No products in the cart.
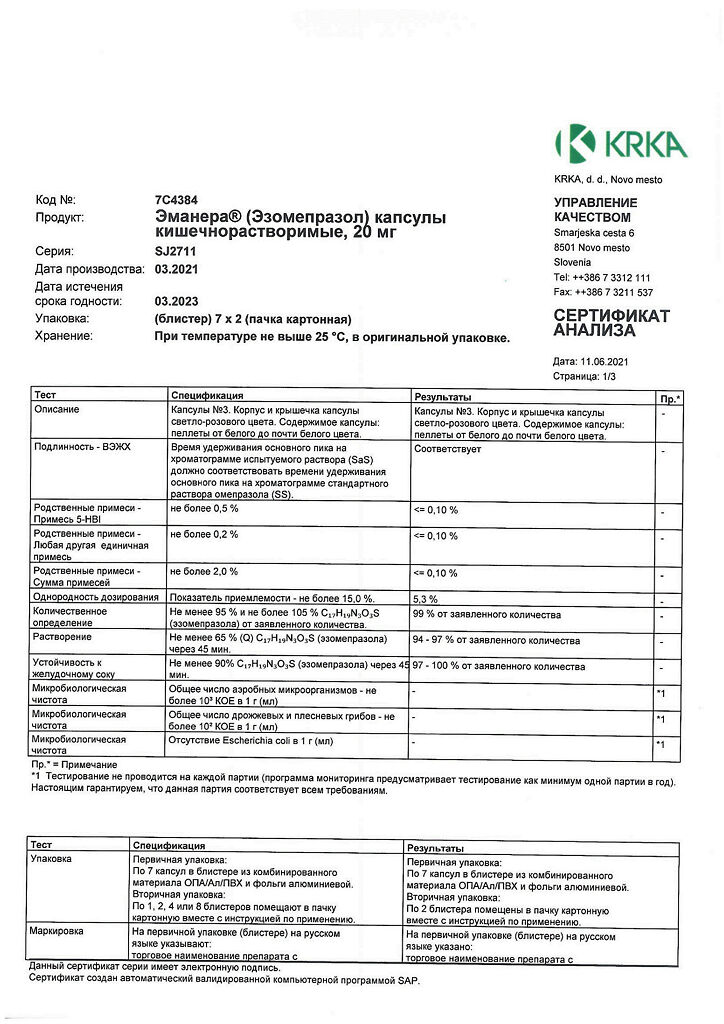
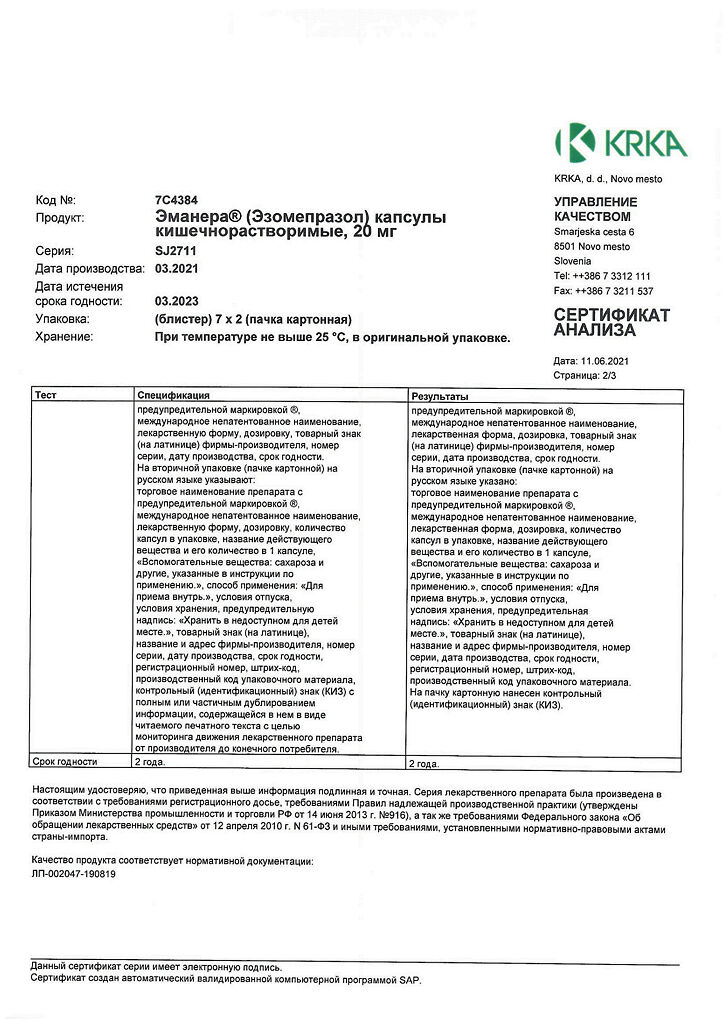
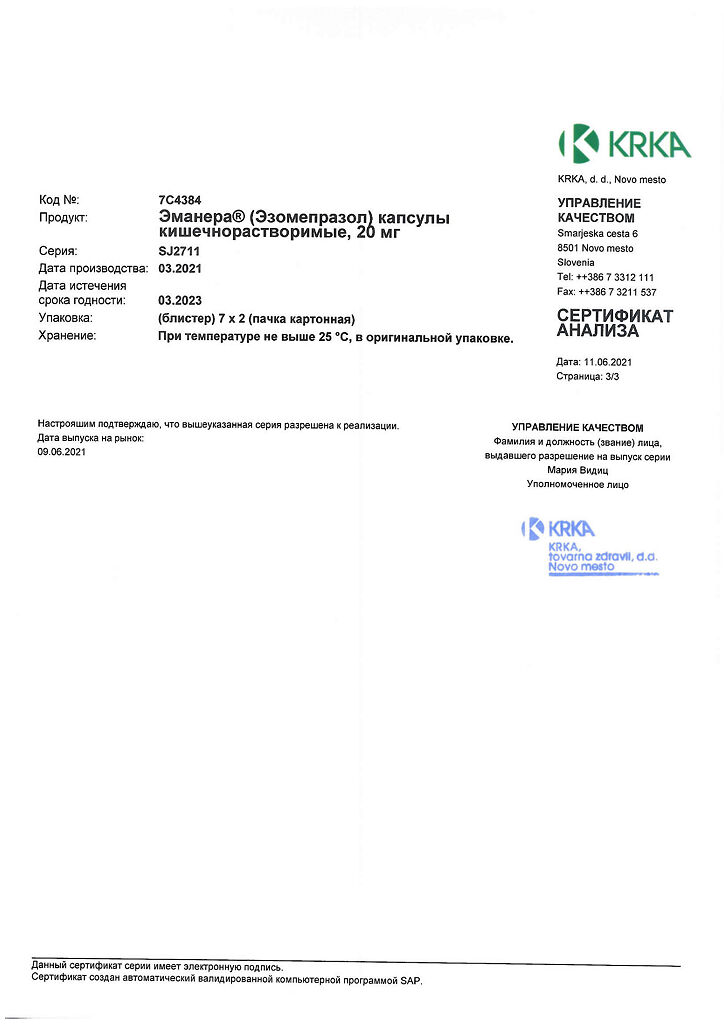
Emanera, 20 mg capsules 14 pcs
€1.00
Out of stock
(E-mail when Stock is available)
EAN: 3838989625603
SKU: 221636
Categories: Medicine, Stomach, intestines, liver, Ulcer and gastritis
Description
Reflux esophagitis, Sour belching, Gastric and duodenal ulcers, GI infections caused by Helicobacter pylori, Heartburn, Pelvic pain
Gastroesophageal reflux disease (GERD):
treatment of erosive reflux esophagitis;
long-term maintenance treatment after healing of erosive reflux esophagitis to prevent relapse;
symptomatic treatment for GERD.
gastric and duodenal ulcer.
