barrier. It can be partially removed from the newborn’s circulation using peritoneal dialysis. Theoretically, it can also be removed by exchange transfusion.
Breastfeeding period
Enalapril and enalaprilat are excreted in trace amounts in mother’s breast milk. If it is necessary to use the drug during breastfeeding, the patient should stop breastfeeding.
Contraindications
Contraindications
Hypersensitivity to enalapril and other ACE inhibitors; a history of angioedema associated with treatment with ACE inhibitors; simultaneous use with aliskiren and drugs containing aliskiren in patients with diabetes mellitus and/or moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area); simultaneous use with angiotensin II receptor antagonists (ARA II) in patients with diabetic nephropathy; porphyria; pregnancy; breastfeeding period; age under 18 years (efficacy and safety have not been established); hereditary lactose intolerance, lactase deficiency, glucose-galactose malabsorption syndrome.
With caution
Arterial hypotension, bilateral renal artery stenosis or stenosis of the artery of a single kidney; renovascular hypertension; renal failure; condition after kidney transplantation; aortic or mitral stenosis; hypertrophic obstructive cardiomyopathy; chronic heart failure; coronary heart disease or cerebrovascular diseases; systemic connective tissue diseases (systemic lupus erythematosus, scleroderma, etc.), inhibition of bone marrow hematopoiesis, immunosuppressive therapy, simultaneous use of allopurinol or procainamide, or a combination of these complicating factors (risk of developing neutropenia and agranulocytosis); liver failure; diabetes mellitus; hyperkalemia; simultaneous use with potassium-sparing diuretics, potassium preparations, potassium-containing substitutes for table salt; simultaneous use with lithium preparations; a history of severe allergies or angioedema; simultaneous desensitization with an allergen from Hymenoptera venom; simultaneous low-density lipoprotein apheresis (LDL apheresis) using dextran sulfate; hemodialysis using high-flux membranes (such as AN69®); conditions accompanied by a decrease in circulating blood volume (including during diuretic therapy, following a diet with limited salt, dialysis, diarrhea or vomiting) and hyponatremia; use during major surgical procedures or during general anesthesia; use in patients of the Negroid race; use in elderly patients (over 65 years old).
Side Effects
Side Effects
In general, Enalapril Renewal was well tolerated. In clinical studies, the total incidence of adverse events (AEs) when using the drug Enalapril Renewal did not exceed that when taking placebo. In most cases, AEs were mild, transient and did not require discontinuation of therapy. To assess the frequency of AEs, the following criteria were used: “very often” (≥ 1/10); “often” (≥ 1/100, < 1/10); “uncommon” (≥ 1/1000, < 1/100); “rare” (≥ 1/10000, < 1/1000); “very rare” (< 1/10000); “frequency unknown” (it is impossible to estimate the frequency based on the available data). AEs are grouped in accordance with the system-organ classes of the medical dictionary for regulatory activities MedDRA; within each class, AEs are listed in descending order of frequency of occurrence; within each group, allocated by frequency of occurrence, AEs are distributed in decreasing order of their importance.
Blood and lymphatic system disorders
Uncommon: anemia (including aplastic and hemolytic).
Rarely: neutropenia, decreased hemoglobin, decreased hematocrit, thrombocytopenia, agranulocytosis, suppression of bone marrow function, pancytopenia, lymphadenopathy, autoimmune diseases.
Endocrine system disorders
Frequency unknown: syndrome of inappropriate antidiuretic hormone secretion.
Metabolic and nutritional disorders
Uncommon: hypoglycemia (see section “Special instructions”).
Nervous system and mental disorders
Common: headache, depression.
Uncommon: confusion, drowsiness, insomnia, nervousness, paresthesia, systemic dizziness.
Rarely: unusual dreams, sleep disturbances.
Visual disorders
Very common: blurred vision.
Disorders of the heart and blood vessels
Very common: dizziness.
Often: marked decrease in blood pressure, fainting, chest pain, arrhythmia, angina pectoris, tachycardia.
Uncommon: orthostatic hypotension, palpitations, myocardial infarction or stroke*, possibly secondary to severe hypotension in patients at high risk (see section “Special Instructions”).
