No products in the cart.
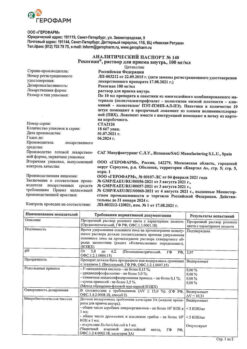
Edarbi Clo, 40 mg+25 mg 28 pcs
€32.64 €29.94
Description
Edarbi® Clo is a combination drug consisting of an angiotensin II receptor antagonist (ARAII – azilsartan medoxomil) and a thiazide-like diuretic (chlorthalidone). Simultaneous use of the two active agents leads to a more pronounced BP reduction compared to that of each of them in monotherapy. When administered once daily, effective BP lowering is achieved within 24 hours.
Asilsartan medoxomil, one of the active ingredients in Edarbi® Clo, is a specific angiotensin II type 1 receptor antagonist (AT1). Angiotensin II is formed from angiotensin I in a reaction catalyzed by ACE (kininase II). Angiotensin II is the major vasoconstrictor of the RAAS and its effects include vasoconstriction, stimulation of aldosterone synthesis and secretion, increased HR, and renal sodium reabsorption. Azilsartan medoxomil is an oral prodrug. Azilsartan medoxomil is rapidly converted to the active molecule azilsartan, which selectively inhibits the effects of angiotensin II by blocking its binding to AT1 receptors in various tissues such as vascular smooth muscle and the adrenal gland. Therefore, its action is not related to the pathway of angiotensin II biosynthesis.
The AT2 receptor is also found in many tissues, but it is not involved in the regulation of CPS activity. The affinity of azilsartan for the AT1 receptor is 10,000 times greater than for the AT2 receptor.
The inhibition of RAAS activity by ACE inhibitors that inhibit the formation of angiotensin II from angiotensin I is widely used in the treatment of arterial hypertension. ACE inhibitors also inhibit the breakdown of bradykinin, which is catalyzed by ACE. Since azilsartan does not inhibit ACE (kininase II), it should not affect bradykinin activity. Azilsartan does not bind to or block other receptors or ion channels that play an important role in cardiovascular regulation.
Asilsartan dose-dependently suppresses the vasoconstrictor effects of angiotensin II infusion. A single administration of azilsartan at a dose equivalent to 32 mg of azilsartan medoxomil suppressed the maximal vasoconstrictor effects of angiotensin II by approximately 90% at the time of highest concentration, and by approximately 60% 24 h after administration. In healthy volunteers, plasma angiotensin I and angiotensin II concentrations and renin activity increased and aldosterone concentrations decreased after a single oral dose and after repeated doses of azilsartan medoxomil; no clinically significant effect on serum potassium or sodium was found. Overall, the pharmacodynamic properties of azilsartan medoxomil are consistent with blocking the AT1 receptor.
The antihypertensive effect of azilsartan medoxomil develops during the first 2 weeks of use with reaching maximum therapeutic effect after 4 weeks. Decrease of BP after a single oral dose is usually achieved within several hours and maintained for 24 hours.
Chlorthalidone, a thiazide-like diuretic, inhibits active sodium ion reabsorption in the renal tubules (the initial part of the distal convoluted tubule of the nephron), increasing excretion of sodium and chlorine ions and increasing diuresis. In addition, chlorthalidone increases excretion of potassium, magnesium and bicarbonate ions and inhibits calcium ions and uric acid. The antihypertensive effect of chlorthalidone is associated with the elimination of fluid and sodium from the body. Diuretic effect develops 2-3 hours after oral administration of chlorthalidone and lasts for 2-3 days.
The antihypertensive effect of chlortalidone develops gradually, with maximum therapeutic effect 2-4 weeks after initiation of therapy.
In the clinical studies, the combination of azilsartan medoxomil + chlorthalidone was more effective than the combination of azilsartan medoxomil with hydrochlorothiazide or the combination olmesartan medoxomil + hydrochlorothiazide, even though a higher proportion of study participants in the comparison group required dose increases due to insufficient BP control.
In a 12-week double-blind, planned dose escalation study, the 40 + 25-mg combination of azilsartan medoxomil + chlorthalidone was statistically significantly superior to the 40 + 25-mg combination of olmesartan medoxomil + hydrochlorothiazide in reducing BP in moderate to severe arterial hypertension.
Similar results were obtained in all patient subgroups, regardless of age, sex, or race. The combination of azilsartan medoxomil + chlorthalidone lowered BP more effectively than the combination of olmesartan medoxomil + hydrochlorothiazide in each hour of the 24-hour interval between doses of the drugs, as measured by CMAD (daily blood pressure monitoring).
