No products in the cart.
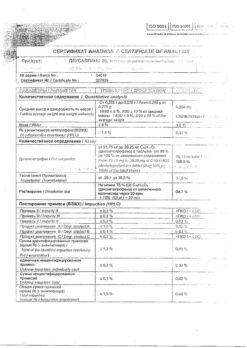
DesGrippin, 500 mg+10 mg+200 mg lime 10 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Combination drug.
Pharmacodynamics
Paracetamol has analgesic and antipyretic effects; relieves headache and other types of pain, reduces fever.
Chlorfenamine is a blocker of H1-histamine receptors, anti-allergic, helps nasal breathing, reduces nasal congestion, sneezing, lacrimation, itching and red eyes.
Ascorbic acid (vitamin C) is involved in the regulation of redox processes, carbohydrate metabolism, increases the body’s resistance.
Pharmacokinetics
Paracetamol
Absorption is high, the maximum concentration is reached after 0.5-2 hours; the maximum concentration is 5-20 µg/ml. Binding with plasma proteins is 15%. Penetrates through the blood-brain barrier. Less than 1% of the dose of paracetamol taken by a nursing mother will penetrate into breast milk. The therapeutically effective plasma concentration of paracetamol is achieved when administered at a dose of 10-15 mg/kg.
It is metabolized in the liver (90-95%): 80% enters into conjugation reactions with glucuronic acid and sulfates to form inactive metabolites; 17% undergoes hydroxylation to form 8 active metabolites, which conjugate with glutathione to form already inactive metabolites.
In glutathione deficiency these metabolites can block the enzyme systems of hepatocytes and cause their necrosis. The CYP2E1 isoenzyme is also involved in the metabolism of the drug. The elimination half-life is 1-4 hours. It is excreted by the kidneys as metabolites, mainly conjugates, only 3% unchanged. In elderly patients the drug clearance decreases and the elimination half-life increases.
Chlorphenamine maleate
Chlorphenamine is relatively slowly absorbed from the gastro-intestinal tract, the maximum plasma concentrations of chlorphenamine are reached 2.5-6 hours after taking the drug. The substance has a low bioavailability of 25-50%. About 70% of chlorphenamine in bloodstream is bound to plasma proteins. It undergoes wide distribution in body tissues including CNS.
Chlorphenamine undergoes significant metabolism during primary passage through the liver. Duration of action is 4-6 hours. In children, a faster and more complete absorption, a faster clearance and a shorter half-life are noted.
The elimination half-life ranges from 2 to 43 hours, even with an average duration of action of 4-6 hours. Part of chlorphenamine is excreted unchanged with metabolites by the kidneys.
Ascorbic acid
It is absorbed in the gastrointestinal tract (mainly in the jejunum). The binding to plasma proteins is 25%. Gastrointestinal diseases (gastric and 12 duodenal ulcer, constipation or diarrhea, helminth infestation, giardiasis), consumption of fresh fruit and vegetable juices, alkaline drinking reduce absorption of ascorbic acid in the intestine.
The plasma concentration of ascorbic acid in the normal range is approximately 10-20 µg/ml. Time of maximum concentration in blood plasma after oral administration is 4 hours. It penetrates easily into leukocytes, platelets and then into all tissues; the highest concentration is reached in glandular organs, leukocytes, liver and eye lens; penetrates through the placenta.
The concentration of ascorbic acid in leukocytes and platelets is higher than in erythrocytes and plasma. In deficiency states, the concentration in leukocytes decreases later and more slowly and is considered a better criterion for assessing deficiency than the concentration in plasma.
Metabolized primarily in the liver to deoxyascorbic acid and then to oxalic acid and ascorbate-2-sulfate. It is excreted by the kidneys, through the intestines, with sweat unchanged and as metabolites. Smoking and use of ethanol accelerate the breakdown of ascorbic acid (transformation into inactive metabolites), dramatically reducing the body’s reserves. It is excreted by hemodialysis.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
Interaction
Interaction
Paracetamol
The anticoagulant effect of warfarin and other coumarins may be enhanced with long-term regular use of paracetamol, and the risk of bleeding increases. Intermittent use of paracetamol has no significant effect.
Hepatotoxic agents can lead to accumulation of paracetamol and overdose. The risk of hepatotoxicity of paracetamol is increased when using drugs that induce microsomal liver enzymes, such as barbiturates, antiepileptic drugs (e.g., phenytoin, phenobarbital, carbamazepine) and drugs to treat tuberculosis, such as rifampicin and isoniazid.
Methoclopramide increases the rate of absorption of paracetamol and increases its maximum plasma concentration. Similarly, domperidone may increase the absorption rate of paracetamol.
Paracetamol may increase the half-life of chloramphenicol. Paracetamol may lead to decreased bioavailability of lamotrigine, with a possible reduction in the effect of the latter, which may lead to a possible induction of metabolism in the liver.