Rarely: Raynaud’s syndrome.
Respiratory, thoracic and mediastinal disorders
Very common: cough.
Common: shortness of breath.
Uncommon: rhinorrhea, sore throat, hoarseness, bronchospasm/bronchial asthma.
Rarely: pulmonary infiltrates, rhinitis, allergic alveolitis/eosinophilic pneumonia.
Digestive system disorders
Very common: nausea.
Common: diarrhea, abdominal pain, taste disturbance.
Uncommon: intestinal obstruction, pancreatitis, vomiting, dyspepsia, constipation, anorexia, gastric irritation, dry mouth, gastric and duodenal ulcers.
Rarely: stomatitis/aphthous ulcers, glossitis.
Very rare: intestinal edema.
Disorders of the liver and biliary tract
Rare: liver failure, hepatitis (hepatocellular or cholestatic), hepatitis (including necrosis), cholestasis (including jaundice).
Skin and subcutaneous tissue disorders
Common: skin rash, hypersensitivity reactions/angioedema: angioedema of the face, extremities, lips, tongue, vocal folds and/or larynx (see section “Special Instructions”).
Uncommon: increased sweating, itching, urticaria, alopecia.
Rarely: erythema multiforme, Stevens-Johnson syndrome, exfoliative dermatitis, toxic epidermal necrolysis, pemphigus, erythroderma.
A symptom complex has been reported that may include all or some of the following symptoms: fever, serositis, vasculitis, myalgia/myositis, arthralgia/arthritis, positive antinuclear antibody test, increased erythrocyte sedimentation rate (ESR), eosinophilia and leukocytosis. Skin rash, photosensitivity and other skin reactions may also occur.
Renal and urinary tract disorders
Uncommon: renal dysfunction, renal failure, proteinuria.
Rarely: oliguria.
Disorders of the genital organs and breast
Uncommon: erectile dysfunction.
Rare: gynecomastia.
General disorders
Very common: asthenia.
Common: increased fatigue.
Uncommon: muscle cramps, flushes of blood to the facial skin, tinnitus, discomfort, fever.
Laboratory and instrumental data
Common: hyperkalemia, increased serum creatinine concentration.
Uncommon: increased concentration of urea in the blood, hyponatremia.
Rarely: increased activity of liver transaminases, increased concentration of bilirubin in the blood serum.
* Incidence rates were comparable to those observed in clinical trials with placebo or another comparator drug.
The following adverse events were identified during post-registration surveillance, but a cause-and-effect relationship with taking the drug Enalapril reneval has not been established: urinary tract infections, upper respiratory tract infections, bronchitis, cardiac arrest, atrial fibrillation, herpes zoster, melena, ataxia, thromboembolism of the branches of the pulmonary artery and pulmonary infarction, hemolytic anemia, including cases of hemolysis in patients with glucose-6-phosphate dehydrogenase deficiency.
It is important to report the development of adverse reactions to ensure continuous monitoring of the benefit-risk ratio of the drug. If any of the side effects indicated in the instructions get worse, or you notice any other side effects not listed in the instructions, tell your doctor. Healthcare professionals report any adverse drug reactions through national adverse event reporting systems.
Interaction
Interaction
Dual blockade of the renin-angiotensin-aldosterone system (RAAS)
Dual blockade of the RAAS with APA II, ACE inhibitors or aliskiren (renin inhibitor) is associated with an increased risk of hypotension, syncope, hyperkalemia and renal dysfunction (including acute renal failure) compared with monotherapy.
Regular monitoring of blood pressure, renal function and electrolyte levels in the blood is necessary in patients taking enalapril and other drugs that affect the RAAS at the same time.
The simultaneous use of ACE inhibitors with medicinal products containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
Concomitant use of ACE inhibitors with angiotensin II receptor antagonists (APA II) is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Potassium-sparing diuretics, potassium preparations, potassium-containing table salt substitutes and other drugs that can increase the potassium content in the blood serum
Concomitant use of enalapril with potassium-sparing diuretics (such as spironolactone, eplerenone, triamterene, amiloride), potassium preparations, potassium-containing table salt substitutes and other drugs that can increase potassium levels in the blood serum (including angiotensin II receptor antagonists, heparin, tacrolimus, cyclosporine; drugs containing co-trimoxazole [trimethoprim + sulfamethoxazole]) can lead to a significant increase in plasma potassium levels. If it is necessary to use enalapril with the drugs listed above, regular monitoring of potassium levels in the blood plasma should be carried out.