As part of the combined therapy:
– treatment of duodenal ulcer associated with Helicobacter pylori;
– prevention of recurrence of peptic ulcer associated with Helicobacter pylori.
Long-term acid-suppressive therapy in patients who have suffered bleeding from a peptic ulcer (after intravenous use of drugs that reduce gastric gland secretion to prevent recurrence).
Patients taking nonsteroidal anti-inflammatory drugs (NSAIDs) for a long time:
– healing of gastric ulcers associated with taking NSAIDs;
– prevention of gastric and duodenal ulcers associated with taking NSAIDs in patients at risk.
Zollinger-Ellison syndrome and other conditions characterized by abnormal hypersecretion of gastric glands, including idiopathic hypersecretion.
Active ingredient
Active ingredient
Composition
Composition
1 capsule of enteric-soluble 20 mg/40 mg contains:
Pellet core:
Active substance:
Esomeprazole magnesium dihydrate 21.688 mg/43.376 mg (equivalent to esomeprazole magnesium 20.645 mg/41.290 mg, equivalent to esomeprazole 20.000 mg/40.000 mg)
Excipients:sugar grits[sucrose, starch treacle], povidone K30, sodium lauryl sulfate
: justify;”> Pellet shell:
Opadray II White 85F28751*, magnesium hydroxycarbonate (magnesium carbonate heavy), methacrylic acid and ethyl acrylate copolymer [1:1], 30% dispersion**, talc, macrogol-6000, titanium dioxide (E171), polysorbate-80
Gelatin capsule
Composition of empty gelatin capsules:
Capsule shell:
Dye iron oxide red (E172), titanium dioxide (E171), gelatin
Capsule cap:
Dye iron oxide red (E172), titanium dioxide (E171), gelatin
* Opadray II White 85F28751 is a mixture of:
Polyvinyl alcohol, titanium dioxide (E171), macrogol-3000, talc
**The Eudragit L30D dispersion contains sodium lauryl sulfate (0.7% per solid in the dispersion) and polysorbate-80 (2.3% per solid in the dispersion) as emulsifiers in addition to methacrylic acid, ethyl acrylate copolymer and water.
How to take, the dosage
How to take, the dosage
Ingestion. The capsule should be swallowed whole, without chewing, with a small amount of liquid.
For patients with difficulty swallowing, the contents of the capsule can be poured into half a glass of still water (other liquids should not be used because the protective coating of the pellets may dissolve), stirred, and then the pellet suspension should be drunk immediately or within 30 minutes. Then fill the glass half-full with water again, rinse the walls of the glass, stir up the rest and drink. The pellets should not be chewed or crushed.
Patients who cannot swallow on their own should dissolve the contents of the capsules in non-carbonated water and administer esomeprazole through a nasogastric tube. It is important that the syringe and tube chosen are suitable for this procedure. For instructions on preparation and administration of the drug through the nasogastric tube, see “Administration of the drug through the nasogastric tube”.
Adults and children over 12 years of age
Adults and children over 12 years of age
Gastroesophageal reflux disease (GERD)
Treatment of erosive reflux esophagitis: 40 mg once daily for 4 weeks.
An additional 4-week course of treatment is recommended in cases where esophagitis does not heal or symptoms persist after the first course of treatment.
Long-term maintenance treatment after healing of erosive reflux esophagitis to prevent recurrence: 20 mg once daily.
Symptomatic treatment of GERD: 20 mg once daily for patients without esophagitis. If symptoms do not disappear after 4 weeks of treatment, further evaluation of the patient should be performed. After elimination of symptoms it is possible to switch to the mode of the medicine intake “on demand”, i.e. to take Emanera® 20 mg once a day if symptoms recur. For patients taking NSAIDs and who are at risk of developing gastric or duodenal ulcer, “on demand” treatment is not recommended.
