No products in the cart.
Coromax 2 mg/ml 10 ml
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group: anti-aggregant.
ATC code: B01AC16.
Pharmacodynamics
Eptifibatide is a synthetic cyclic heptapeptide containing 6 amino acid residues, including one cysteinamide and one mercaptopropionyl residue – desaminocysteinyl. Eptifibatide is a platelet aggregation inhibitor and belongs to the class of arginine-glycine-aspartate mimetics. Eptifibatide reversibly inhibits platelet aggregation by preventing binding of fibrinogen, Willebrand factor and other adhesive ligands to glycoprotein IIb/IIIa receptors of platelets.
Eptifibatide causes dose- and concentration-dependent suppression of platelet aggregation, which has been demonstrated ex vivo with ADP and other platelet aggregation-inducing agonists. The action of eptifibatide is seen immediately after an intravenous bolus injection at a dose of 180 μg/kg. A regimen followed by continuous IV infusion at a dose of 2 µg/kg/min provides more than 80% inhibition of ADP-induced platelet aggregation ex vivo, at physiological calcium concentrations, in more than 80% of patients. The inhibition of platelet aggregation is reversible; 4 h after cessation of continuous infusion at a dose of 2 μg/kg/min, platelet function is more than 50% restored to baseline. Measurements of ADP-induced platelet aggregation ex vivo at physiological calcium concentrations (anticoagulant D-phenylalanyl-L-prolyl-L-arginine chloromethyl ketone) in patients with unstable angina and myocardial infarction without Q-wave were found to be concentration-dependent inhibition with IC50 (concentration, inhibiting aggregation by 50%) of 557 ng/mL and IC80 (concentration inhibiting aggregation by 80%) of 1107 ng/mL. Bleeding time is reversibly increased up to 5 times when Coromax is administered by bolus and infusion, and it returns to baseline within 2-6 h after stopping the infusion. When used as monotherapy, eptifibatide has no significant effect on PV and AHR.
Pharmacokinetics
The pharmacokinetics of eptifibatide are linear and dose-dependent with bolus administration in the dose range of 90 to 250 µg/kg and infusion at a rate of 0.5-3 µg/kg/min. When infused at a dose of 2 µg/kg/min in patients with CHD, the average plasma Css of eptifibatide is set at 1.5-2.2 µg/mL. This plasma concentration is achieved more rapidly if the infusion is preceded by a bolus infusion at a dose of 180 µg/kg.
The degree of binding of eptifibatide to human plasma proteins is about 25%.
In the same patient population, the T1/2 from plasma is approximately 2.5 h, plasma clearance is 55-80 ml/kg/h, Vd is approximately 185-260 ml/kg. In healthy patients the proportion of renal excretion from total clearance is about 50%; approximately 50% of the substance is excreted unchanged.
Moderate increase in T1/2 and Vd is observed in elderly patients, patients with low body weight (< 74 kg) and/or low Cl creatinine. The dose and sex of the patient do not affect the pharmacokinetics of Coromax. In mild renal failure (creatinine Cl ≥50 ml/min by Cockcroft-Gault formula) no dose adjustment is required by bolus or infusion. In moderate renal failure (creatinine Cl ≥30 – < 50 ml/min by the Cockcroft-Gault formula) a dose adjustment is recommended. In patients with renal insufficiency of moderate or severe degree (creatinine Cl < 50 ml/min) a decrease of eptifibatide clearance by approximately 50% and increase of Css in plasma by approximately 2 times is observed (see “Special notes”, “Dosage and administration”).
Indications
Indications
early prevention of myocardial infarction in patients with unstable angina or myocardial infarction without a Q wave, who noted the last painful attack within 24 hours, with changes in the ECG and/or increased activity of cardiac-specific enzymes;
prevention of sudden closure of the vessel and associated acute ischemic complications during percutaneous transluminal coronary angioplasty (PTCA).
Eptifibatide is intended for use in combination with acetylsalicylic acid and unfractionated heparin.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antiplatelet agent.
ATX code: B01AC16.
Pharmacodynamics
Eptifibatide is a synthetic cyclic heptapeptide containing 6 amino acid residues, including one cysteinamide and one mercaptopropionyl residue, desaminocysteinyl. Eptifibatide is an inhibitor of platelet aggregation and belongs to the class of arginine-glycine-aspartate mimetics. Eptifibatide reversibly inhibits platelet aggregation by preventing the binding of fibrinogen, von Willebrand factor and other adhesive ligands to platelet glycoprotein IIb/IIIa receptors.
