Subtotal: €17.68
Egolanza, 5 mg 28 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Schizophrenia, Anxiety, Manic Depressive Psychosis
Schizophrenia (exacerbation, maintenance and long-term antiretroviral therapy). Bipolar affective disorder (monotherapy or in combination with Li+ drugs or valproic acid): acute manic or mixed episodes with/without psychotic manifestations and with/without rapid phase change.
Bipolar relapse and prevention of bipolar relapse (if the drug is effective in treating the manic phase).
Indications
Schizophrenia (exacerbation, maintenance and long-term anti-relapse therapy). Bipolar affective disorder (monotherapy or in combination with Li+ or valytroic acid): acute manic or mixed episodes with/without psychotic manifestations and with/without rapid phase changes.
Relapse of bipolar disorder and prevention of relapse of bipolar disorder (if the drug is effective in treating the manic phase).
Pharmacological effect
Egolanza – antipsychotic drug (neuroleptic)
Special instructions
While taking antipsychotic medications, patients’ clinical condition may improve within days or weeks. During this period, patients need careful monitoring.
Psychosis and/or behavioral disorders associated with dementia
Olanzapine is not approved for use in the treatment of psychosis and/or behavioral disturbances associated with dementia, and this drug is not recommended for use in these patients due to increased mortality and risk of cerebrovascular accidents. Cerebrovascular events (stroke, transient ischemic attack), including deaths, have been reported when taking olanzapine in elderly patients with psychosis due to dementia. These patients had previous risk factors (cerebrovascular disorders (history), transient ischemic attacks, arterial hypertension, smoking), as well as concomitant diseases and/or drug intake that were temporally associated with cerebrovascular disorders.
Olanzapine is not recommended for the treatment of dopamine agonist-associated psychosis in patients with Parkinson’s disease.
Neuroleptic malignant syndrome (NMS)
When treated with neuroleptics (including olanzapine), neuroleptic malignant syndrome may develop. Clinical manifestations of NMS are fever, muscle rigidity, changes in mental state, instability of autonomic functions (unstable levels of heart rate and blood pressure, tachycardia, sweating, cardiac arrhythmia). Additional signs may include elevated creatine phosphokinase levels, myoglobinuria (rhabdomyolysis), and acute renal failure. If a patient develops symptoms and signs of NMS or develops an unexplained fever without additional clinical manifestations of NMS, all antipsychotics, including olanzapine, should be discontinued.
Hyperglycemia and diabetes mellitus
There is a higher prevalence of diabetes mellitus in patients with schizophrenia. Very rarely, cases of hyperglycemia, development of diabetes mellitus or exacerbation of pre-existing diabetes mellitus, ketoacidosis and diabetic coma have been reported. The causal relationship between antipsychotic drugs and these conditions has not been established. Clinical monitoring of patients with diabetes mellitus or with risk factors for its development is recommended.
Changes in lipid levels
If lipid levels change while taking olanzapine, appropriate treatment should be prescribed, especially in patients with dyslipidemia or risk factors for developing lipid metabolic disorders.
Anticholinergic activity
Although olanzapine has anticholinergic activity in vitro, due to limited clinical experience with olanzapine in patients with underlying medical conditions, caution is advised when prescribing this drug to patients with prostatic hypertrophy, paralytic ileus and other similar conditions.
Liver function
Particular caution is required when the activity of liver transaminases, ALT and/or AST is increased in patients with liver failure or receiving treatment with potentially hepatotoxic drugs. Monitoring the patient and, if necessary, reducing the dose is required. If hepatitis (including hepatocellular, cholestatic or mixed liver damage) is detected, olanzapine should be discontinued.
Neutropenia
Olanzapine should be used with caution in patients with a decrease in the number of white blood cells, including neutrophils; with signs of depression or toxic impairment of bone marrow function under the influence of drugs (history); with suppression of bone marrow function due to concomitant disease, radiotherapy or chemotherapy (history); with hypereosinophilia or myeloproliferative disease. Neutropenia is often observed with the combined use of olanzapine and valproate. The use of olanzapine in patients with clozapine-dependent neutroenia or agranulocytosis (history) was not accompanied by relapses of these disorders.