Adult patients
Gastric and Duodenal Ulcer
In combination therapy to eradicate Helicobacter pylori
Long-term acid-suppressive therapy in patients who have had bleeding from a peptic ulcer (after intravenous use of drugs that reduce gastric gland secretion to prevent recurrence)
The drug Emanera® 40 mg once daily for 4 weeks after completion of intravenous therapy with gastric gland secretion-lowering drugs.
Patients taking long-term NSAIDs
Conditions associated with abnormal hypersecretion of gastric glands, including Zollinger-Ellison syndrome and idiopathic hypersecretion
The recommended initial dose of Emanera® is 40 mg twice daily. Subsequently, the dose is adjusted individually and the duration of treatment is determined by the clinical picture of the disease. There is an experience of using the drug in doses up to 120 mg twice a day.
Renal insufficiency:Emanera® dose adjustment is not required. However, the experience of using esomeprazole in patients with severe renal insufficiency is limited; therefore, caution should be exercised when prescribing Emanera® to these patients (see section “Pharmacokinetics”).
hepatic failure:in mild to moderate hepatic failure, no dose adjustment of Emanera® is required. For patients with severe hepatic insufficiency, the maximum daily dose should not exceed 20 mg.
Elderly patients: Dose adjustment of Emanera® is not required.
Injection of the drug via nasogastric tube
Injecting the drug through the nasogastric tube
Interaction
Interaction
Effects of esomeprazole on the pharmacokinetics of other drugs
Drugs whose absorption depends on pH
Decreased gastric hydrochloric acid secretion with treatment with esomeprazole and other PPIs can lead to changes in absorption of drugs whose absorption depends on the level of acidity of the environment. Like antacids and other drugs that reduce gastric acidity, use of esomeprazole may reduce absorption of ketoconazole, itraconazole and erlotinib and increase absorption of drugs such as digoxin.
The simultaneous administration of omeprazole at a dose of 20 mg once daily and digoxin increases the bioavailability of digoxin by 10% (the bioavailability of digoxin was increased by up to 30% in two of ten patients).
Interactions of omeprazole with some antiviral drugs are known.The mechanism and clinical significance of these interactions are not always known. A decrease in gastric acidity during therapy with omeprazole may affect absorption of antiviral drugs.An interaction at the level of CYP2C19 isoenzyme is also possible. During therapy with omeprazole a decrease in serum concentrations of some antiviral drugs (atazanavir and nelfinavir) has been noted. Therefore concomitant use is contraindicated. Concomitant use of omeprazole (40 mg once daily) with atazanavir 300 mg/ritonavir .100 mg in healthy volunteers was accompanied by a marked decrease in the bioavailability of atazanavir (AUC, Cmax and minimum plasma concentration [Cmin]decreased by approximately 75%). Increasing the atazanavir dose to 400 mg did not compensate for the effects of omeprazole on the bioavailability of atazanavir.
Simultaneous use of omeprazole with saquinavir increases the serum concentration of saquinavir.
Given the similar pharmacokinetic and pharmacodynamic properties of omeprazole and esomeprazole, simultaneous use of esomeprazole with antiviraldrugs such as atazanavir and nelfinavir is contraindicated.
Drugs metabolized by isoenzyme CYP2.C19
Esomeprazole inhibits the CYP2C19 isoenzyme, the main isoenzyme of esomeprazole metabolism. Thus, co-administration of esomeprazole with drugs metabolized by CYP2C19 isoenzyme, such as diazepam, citalopram, imipramine, clomipramine, phenytoin, etc., may increase the plasma concentration of these drugs and, therefore, their doses should be decreased.
This should especially be considered when prescribing Emanera® on demand. For example, concomitant use with 30 mg of esomeprazole decreases the clearance of diazepam (a substrate of the CYP2C19 isoenzyme) by 45%.
Simultaneous use of esomeprazole in dose of 40 mg leads to increase plasma concentrations of phenytoin in patients with epilepsy by 13%. It is recommended to monitor plasma concentrations of phenytoin at the beginning of therapy with esomeprazole and at its withdrawal.