Indications
Indications
Essential hypertension (patients for whom combination therapy is indicated).
Pharmacological effect
Pharmacological effect
Edarbi® Clo is a combination drug that contains an angiotensin II receptor antagonist (ARAII – azilsartan medoxomil) and a thiazide-like diuretic (chlorthalidone). The simultaneous use of two active substances leads to a more pronounced decrease in blood pressure compared to that when taking each of them in monotherapy. When taking the drug once a day, an effective reduction in blood pressure is achieved within 24 hours.
Azilsartan medoxomil, one of the active ingredients of the drug Edarbi® Clo, is a specific antagonist of angiotensin II type 1 receptors (AT1). Angiotensin II is formed from angiotensin I in a reaction catalyzed by ACE (kininase II). Angiotensin II is the main vasoconstrictor factor of the RAAS; its actions include vasoconstriction, stimulation of aldosterone synthesis and secretion, increased heart rate and renal sodium reabsorption. Azilsartan medoxomil is an oral prodrug. Azilsartan medoxomil is rapidly converted to the active molecule azilsartan, which selectively inhibits the effects of angiotensin II by blocking its binding to AT1 receptors in various tissues, such as vascular smooth muscle and the adrenal glands. Therefore, its action is not related to the angiotensin II biosynthetic pathway.
The AT2 receptor is also found in many tissues, but it is not involved in the regulation of CVS activity. The affinity of azilsartan for the AT1 receptor is 10,000 times higher than for the AT2 receptor.
Inhibition of RAAS activity through ACE inhibitors, which suppress the formation of angiotensin II from angiotensin I, is widely used in the treatment of arterial hypertension. ACE inhibitors also suppress the breakdown of bradykinin, which is catalyzed by ACE. Since azilsartan does not inhibit ACE (kininase II), it should not affect the activity of bradykinin. Azilsartan does not bind to or block other receptors or ion channels that play an important role in the regulation of cardiovascular system.
Azilsartan dose-dependently suppresses the vasoconstrictor effects of angiotensin II infusion. A single dose of azilsartan at a dose equivalent to 32 mg of azilsartan medoxomil suppressed the maximum vasoconstrictor effect of angiotensin II by approximately 90% at the time of highest concentration, and by approximately 60% 24 hours after administration. In healthy volunteers, plasma concentrations of angiotensin I and angiotensin II and renin activity increased, and aldosterone concentrations decreased after a single oral dose and after repeated doses of azilsartan medoxomil; no clinically significant effect on serum potassium or sodium levels was detected. In general, the pharmacodynamic properties of azilsartan medoxomil are consistent with blocking the AT1 receptor.
The antihypertensive effect of azilsartan medoxomil develops during the first 2 weeks of use, achieving the maximum therapeutic effect after 4 weeks. A reduction in blood pressure after oral administration of a single dose is usually achieved within a few hours and persists for 24 hours.
Chlorthalidone, a thiazide-like diuretic, inhibits the active reabsorption of sodium ions in the renal tubules (the initial part of the distal convoluted tubule of the nephron), increasing the excretion of sodium and chloride ions and increasing diuresis. In addition, chlorthalidone increases the excretion of potassium, magnesium and bicarbonate ions, and retains calcium ions and uric acid. The antihypertensive effect of chlorthalidone is associated with the removal of fluid and sodium from the body. The diuretic effect develops 2–3 hours after taking chlorthalidone orally and persists for 2–3 days.
The antihypertensive effect of chlorthalidone develops gradually, with the maximum therapeutic effect achieved 2–4 weeks after the start of therapy.
In clinical trials, the combination of azilsartan medoxomil + chlorthalidone was more effective than the combination of azilsartan medoxomil with hydrochlorothiazide or the combination of olmesartan medoxomil + hydrochlorothiazide, although a higher proportion of study participants in the comparison group required an increase in dose due to insufficient blood pressure control.
In a double-blind, planned dose-escalation study of 12 weeks duration, the combination of azilsartan medoxomil + chlorthalidone 40 + 25 mg was statistically significantly superior to the combination of olmesartan medoxomil + hydrochlorothiazide 40 + 25 mg in reducing SBP in moderate to severe hypertension.
Similar results were obtained in all patient subgroups, regardless of age, gender or race. The combination of azilsartan medoxomil + chlorthalidone lowered blood pressure more effectively than the combination of olmesartan medoxomil + hydrochlorothiazide in each hour of the 24-hour interval between doses of drugs, according to ABPM (24-hour blood pressure monitoring).