Potassium-sparing (thiazide and loop) diuretics
The use of diuretics in high doses can lead to hypovolemia (due to a decrease in blood volume), and the addition of enalapril to therapy can lead to a pronounced decrease in blood pressure. Excessive antihypertensive effect of enalapril can be reduced either by discontinuing the diuretic, or by increasing the volume of blood volume or consuming table salt, as well as by reducing the dose of enalapril.
With simultaneous use of enalapril with potassium-sparing (thiazide or loop) diuretics, hypokalemia caused by the action of diuretics is usually weakened due to the effect of enalapril.
Other antihypertensive drugs
An additive effect may be observed with concomitant use of enalapril and other antihypertensive therapy.
When enalapril is used concomitantly with other antihypertensive drugs, especially diuretics, an enhanced antihypertensive effect may be observed.
The simultaneous use of enalapril with beta-blockers, methyldopa or blockers of “slow” calcium channels increased the severity of the antihypertensive effect.
The simultaneous use of enalapril with alpha-blockers, beta-blockers and ganglion blockers should be carried out under close medical supervision.
The simultaneous use of enalapril with nitroglycerin, other nitro-containing drugs or other vasodilators enhances the antihypertensive effect.
Lithium preparations
Like other drugs that affect sodium excretion, ACE inhibitors may reduce the renal excretion of lithium and lead to increased cardiotoxic and neurotoxic effects of lithium. If simultaneous use of drugs containing lithium and ACE inhibitors is necessary, the concentration of lithium in the blood serum should be regularly monitored.
Nonsteroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors and high doses of acetylsalicylic acid (≥ 3 g/day)
NSAIDs, including selective cyclooxygenase-2 (COX-2) inhibitors and acetylsalicylic acid in doses of 3 g/day and above, may reduce the antihypertensive effect of diuretics and other antihypertensive drugs. As a result, the antihypertensive effect of angiotensin II receptor antagonists (APA II) or ACE inhibitors may be weakened when used simultaneously with NSAIDs, including selective COX-2 inhibitors.
In some patients with compromised renal function (for example, elderly or dehydrated patients, including those taking diuretics) receiving NSAID therapy (including selective COX-2 inhibitors), concomitant use of ACE or APA II inhibitors may cause a further deterioration of renal function, including the development of acute renal failure, and hyperkalemia.
These effects are usually reversible. The simultaneous use of ACE inhibitors and NSAIDs should be used with caution (especially in elderly patients and in patients with impaired renal function). Patients should receive adequate fluids. It is recommended to carefully monitor renal function, both at the beginning and during treatment.
The use of enalapril in combination with acetylsalicylic acid as an antiplatelet agent is not contraindicated.
Hypoglycemic drugs
Epidemiological studies have shown that the simultaneous use of ACE inhibitors and hypoglycemic drugs (insulin, oral hypoglycemic drugs) may enhance the hypoglycemic effect of the latter with the risk of developing hypoglycemia. This phenomenon, as a rule, was most often observed during the first weeks of combination therapy, as well as in patients with impaired renal function.
In patients with diabetes mellitus taking oral hypoglycemic drugs or insulin, blood glucose concentrations should be regularly monitored, especially during the first month of concomitant use with ACE inhibitors.
Tricyclic antidepressants / antipsychotics / general anesthetics / narcotics
Strengthening the antihypertensive effect of ACE inhibitors (further reduction in blood pressure with simultaneous use) and increasing the risk of developing orthostatic hypotension.
Alpha and beta adrenergic agonists
Alpha and beta adrenergic agonists (sympathomimetics), such as epinephrine (adrenaline), isoproterenol, dobutamine, dopamine, may reduce the antihypertensive effect of ACE inhibitors.
Baclofen
Enhances the antihypertensive effect of ACE inhibitors. Blood pressure should be carefully monitored and, if necessary, the dosage of antihypertensive drugs should be adjusted.