The absorption of paracetamol may be decreased when used concomitantly with colestyramine, but the decrease in absorption is insignificant if colestyramine is used one hour later.
The regular use of paracetamol concomitantly with zidovudine may cause neutropenia and increase the risk of liver damage.
Probenecid affects the metabolism of paracetamol. In patients concomitantly using probenecid, the dose of paracetamol should be reduced.
Hepatotoxicity of paracetamol is increased with prolonged excessive use of ethanol (alcohol).
Myelotoxic drugs increase the manifestation of hematoxicity of paracetamol.
Paracetamol may affect the results of uric acid phosphoric acid tests.
Phenytoin reduces the effectiveness of paracetamol, therefore, patients taking phenytoin should avoid frequent use of paracetamol, especially in high doses. Indirect anticoagulants: repeated administration of paracetamol for more than 4 days increases the anticoagulant effect.
The international normalized ratio (INR) should be monitored during and after concomitant use of paracetamol (especially in high doses and/or for a long time) and coumarin derivatives.
The irregular use of paracetamol has no significant effect. Propantelin and other drugs that slow down the evacuation from the stomach decrease the rate of absorption of paracetamol, which may delay or reduce the onset of effect.
Long-term concomitant use of paracetamol and other NSAIDs increases the risk of “analgesic” nephropathy and renal papillary necrosis, onset of end-stage renal failure. The simultaneous long-term prescription of paracetamol in high doses and salicylates increases the risk of developing kidney or bladder cancer.
Chlorphenamine maleate
. Antihistamines such as chlorphenamine can increase the effects of opioid analgesics, anticonvulsants, antidepressants (tricyclic and monoamine oxidase inhibitors), other antihistamines, antiemetics and antipsychotics, anxiolytics, sleeping pills, ethanol (alcohol) and other central nervous system depressants.
Because chlorphenamine has some anticholinergic activity, the effects of anticholinergic drugs (e.g., some psychotropic drugs, atropine, and drugs to treat urinary incontinence) may be enhanced by the use of this drug. This may lead to tachycardia, dry mouth, gastrointestinal disorders (e.g., colic), urinary retention, and headache.
Phenytoin metabolism can be inhibited by chlorphenamine, and phenytoin toxicity may develop.
Ascorbic acid
. Ascorbic acid increases absorption of drugs from penicillin group and iron, decreases clinical effect of heparin and indirect anticoagulants, increases risk of crystalluria during treatment with salicylates and short acting sulfonamides, slows down excretion of acids by kidneys, increases excretion of drugs with alkaline reaction (including alkaloids).including alkaloids), reduces the blood concentration of oral contraceptives.
It should not be prescribed in the first month of treatment with deferoxamine due to increased iron toxicity. Large doses of ascorbic acid may lead to increased plasma concentrations of ethinylestradiol in women taking oral contraceptives. Simultaneous administration of ascorbic acid and fluphenazine may lead to a decrease in plasma concentrations of fluphenazine.
Special Instructions
Special Instructions
When taking metoclopramide, domperidone or colestiramine it is also necessary to consult a physician.
Long-term use in doses significantly higher than recommended increases the possibility of liver and renal function disorders, it is necessary to monitor the peripheral blood picture.
Paracetamol and ascorbic acid can distort laboratory tests (quantitative determination of plasma glucose and uric acid, bilirubin, activity of “hepatic” transaminases, LDH).
To avoid toxic liver damage, paracetamol should not be combined with the intake of alcoholic beverages, and should not be taken by persons prone to chronic alcohol consumption. The risk of liver damage increases in patients with alcoholic hepatosis.
Patients with glutathione deficiency are prone to overdose, caution should be exercised. Cases of liver failure have been reported in patients with low glutathione levels, particularly in extremely emaciated patients, anorexic patients, those with chronic alcoholism or patients with low body mass index.
The use of paracetamol in patients with low glutathione levels, e.g., in sepsis, may increase the risk of metabolic acidosis.
Paracetamol may cause serious skin reactions, such as acute generalized exanthematous pustulosis, Stephen-Johnson syndrome, and toxic epidermal necrolysis. At the first appearance of the rash or other hypersensitivity reactions the use of the drug should be discontinued.
Prescribing ascorbic acid to patients with rapidly proliferating and intensely metastatic tumors may aggravate the course of the process. In patients with elevated iron levels in the body, ascorbic acid should be used in minimal doses.
Drowsiness may develop for several hours after taking the drug.
Contraindications
Contraindications
Hypersensitivity to paracetamol, ascorbic acid, chlorphenamine or any other component of the drug.
Erosive ulcerative lesions of the gastrointestinal tract (acute phase).
Developed renal and/or hepatic insufficiency.
Alcoholism. Closed-angle glaucoma.
Portal hypertension.
Prostatic hyperplasia.
Lactose intolerance, lactase deficiency, glucose-galactose malabsorption. Because of the aspartame content, it is contraindicated in patients with phenylketonuria.
Childhood (under 15 years).
Pregnancy and the period of breastfeeding.