Special instructions
Special instructions
Arterial hypotension due to water and electrolyte imbalance
In patients with reduced blood volume and/or hyponatremia (as a result of vomiting, diarrhea, taking large doses of diuretics, or following a diet with limited sodium intake), clinically significant arterial hypotension may develop after starting therapy with Edarbi® Clo. Hypovolemia and water-electrolyte balance should be corrected before starting treatment. Transient arterial hypotension is not a contraindication to further treatment, which can be continued after stabilization of blood pressure.
Renal dysfunction
In patients with impaired renal function (creatinine clearance more than 30 ml/min), the drug should be used with caution. It is recommended to regularly monitor potassium levels and serum creatinine concentrations. Such patients require careful dose selection with constant monitoring and blood pressure control. An increase in creatinine concentration is more often observed in patients with moderate to severe renal impairment.
Chlorthalidone may cause azotemia.
In case of progressive deterioration of renal function (increased blood urea nitrogen), temporary cessation of diuretic therapy or their complete abolition is recommended.
Double blockade of the RAAS
In patients whose vascular tone and renal function depend to a large extent on the activity of the RAAS (for example, patients with severe CHF – functional class IV according to the NYHA classification, severe renal failure or renal artery stenosis), treatment with drugs acting on the RAAS, such as ACE inhibitors and ARAII, is associated with the possibility of developing acute arterial hypotension, azotemia, oliguria, or rarely, acute renal failure. The possibility of developing the listed effects cannot be excluded when using the drug Edarbi® Clo.
A sharp decrease in blood pressure in patients with ischemic cardiomyopathy or ischemic cerebrovascular diseases can lead to the development of myocardial infarction or stroke.
Kidney transplant
There are no data on the use of Edarbi® Clo in patients who have recently undergone kidney transplantation.
Liver dysfunction
There are no data on clinical experience with the use of Edarbi® Clo in patients with severe liver dysfunction, therefore the use of the drug in this category of patients is not recommended (see “Contraindications”). Due to limited experience, Edarbi® Clo should be used with caution in patients with mild to moderate liver dysfunction (less than 9 points on the Child-Pugh scale), since even minor disturbances in water and electrolyte balance when taking diuretics can provoke hepatic coma. It is recommended to actively monitor the condition of such patients.
Primary hyperaldosteronism
Patients with primary hyperaldosteronism are usually resistant to treatment with antihypertensive drugs that affect the RAAS. In this regard, Edarbi® Clo is not recommended for use in such patients.
Hypokalemia
Hypokalemia may develop during therapy with chlorthalidone. It is necessary to regularly monitor potassium levels in the blood serum. In patients taking cardiac glycosides, hypokalemia may predispose to arrhythmia.
Aortic or mitral valve stenosis, HOCM
When prescribing Edarbi® Clo to patients with aortic or mitral stenosis or HOCM, caution should be exercised.
Lithium
As with other ARAIIs, simultaneous use of lithium and Edarbi® Clo is not recommended.
Impact on the ability to drive vehicles and operate machinery. Care must be taken when driving vehicles and working with mechanisms that require increased attention and speed of reaction – there is a risk of developing dizziness and increased fatigue.
Active ingredient
Active ingredient
Azilsartan medoxomil, Chlorthalidone
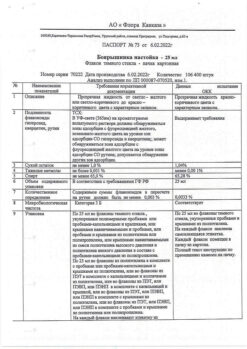
Composition
Composition
1 tab. contains:
Contraindications
Contraindications
hypersensitivity to active substances and other components of the drug;
refractory hypokalemia;
anuria;
simultaneous use of aliskiren and aliskiren-containing drugs in patients with diabetes mellitus or moderate or severe renal impairment (glomerular filtration rate less than 60 ml/min/1.73 m2);
severe forms of diabetes mellitus;
severe liver dysfunction (more than 9 points on the Child-Pugh scale) (no experience with use);
severe renal failure (creatinine Cl less than 30 ml/min) (no experience with use);
pregnancy and breastfeeding (see “Use during pregnancy and breastfeeding);
age under 18 years (efficacy and safety have not been established).