The use of omeprazole in dose 40 mg increases Cmax and AUCvoriconazole (CYP2C19 isoenzyme substrate) by 15% and 41%, respectively.
Coagulation time with concomitant long-term administration of warfarin and esomeprazole at a dose of 40 mg remains within acceptable limits. However, several cases of clinically significant increases in international normalized ratio (INR) have been reported. It is recommended to monitor INR at the beginning and at the end of concomitant use of esomeprazole and warfarin or other coumarin derivatives.
The use of omeprazole at a dose of 40 mg resulted in an increase in Cmax and AUC cilostazole by 18% and 26%, respectively, for one of the active metabolites cilostazole the increase was 29% and 69%, respectively.
Simultaneous use of esomeprazole at a dose of 40 mg with cisapride leads to increased values of pharmacokinetic parameters of cisapride in healthy volunteers: AUC by 32% and T1/2 by 31%, but Cmax does not change significantly. Slight prolongation of the QT interval on ECG, which is observed with cisapride monotherapy, was not increased with the addition of esomeprazole.
In some patients, increased serum concentrations of methotrexate were noted with concomitant use of PPIs. If high doses of methotrexate are used, temporary withdrawal of esomeprazole should be considered.
Esomeprazole does not cause clinically significant changes in pharmacokinetics of amoxicillin and quinidine.
Simultaneous short-term use of esomeprazole and naproxen or rofecoxib showed no clinically significant pharmacokinetic interaction.
Results obtained in studies with healthy volunteers have demonstrated a pharmacokinetic/pharmacodynamic interaction between clopidogrel (loading dose of 300 mg/maintenance dose of 75 mg daily) and esomeprazole (40 mg daily if ingested) that results in an average 40% reduction in systemic exposure to the active metabolite clopidogrel and an average 14% reduction in maximum suppression (ADP-induced) of platelet aggregation.
The use of clopidogrel alone with a fixed combination of 20 mg esomeprazole/81 mg acetylsalicylic acid (ASA) compared with using clopidogrel alone in a study involving healthy volunteers showed a reduction of nearly 40% in systemic exposure to the active metabolite clopidogrel. However, the maximum levels of suppression (ADP-induced) of platelet aggregation in these healthy volunteers were similar in the clopidogrel and clopidogrel with fixed combination (esomeprazole/ASC) groups.
In both observational and clinical studies, conflicting data have been reported regarding the clinical consequences of the pharmacokinetic/pharmacodynamic interaction of esomeprazole on major cardiovascular events. Concomitant use of clopidogrel should be avoided as a precautionary measure.
Concomitant use with tacrolimus may increase serum concentrations of tacrolimus.
Influence of drugs on the pharmacokinetics of esomeprazole
The effect of drugs on the pharmacokinetics of esomeprazole: justify;”>The CYP2C19 and CYP3A4 isoenzymes are involved in the metabolism of esomeprazole.
Simultaneous use of esomeprazole with clarithromycin (500 mg 2 times daily) (CYP3A4 isoenzyme inhibitor), AUC of esomeprazole is increased by 2 times.
Simultaneous use of esomeprazole and combined inhibitor of CYP2C19 and CYP3A4 isoenzymes (e.g. voriconazole) may be accompanied by more than 2-fold increase in AUC of esomeprazole. No change in the dose of esomeprazole is usually required in such situations. In patients with severe hepatic impairment or if prolonged therapy is necessary, a reduction in the dose of esomeprazole should be considered.
Medicinal products inducing CYP2C19 and CYP3A4 isoenzymes, such as rifampicin and St. John’s Wort preparations, when used concomitantly with esomeprazole may decrease esomeprazole plasma concentration by accelerating esomeprazole metabolism.
Special Instructions
Special Instructions
Severe renal impairment (experience of use is limited).
It is contraindicated in children under 12 years of age (no data on efficacy and safety) and is contraindicated in children over 12 years for indications other than gastroesophageal reflux disease (GERD).