Stopping the drug
In very rare cases, if you suddenly stop taking olanzapine (
Interval FROM
As with other antipsychotics, caution should be used during treatment with olanzapine if this drug is coadministered with drugs that prolong the QTc interval, especially in elderly patients, patients with congenital long QT syndrome, congestive heart failure, cardiac hypertrophy, hypokalemia, hypomagnesemia, or a family history of QT prolongation.
Concomitant use of other antipsychotics or drugs that also prolong the QT interval or cause hypokalemia should be avoided.
Thromboembolism
Coincidence in the timing of olanzapine administration and venous thromboembolism has been reported in rare cases (less than 0.01%). The causal relationship between the symptoms of venous thromboembolism and the use of olanzapine has not been established. However, since patients with schizophrenia often have acquired risk factors for venous thromboembolism, all possible risk factors for venous thromboembolism, such as patient immobility, should be identified and preventive measures taken.
Seizures
Olanzapine should be used with caution in patients with a history of seizures or exposure to factors that lower the seizure threshold. Seizures are rare in patients receiving olanzapine. Most of these cases have a history of seizures or risk factors for seizures.
Tardive dyskinesia
If signs of tardive dyskinesia develop, it is recommended to reduce the dose or discontinue olanzapine. Symptoms of tardive dyskinesia may increase or manifest after discontinuation of the drug.
Orthpostatic hypotension
In clinical trials of olanzapine, orthostatic hypotension was observed infrequently in elderly patients. As with other antipsychotic drugs, it is recommended that blood pressure be measured periodically in patients over 65 years of age.
Use in pediatrics
Olanzapine is not recommended for use in children and adolescents. Studies conducted in patients aged 13-17 years have revealed a variety of adverse reactions, including weight gain, changes in metabolic parameters and increased prolactin levels. The long-term outcomes of these events have not been studied and remain unknown.
Lactose
This medicine contains lactose and should not be used in patients with rare hereditary galactose intolerance disorders, hereditary Sami lactase deficiency or glucose-galactose malabsorption. Caution should be exercised when using olanzapine in combination with other centrally acting drugs and ethanol.
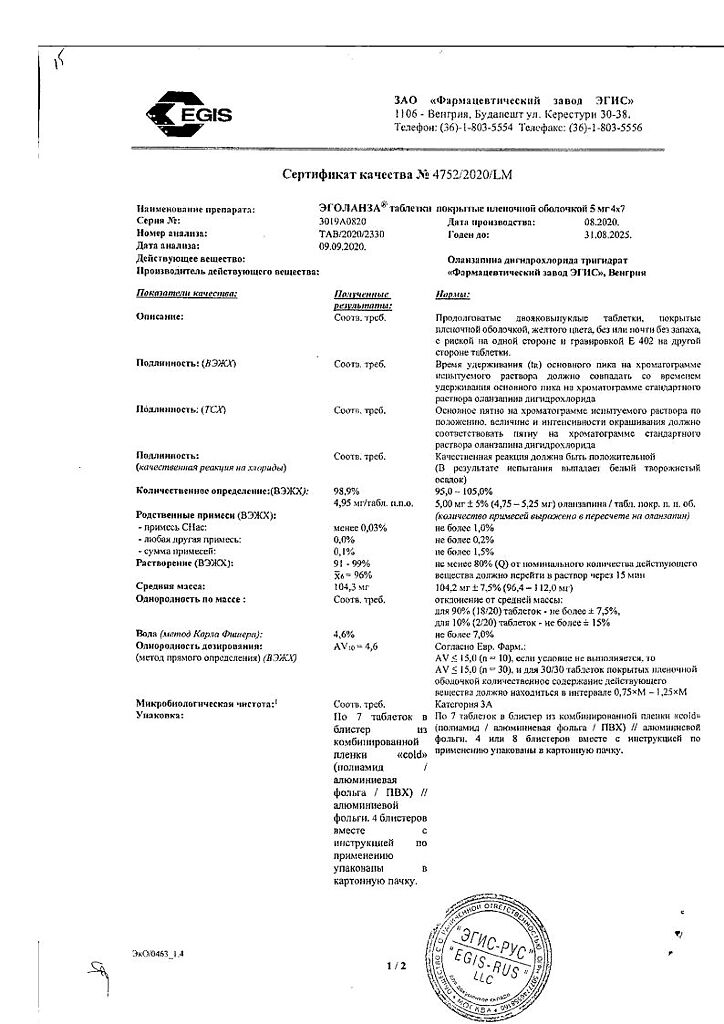
Active ingredient
Olanzapine
Composition
1 tablet contains:
Contraindications
Hypersensitivity to the active substance or any of the components of the drug. Angle-closure glaucoma. Psychoses and/or behavioral disorders associated with dementia. Lactation period. Children’s age (up to 18 years due to insufficient clinical data). Lactose intolerance, lactase deficiency or glucose-galactose malabsorption (the drug contains lactose).