With caution: severe chronic heart failure (functional class IV according to the NYHA classification); impaired renal function (creatinine Cl more than 30 ml/min); mild to moderate liver dysfunction (5–9 points on the Child-Pugh scale); bilateral renal artery stenosis and stenosis of the artery of the only functioning kidney; ischemic cardiomyopathy; ischemic cerebrovascular diseases; condition after kidney transplantation; conditions accompanied by a decrease in blood volume (including vomiting, diarrhea, taking high doses of diuretics), as well as a diet with limited salt; primary hyperaldosteronism; hyperuricemia and gout; bronchial asthma; systemic lupus erythematosus; stenosis of the aortic and mitral valve; hypertrophic obstructive cardiomyopathy (HOCM); age over 75 years; hypokalemia. If the patient has one of the listed diseases, you should consult your doctor before taking Edarbi® Clo.
Side Effects
Side Effects
Combination of azilsartan medoxomil and chlorthalidone
From the blood and lymphatic system: infrequently – anemia.
From the nervous system: often – dizziness, postural dizziness; infrequently – fainting (syncope), paresthesia.
From the side of blood vessels: often – a pronounced decrease in blood pressure.
From the gastrointestinal tract: often – diarrhea, nausea; infrequently – vomiting.
From the skin and subcutaneous tissues: infrequently – skin rash, itching; rarely – angioedema.
From the musculoskeletal and connective tissue side: infrequently – muscle spasms.
Metabolism and nutrition: often – hyperuricemia; uncommon – hypokalemia, increased potassium levels, hyponatremia, exacerbation of gout.
Impact on the results of laboratory and instrumental studies: very often – increased creatinine concentration; often – increased urea concentration; infrequently – increased glucose concentration.
General disorders: often – increased fatigue, peripheral edema.
Azilsartan medoxomil (monotherapy)
From the nervous system: often – dizziness; infrequently – headache.
From the side of blood vessels: infrequently – a pronounced decrease in blood pressure.
From the gastrointestinal tract: often – diarrhea; infrequently – nausea.
From the skin and subcutaneous tissues: infrequently – skin rash, itching; rarely – angioedema.
From the musculoskeletal and connective tissue side: infrequently – muscle spasms.
Impact on the results of laboratory and instrumental studies: often – increased CPK activity; uncommon – increased creatinine concentration, hyperuricemia.
General disorders: infrequently – increased fatigue, peripheral edema.
Chlorthalidone (monotherapy)
From the nervous system: rarely – headache.
From the heart: rarely – arrhythmia.
From the side of blood vessels: often – a pronounced decrease in blood pressure.
From the digestive system: often – loss of appetite, gastrointestinal disorders; rarely – constipation, abdominal pain; very rarely – pancreatitis.
From the skin and subcutaneous tissues: often – urticaria; rarely – photosensitivity, cutaneous vasculitis.
From the respiratory system, chest and mediastinal organs: rarely – allergic pulmonary edema.
From the liver and biliary tract: rarely – intrahepatic cholestasis or jaundice.
From the kidneys and urinary tract: rarely – allergic interstitial nephritis.
From the blood and lymphatic system: rarely – thrombocytopenia, leukopenia, agranulocytosis, eosinophilia.
From the side of metabolism and nutrition: very often – hyperlipidemia, hypokalemia; often – hypomagnesemia; rarely – hypercalcemia, glycosuria, decompensation of existing diabetes mellitus; very rarely – hypochloremic alkalosis.
General disorders: often – decreased potency.
Description of selected adverse reactions
With simultaneous use of azilsartan medoxomil with chlorthalidone, the frequency of adverse reactions – a pronounced decrease in blood pressure and an increase in creatinine concentration – increases in frequency: from infrequently to often. This is due to a more effective reduction in blood pressure compared to monotherapy with azilsartan medoxomil. Most of these effects were short-lived or did not progress as long as patients continued therapy. After discontinuation of the drug, most cases of increase in creatinine concentration that did not go away during treatment were reversible.
The increase in uric acid concentration when using the drug Edarbi® Clo is due to the chlorthalidone included in its composition and depends on the dose of the diuretic. Reports of the development of gout were infrequent even with long-term therapy.
With simultaneous use of azilsartan medoxomil with chlorthalidone, the incidence of adverse reactions such as hypokalemia is reduced.
If any of the side effects indicated in the instructions get worse or the patient notices any other side effects not listed in the instructions, you should inform your doctor.
Interaction
Interaction
Lithium. A reversible increase in serum lithium concentration and toxicity was observed during the simultaneous use of lithium preparations and diuretics and lithium preparations with ARAII. Therefore, the simultaneous use of Edarbi® Clo in combination with lithium preparations is not recommended (see “Special Instructions”). If it is necessary to use appropriate combination therapy, regular monitoring of lithium concentrations in the blood serum is recommended.