Children over 12 years of age
Gastroesophageal reflux disease (GERD)
Treatment of erosive reflux esophagitis: 40 mg once daily for 4 weeks.
Long-term maintenance treatment after healing of erosive reflux esophagitis to prevent recurrence: 20 mg once daily.
Symptomatic treatment of GERD: 20 mg once daily for patients without esophagitis. Once symptoms have resolved, you can switch to an “on-demand” regimen, i.e., take Emanera® 20 mg once daily when symptoms recur.
Renal failure:Dose adjustment of Emanera® is not required. However, the experience of using esomeprazole in patients with severe renal insufficiency is limited; therefore, caution should be exercised when prescribing Emanera® to these patients (see section “Pharmacokinetics”).
Hepatic failure:In mild to moderate hepatic failure, no dose adjustment of Emanera® is required. For patients with severe hepatic insufficiency, the maximum daily dose should not exceed 20 mg.
Elderly patients:Dose adjustment of Emanera® is not required.
In case of alarming symptoms (such as significant, spontaneous weight loss, recurrent vomiting, dysphagia, vomiting with blood or melena) and when gastric ulcer is suspected or detected, malignancy should be excluded, as use of Emanera® may reduce symptom severity and delay the diagnosis.
Patients taking Emanera® for a long time (especially more than a year) should be under regular medical supervision.
Patients taking the drug “on-demand” should be informed to consult a physician when symptoms change. Taking into account the fluctuations of esomeprazole concentrations in blood plasma when using the drug in the “on demand” mode, interactions with other medicinal products should be considered (see section “Interaction with medicinal products”).
When using esomeprazole to eradicate Helicobacterpylori, possible interaction between the components of triple therapy should be considered. Clarithromycin is a potent CYP3A4 inhibitor, therefore contraindications and drug interactions of clarithromycin should be considered while administering triple therapy to patients who simultaneously take drugs metabolized by CYP3A4 isoenzyme, such as cisapride.
Influence on the results of laboratory tests
An increase in plasma CgA concentration may affect the results of tests conducted to diagnose neuroendocrine tumors. To avoid this effect, treatment with Emanera® should be stopped at least 5 days before determining the plasma CgA concentration (see subsection “Pharmacodynamics” of section “Pharmacological properties”). If CgA and gastrin levels do not return to normal range after initial measurement, a control study should be performed 14 days after discontinuation of PPI treatment.
Hypomagnesemia
Severe cases of severe hypomagnesemia have been reported in patients treated with PPIs, such as esomeprazole, for at least three months and, in most cases, for up to a year. Severe manifestations of hypomagnesemia such as fatigue, tetany, delirium, seizures, dizziness and ventricular arrhythmias may occur, but they may develop gradually and may be overlooked. In patients with the most severe abnormalities, hypomagnesemia decreased after magnesium replacement therapy and PPI withdrawal.
In patients who are scheduled for long-term therapy or who take PPIs concurrently with digoxin or drugs that cause hypomagnesemia (e.g., diuretics), healthcare providers should consider monitoring plasma magnesium before starting PPI treatment and periodically during treatment.
Fractures of the femoral neck, carpal and spinal bones
PPPIs, especially when used in high doses and over a long period of time (more than 1 year), may moderately increase the risk of femoral neck, carpal, and spine fractures, primarily in the elderly or in the presence of other identified risk factors. Observational studies suggest that PPIs may increase the overall risk of fracture by 10-40%. Some of this increase may be due to other risk factors. Patients at risk for osteoporosis should be treated according to current clinical guidelines and should consume adequate amounts of vitamin D and calcium.
Open cutaneous lupus erythematosus (SLE)
PPI use is associated with extremely rare cases of SLE. In case of pathological skin changes, especially in exposed skin areas accompanied by arthralgia, the patient should seek medical attention immediately. The physician should consider discontinuing EmanerÃ. PKCV due to prior PPI therapy may increase the risk of PKCV during subsequent therapy with other PPIs.