Ethanol
Ethanol enhances the antihypertensive effect of ACE inhibitors.
Theophylline
Enalapril weakens the effect of medications containing theophylline.
Estrogens
Estrogens weaken the antihypertensive effect of enalapril due to fluid retention.
Allopurinol, procainamide, cytostatics, immunosuppressants, glucocorticosteroids (for systemic use)
Concomitant use with ACE inhibitors may increase the risk of developing neutropenia/agranulocytosis.
Gold preparations
With the simultaneous use of gold preparations for parenteral administration (sodium aurothiomalate) and ACE inhibitors, including enalapril, a symptom complex (nitrate-like reactions) has been described, including a “rush” of blood to the facial skin, nausea, vomiting and arterial hypotension.
mTOR (mammalion Target of Rapamycin) inhibitors (eg, temsirolimus, sirolimus, everolimus)
In patients taking ACE inhibitors and mTOR inhibitors simultaneously (temsirolimus, sirolimus, everolimus), an increased incidence of angioedema was observed.
Dipeptidyl peptidase type IV (DPP-IV) inhibitors (gliptins), eg sitagliptin, saxagliptin, vildagliptin, linagliptin
An increased incidence of angioedema was observed in patients taking ACE inhibitors and dipeptidyl peptidase type IV inhibitors (gliptins) simultaneously.
Estramustine
Increased incidence of angioedema when used simultaneously with ACE inhibitors.
Neutral endopeptidase inhibitors (NEP)
An increased risk of angioedema has been reported with concomitant use of ACE inhibitors and racecadotril (an enkephalinase inhibitor).
Acetylsalicylic acid, thrombolytics and beta-blockers
Enalapril can be used simultaneously with acetylsalicylic acid (as an antiplatelet agent), thrombolytics and beta-blockers.
Pharmacokinetic interactions
Antacids
The bioavailability of ACE inhibitors may decrease.
Other medicines
No clinically significant pharmacokinetic drug interactions were observed between enalapril and the following drugs: hydrochlorothiazide, furosemide, digoxin, timolol, methyldopa, warfarin, indomethacin, sulindac and cimetidine.
With the simultaneous use of enalapril and propranolol, the concentration of enalaprilat in the blood serum decreases, but this effect is not clinically significant.
Overdose
Overdose
Information on overdose is limited. The most characteristic symptoms of overdose: a pronounced decrease in blood pressure, beginning approximately 6 hours after taking the drug simultaneously with blockade of the RAAS, and stupor. Enalaprilat serum concentrations 100 and 200 times higher than those observed at therapeutic doses occurred after taking 300 mg and 440 mg of enalapril, respectively.
Recommended treatment of overdose: intravenous infusion of 0.9% sodium chloride solution. If the drug was recently taken, induce vomiting. Enalaprilat can be removed from the systemic circulation by hemodialysis (see section “Special instructions” Patients on hemodialysis).
Storage conditions
Storage conditions
In the original packaging (blister packaging in a pack) at a temperature not exceeding 30 °C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after expiration date.