With caution
Liver failure, renal failure, prostatic hyperplasia, epilepsy, history of convulsive syndrome, myelosuppression (including leukopenia, neutropenia). myeloproliferative diseases, hypereosinophilic syndrome, paralytic ileus, pregnancy, cardiovascular or cerebrovascular disease or other conditions predisposing to hypotension, congenital prolongation of the QT interval on the electrocardiogram (ECG) (increase in the corrected QT interval (QTc) on the ECG), or when there are any conditions that can potentially cause prolongation of the QT interval (for example, simultaneous administration of drugs that prolong the QT interval, congestive heart failure, hypokalemia, hypomagnesemia), advanced age, as well as simultaneous use of other centrally acting drugs; immobilization.
Side Effects
From the nervous system and sensory organs: dizziness, headache, migraine, weakness, asthenia, drowsiness, insomnia, anxiety, hostility, agitation, euphoria, amnesia, depersonalization, phobia, obsessive-compulsive symptoms, neuralgia, facial nerve paresis, hypoesthesia, extrapyramidal disorders, incl. tardive dyskinesia, ataxia, stiff neck, muscle twitching, tremor, akathisia, dysarthria, stuttering, syncope, delirium, suicidal tendencies, stupor, coma, subarachnoid hemorrhage, stroke, nystagmus, diplopia, mydriasis, pigment deposition in the lens, cataract, xerophthalmia, hemorrhages in the eye, accommodation disturbance, amblyopia, glaucoma, corneal damage, eye pain, keratoconjunctivitis, blepharitis, noise and pain in the ears, deafness, impaired taste.
From the cardiovascular system and blood (hematopoiesis, hemostasis): orthostatic hypotension, tachy- and bradycardia, palpitations, ventricular extrasystole, ECG changes, cardiac arrest, cyanosis, vasodilation, transient leuko- and neutropenia, eosinophilia, leukocytosis, thrombocytopenia, hemorrhagic syndrome.
From the respiratory system: rhinitis, pharyngitis, laryngitis, change in voice, increased cough, dyspnea, apnea, bronchial asthma, hyperventilation.
From the gastrointestinal tract: increased appetite up to bulimia, thirst, dry mouth, increased salivation, aphthous stomatitis, gingivitis, glossitis, dysphagia, belching, esophagitis, nausea, vomiting, gastritis, gastroenteritis, enteritis, melena, rectal bleeding, constipation, flatulence, fecal incontinence, transient increase in liver activity transaminases, gamma-glutamyl transpeptidase and creatine phosphokinase, hepatitis.
From the metabolic side: hyperprolactinemia, increase (rarely decrease) in body weight, diabetes mellitus, hyperglycemia, diabetic ketoacidosis, diabetic coma, goiter.
From the genitourinary system: dysuria (including polyuria), hematuria, pyuria, albuminuria, urinary incontinence, urinary tract infections, cystitis, decreased libido, impotence, ejaculation disorders, priapism, gynecomastia, galactorrhea, pain in the mammary glands, uterine fibrosis, premenstrual syndrome, meno- and metrorrhagia, amenorrhea.
From the musculoskeletal system: arthritis, arthralgia, bursitis, myasthenia gravis, myopathy, calf muscle cramps, bone pain.
From the skin: photosensitivity, alopecia, hirsutism, dry skin, eczema, seborrhea, contact dermatitis, ulcerative skin lesions, skin discoloration, maculopapular rash.