Special information on excipients
Emanera® contains sucrose, so its use is contraindicated in patients with hereditary fructose intolerance, glucose-galactose malabsorption syndrome or sucrose-isomaltase deficiency.
When using the drug, caution should be exercised while performing potentially hazardous activities requiring increased concentration and quick psychomotor reactions.
Synopsis
Synopsis
Capsules 20 mg:
Capsules #3. The body and cap of the capsule are light pink in color. The content of the capsule: pellets of white to almost white color.
Capsules 40 mg:
Capsules #1. The capsule body and cap are pink to pink with a faint grayish tint. Capsule contents: pellets of white to almost white color.
Contraindications
Contraindications
Hypersensitivity to esomeprazole, substituted benzimidazoles, or other components of the drug.
Petiatric age less than 12 years (no efficacy or safety data are available) and pediatric age greater than 12 years for indications other than gastroesophageal reflux disease (GERD).
Concurrent administration with atazanavir and nelfinavir (see “Interaction with other drugs”).
Hereditary fructose intolerance, glucose-galactose malabsorption syndrome or sucrose-isomaltase deficiency (Emanera® contains sucrose).
Side effects
Side effects
The following are the dosage-independent side effects of Emanera® noted with esomeprazole, both in clinical trials and in post-marketing studies.
World Health Organization (WHO) recommended side effect frequency classification:
very frequently â¥1/10
often ⥠1/100 to < 1/10
infrequently from ⥠1/1000 to < 1/100
rarely from ⥠1/10000 to < 1/1000
very rarely < 1/10000
frequency is unknown cannot be estimated from available data.
In each group, adverse effects are presented in decreasing order of severity.
Blood and lymphatic system disorders:
rarely: Leukopenia, thrombocytopenia;
very rarely: agranulocytosis, pancytopenia.
immune system disorders:
rare: hypersensitivity reactions (e.g., fever, angioneurotic edema, anaphylactic reaction/anaphylactic shock).
Metabolic and nutritional disorders:
infrequent: peripheral edema;
rarely: hyponatremia;
very rarely: hypomagnesemia, hypocalcemia due to severe hypomagnesemia, hypocalemia due to hypomagnesemia.
Mental disorders:
infrequently:insomnia;
rarely: depression, agitation, confusion;
very rare: hallucinations, aggressive behavior.
Nervous system disorders:
often: headache;
Overdose
Overdose
To date, extremely rare cases of intentional overdose of esomeprazole have been described. An oral dose of 280 mg of esomeprazole was accompanied by general weakness and gastrointestinal symptoms. A single dose of 80 mg of esomeprazole caused no adverse effects. The antidote for esomeprazole is not known. Esomeprazole binds well to plasma proteins, so dialysis is ineffective. In case of overdose, symptomatic and general supportive treatment is necessary.
Pregnancy use
Pregnancy use
There are insufficient data on the use of esomeprazole in pregnant women.
No fetotoxic effects or fetal development disorders were found in epidemiological studies during the use of racemic omeprazole mixture.
In studies with esomeprazole in animals, no direct or indirect adverse effects on embryonic or fetal development have been identified, and no direct or indirect adverse effects on pregnancy, labor, and postnatal development of the newborn have been identified. The drug should be administered to pregnant women only when the expected benefits to the mother outweigh the possible risk to the fetus.
It is currently unknown whether esomeprazole is excreted with the breast milk, so Emanera® should not be used during breastfeeding.
Similarities
Similarities
Additional information
| Weight | 0.019 kg |
|---|---|
| Shelf life | 2 years. Do not use the product after the expiration date. |
| Conditions of storage | At temperature not exceeding 25ºC, in original packaging. Store out of reach of children. |
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | capsules |
| Brand | KRKA dd Novo mesto |
Other forms…
Related products
Buy Emanera, 20 mg capsules 14 pcs with delivery to USA, UK, Europe and over 120 other countries.