NSAIDs, including selective COX-2 inhibitors. In elderly patients and patients with reduced blood volume (including those receiving diuretics) or with impaired renal function, the simultaneous use of ARA II and NSAIDs can lead to a deterioration in renal function, including the development of acute renal failure. Therefore, at the beginning of treatment, patients are advised to regularly take sufficient fluids and monitor kidney function. With the simultaneous use of APAII and NSAIDs, including selective COX-2 inhibitors, acetylsalicylic acid (more than 3 g/day) and non-selective NSAIDs, the antihypertensive effect may be weakened.
Double blockade of the RAAS. Dual blockade of the RAAS by APAII, ACE inhibitors, or aliskiren is associated with an increased risk of arterial hypotension, hyperkalemia, and renal dysfunction (including acute renal failure) compared with monotherapy.
Cardiac glycosides. Concomitant use of cardiac glycosides and a diuretic may worsen the effects of hypokalemia, such as cardiac arrhythmias.
Additional interaction information for azilsartan medoxomil
No PCF was observed with simultaneous use of azilsartan medoxomil or azilsartan with amlodipine, antacids (aluminum and magnesium hydroxide), chlorthalidone, digoxin, fluconazole, glibenclamide, ketoconazole, metformin and warfarin.
Azilsartan medoxomil is converted into the pharmacologically active metabolite azilsartan during absorption from the gastrointestinal tract under the action of the enzyme carboxymethylenebutenolidase in the intestine and liver. In vitro studies have shown that interactions based on enzyme inhibition are unlikely.
Additional information on chlorthalidone interactions
Chlorthalidone enhances the effect of curare-like muscle relaxants and antihypertensive drugs (including guanethidine, methyldopa, beta-blockers, vasodilators, CCBs), MAO inhibitors.
Concomitant use of chlorthalidone with allopurinol may lead to an increased incidence of hypersensitivity reactions to allopurinol.
Chlorthalidone may increase the risk of adverse reactions due to amantadine.
Anticholinergic drugs (eg atropine, biperiden) may increase the bioavailability of chlorthalidone, reducing gastrointestinal motility and gastric emptying.
The hypokalemic effect of chlorthalidone is enhanced by simultaneous use with corticosteroids, ACTH, amphotericin, beta2-blockers, carbenoxolone. Patients should monitor serum potassium levels during combination therapy.
It may be necessary to adjust (decrease or increase) the dose of oral hypoglycemic agents and insulin.
The pharmacological effects of calcium salts and vitamin D may be increased to clinically significant levels when used concomitantly with chlorthalidone.
Concomitant use with cyclosporine may increase the risk of developing hyperuricemia and complications such as gout.
Cholestyramine interferes with the absorption of chlorthalidone. The pharmacological effect of chlorthalidone may be reduced.
The simultaneous use of chlorthalidone with methotrexate and cyclophosphamide can lead to potentiation of the pharmacological effect of anticancer drugs.
Overdose
Overdose
Azilsartan medoxomil (monotherapy)
Experience with the use of azilsartan medoxomil in adults in doses up to 320 mg/day for 7 days shows that the drug is well tolerated.
Symptoms: marked decrease in blood pressure, dizziness.
Treatment: with a pronounced decrease in blood pressure, place the patient in a lying position, raise his legs, and take measures to increase the blood volume; symptomatic therapy. Azilsartan is not removed from the systemic circulation by dialysis.
Chlorthalidone (monotherapy)
Symptoms: nausea, weakness, dizziness, water and electrolyte imbalance.
Treatment: there is no specific antidote. If there is a pronounced decrease in blood pressure, rinse the stomach and take measures to normalize the water and electrolyte balance (infusion therapy); symptomatic therapy.
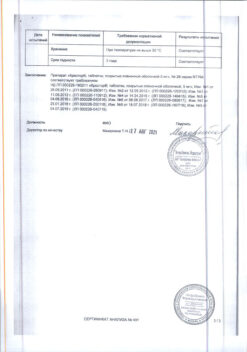
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 °C in the original packaging.
Shelf life
Shelf life
3 years.
Manufacturer
Manufacturer
Takeda Island Limited, Ireland
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C in the original package. |
| Manufacturer | Takeda Island Limited, Ireland |
| Medication form | pills |
| Brand | Takeda Island Limited |
Other forms…
Related products
Buy Edarbi Clo, 40 mg+25 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.