Allergic reactions: urticaria.
Other: fever, chills, flu-like syndrome, lymphadenopathy, chest or abdominal pain, peripheral edema, withdrawal syndrome, abuse possible.
Interaction
Inducers or inhibitors of the CYP1A2 isoenzyme may alter the metabolism of olanzapine. Inducers of the CYP1A2 isoenzyme: the clearance of olanzapine increases in smoking patients and with simultaneous use of carbamazepine, which leads to a decrease in the concentration of olanzapine in the blood plasma. It may be necessary to increase the dose of the drug. CYP1A2 isoenzyme inhibitors: fluvoxamine significantly inhibits the metabolism of olanzapine. By reducing the clearance of olanzapine, it increases Olanzapine C in non-smoking women by 54% and by 77% in smoking men, AUC by 52% and 108%, respectively, therefore, in patients taking fluvoxamine or any other inhibitor of the CYP1A2 isoenzyme (for example, ciprofloxacin), the use of a lower initial dose of olanzapine should be considered.
Activated charcoal reduces the bioavailability of olanzapine by 50-60% and should be taken at least 2 hours before or 2 hours after olanzapine.
Fluoxetine (a CYP2D6 inhibitor), as well as a single dose of antacids (aluminum or magnesium) or cimetidine, did not have a significant effect on the pharmacokinetics of olanzapine.
Ethanol did not affect the pharmacokinetics of olanzapine at steady state, however, taking ethanol together with olanzapine may be accompanied by an increase in the pharmacological effects of olanzapine (sedation).
Olanzanine slightly inhibits the formation of valproic acid glucuronide (the main metabolic pathway). Valproic acid has little effect on the metabolism of olanzapine. A clinically significant pharmacokinetic interaction between olanzapine and valproic acid is unlikely.
Caution is required when using olanzapine with drugs that prolong the QTc interval (amitriptyline, chlorpromazine, droperidol, thioridazine, pimozide, quinidine, procainamide, sotalol, ephedrine, epinephrine, terbutaline, erythromycin, trimethoprim/sulfamethoxazole, ketoconazole, fluconazole, etc.), disrupting the electrolyte balance or inhibiting the metabolism of olanzapine in the liver.
Concomitant use of olanzapine and antiparkinsonian drugs in patients with Parkinson’s disease and dementia is not recommended.
Olanzapine exhibits dopamine antagonism and, theoretically, may inhibit the effects of levodopa and dopamine agonists.
Olanzapine does not inhibit the main CYP450 isoenzymes in vitro (for example, 1A2, 2D6, 2C9, 2C19, 3A4); a clinically significant interaction is unlikely. No inhibition of the metabolism of the following active substances was found: tricyclic antidepressants (representing mainly the CYP2D6 pathway), warfarin (CYP2C9), theophylline (CYP1A2) or diazepam (CYP3A4 and 2C19).
No interaction was detected when used simultaneously with lithium or biperiden.
Overdose
Symptoms: tachycardia, agitation/aggression, articulation disorder, extrapyramidal disorders, depression of consciousness of varying severity (from sedation to coma), delirium, convulsions, neuroleptic malignant syndrome, respiratory depression, aspiration, increased or decreased blood pressure, arrhythmias, cardiac and respiratory arrest. The minimum dose for acute overdose with fatal outcome was 450 mg, the maximum dose with a favorable outcome (survival) was 1500 mg.
Treatment: gastric lavage, administration of activated carbon, symptomatic treatment, maintaining respiratory function. You should not use sympathomimetics (including norepinephrine, dopamine), which are beta-adrenergic receptor agonists (stimulation of these receptors can aggravate the decrease in blood pressure). Close medical observation and monitoring should continue until the patient recovers.
Storage conditions
Store at a temperature not exceeding 30 °C. Keep the drug out of the reach of children!
Shelf life
3 years
Manufacturer
EGIS, Hungary
| Shelf life | 3 years |
|---|---|
| Conditions of storage | Store at the temperature not more than 30 °С. Keep the drug out of reach of children! |
| Manufacturer | EGIS, Hungary |
| Medication form | pills |
| Brand | EGIS |
Related products
Buy Egolanza, 5 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.