Side effects
Side effects
Overdose
Overdose
The symptoms of drug overdose are caused by its constituent substances, mainly the presence of paracetamol.
Paracetamol
The clinical picture of acute overdose with paracetamol develops within 24 hours after taking it. Gastrointestinal disorders appear (nausea, vomiting, decreased appetite, abdominal discomfort and/or abdominal pain, pale skin).
Hepatocyte cytolysis with complete and irreversible liver necrosis, liver failure, metabolic acidosis and encephalopathy occurs when administered to adults 7.5 g or more or children 140 mg/kg at a time, which may lead to coma and death.
Ingestion of 5 g or more of paracetamol may lead to liver damage in the presence of risk factors (long-term treatment with carbamazepine, phenobarbital, phenytoin, primidone, rifampicin, St. John’s wort or other drugs that are inducers of microsomal liver enzymes; ethanol abuse, glutathione deficiency, digestive disorders, cystic fibrosis, HIV infection, starvation, cachexia).
Twelve to 48 hours after administration of paracetamol there is an increase in the activity of microsomal liver enzymes, lactate dehydrogenase, bilirubin concentration and prothrombin decrease. Clinical symptoms of liver damage appear 2 days after paracetamol overdose and reach their maximum on the 4th-6th day.
In overdose intoxication is possible, especially in elderly patients, children, patients with liver disease (caused by chronic alcoholism), in patients with nutritional disorders, as well as in patients taking inducers of microsomal liver enzymes, with the development of fulminant hepatitis, liver failure, cholestatic hepatitis, cytolytic hepatitis, sometimes with a fatal outcome.
In severe cases of overdose as a result of liver failure encephalopathy (impaired brain function), cerebral edema, bleeding, hypoglycemia may develop, up to death.
The development of acute renal failure with acute tubular necrosis is possible, characterized by pain in the lumbar region, hematuria (blood or red blood cells in the urine), proteinuria (high protein content in the urine), while severe liver damage may be absent. There have been cases of abnormal heart rhythm and pancreatitis.
Treatment. Immediate hospitalization. If overdose is suspected, even if there are no expressed first symptoms, paracetamol use should be stopped and medical attention should be sought immediately.
Paracetamol plasma levels should be determined, but not earlier than 4 hours after overdose (earlier results are not reliable). Laboratory studies of microsomal liver enzyme activity should be performed at the beginning of treatment and every 24 hours thereafter.
The administration of SH-group donators and precursors of glutathione synthesis – methionine and acetylcysteine – is most effective in the first 8 hours.
In 1 hour after overdose it is recommended to wash the stomach and take enterosorbents (activated charcoal, etc.). in most cases the activity of microsomal liver enzymes is normalized within 1-2 weeks.
In very severe cases, liver transplantation may be necessary. Administration of acetylcysteine within 24 hours after overdose. Maximum protective effect is provided during the first 8 hours after overdose, with time the effectiveness of the antidote decreases sharply.
If necessary, acetylcysteine is administered intravenously. In the absence of vomiting before the patient is admitted to the hospital, methionine may be used. The need for additional therapeutic measures (further administration of methionine, intravenous administration of acetylcysteine) is determined depending on the concentration of paracetamol in the blood, as well as on the time elapsed after its administration.
The treatment of patients with severe liver dysfunction 24 hours after taking paracetamol should be done in conjunction with specialists from a toxicology center or a specialized department of liver disease.
Chlorphenamine maleate
Symptoms of chlorphenamine maleate overdose include drowsiness, respiratory arrest, seizures, anticholinergic effects, dystonic reactions, and cardiovascular collapse, including arrhythmias. In children, overdose symptoms may include poor coordination, agitation, tremors, behavioral changes, hallucinations, seizures, and anticholinergic effects.
Treatment. Includes gastric lavage in cases of massive overdose, or stimulation of vomiting. This may be followed by administration of activated charcoal and laxatives to slow absorption. In case of seizures, sedation with intravenous diazepam or phenytoin should be given. In severe cases hemoperfusion may be performed.
Ascorbic acid
Symptoms of ascorbic acid overdose: nephrolithiasis, insomnia, irritability, hypoglycemia.
Treatment. Treatment of ascorbic acid overdose is symptomatic, force diuresis may be required.
Pregnancy use
Pregnancy use
Additional information
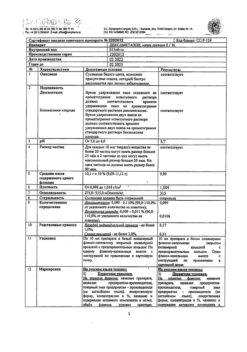
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 ° C. Keep out of reach of children. |
| Manufacturer | PharmVilar NGO, Russia |
| Medication form | effervescent tablets |
| Brand | PharmVilar NGO |
Related products
Buy DesGrippin, 500 mg+10 mg+200 mg lime 10 pcs with delivery to USA, UK, Europe and over 120 other countries.