Manufacturer
Manufacturer
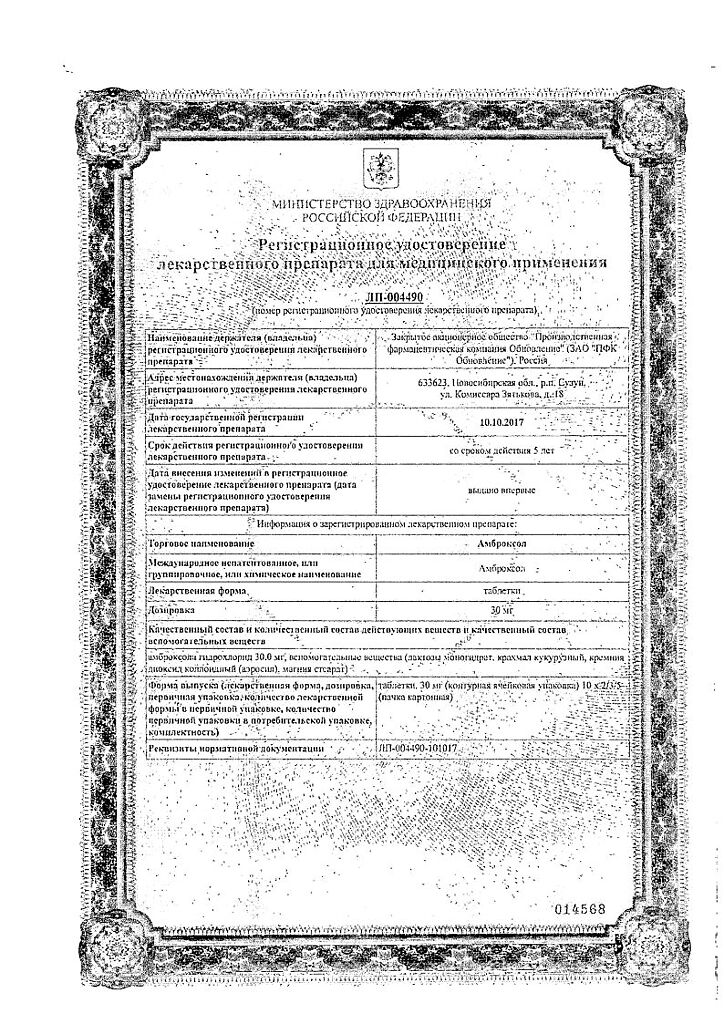
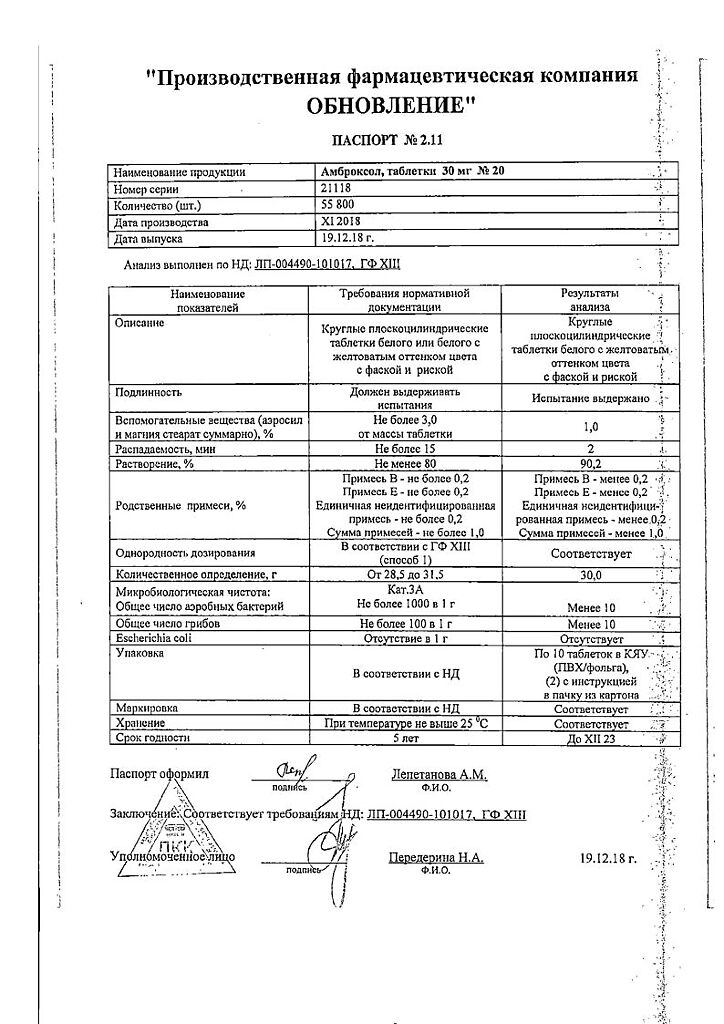
Update of PFC JSC, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In the original package (in a box in a package) at a temperature not exceeding 30 °С. Keep out of reach of children. |
| Manufacturer | Update PFC AO, Russia |
| Medication form | pills |
| Brand | Update PFC AO |
Other forms…
Related products
Buy Enalapril Reneval, tablets 10 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.