Eptifibatide causes a dose- and concentration-dependent inhibition of platelet aggregation, which has been demonstrated ex vivo using ADP and other platelet aggregation-inducing agonists. The effect of eptifibatide is observed immediately after intravenous bolus administration at a dose of 180 mcg/kg. The regimen followed by a continuous IV infusion at a dose of 2 mcg/kg/min provided greater than 80% inhibition of ex vivo ADP-induced platelet aggregation at physiological calcium concentrations in more than 80% of patients. Inhibition of platelet aggregation is reversible; 4 hours after stopping the continuous infusion at a dose of 2 mcg/kg/min, platelet function is restored by more than 50% to its original level. Ex vivo measurements of ADP-induced platelet aggregation at physiological concentrations of calcium (the anticoagulant D-phenylalanyl-L-prolyl-L-arginine chloromethylketone) in patients with unstable angina and non-Q wave myocardial infarction revealed a concentration-dependent inhibition with an IC50 (concentration that inhibits aggregation by 50%) of 557 ng/ml, and IC80 (concentration that inhibits aggregation by 80%) of 1107 ng/ml. The bleeding time when using the drug Coromax intravenously in the form of a bolus and infusion increases reversibly up to 5 times, this indicator returns to the original level within 2-6 hours after stopping the infusion. When used as monotherapy, eptifibatide does not have a significant effect on PT and APTT.
Pharmacokinetics
The pharmacokinetics of eptifibatide is linear and dose-dependent when administered as a bolus in the dose range from 90 to 250 mcg/kg and infused at a rate of 0.5–3 mcg/kg/min. When infused at a dose of 2 mcg/kg/min in patients with coronary artery disease, the average Css of eptifibatide in plasma is established in the range of 1.5–2.2 mcg/ml. This plasma concentration is achieved more quickly if the infusion is preceded by a bolus dose of 180 mcg/kg.
The degree of binding of eptifibatide to human plasma proteins is about 25%.
In the same patient population, T1/2 from plasma is approximately 2.5 hours, plasma clearance is 55-80 ml/kg/h, Vd is approximately 185-260 ml/kg. In healthy patients, the proportion of renal excretion of the total clearance is about 50%; approximately 50% of the substance is excreted in unchanged form.
A moderate increase in T1/2 and Vd is observed in older patients, patients with reduced body weight (<74 kg) and/or reduced creatinine Cl. The dose size and gender of the patient do not affect the pharmacokinetics of the drug Coromax. For mild renal failure (creatinine Cl ≥50 ml/min according to the Cockroft-Gault formula), no dose adjustment is required for bolus or infusion administration. For moderate renal failure (creatinine Cl ≥30 - <50 ml/min according to the Cockcroft-Gault formula), dose adjustment is recommended. In patients with moderate or severe renal insufficiency (Cl creatinine < 50 ml/min), there is a decrease in clearance of eptifibatide by approximately 50% and an increase in plasma Css by approximately 2 times (see “Special Instructions”, “Dosage and Administration”).
Special instructions
Special instructions
Eptifibatide is for use in hospital settings only.
Bleeding
Eptifibatide is an antithrombotic agent that inhibits platelet aggregation; therefore, during treatment with eptifibatide, all patients should be carefully examined to identify possible bleeding, especially women, elderly patients, and patients with low body weight, as they have the greatest risk of bleeding (see “Side effects”). If serious bleeding occurs that cannot be controlled by applying a pressure bandage, the infusion of the drug and any concomitant heparin should be stopped immediately.
The risk of bleeding in patients undergoing PTCA is greatest at the arterial access site. It is necessary to carefully monitor sites of possible bleeding, for example, the site of catheter insertion, arterial puncture, venipuncture or needle puncture, venesection; One should keep in mind the possibility of bleeding from the gastrointestinal tract and genitourinary tract, retroperitoneal bleeding. Bleeding in the central and peripheral nervous system is also possible.
Control of access to the femoral artery
When using eptifibatide, the risk of bleeding is greatest at the site of insertion of the catheter into the femoral artery during PTCA. Care should be taken to ensure that only the anterior wall of the femoral artery is punctured. The introducer from the femoral artery can be removed after the coagulation function is restored to normal: ABC – less than 180 s (usually 2-6 hours after discontinuation of heparin). After removal of the sheath, hemostasis should be performed followed by careful observation until discharge from the hospital.
Thrombocytopenia and immunogenicity associated with the use of IIb/IIIa receptor inhibitors
Eptifibatide inhibits platelet aggregation but does not affect platelet viability. The incidence of thrombocytopenia was low and similar to that in patients receiving placebo, which was observed both during clinical trials and in rare case reports of immune thrombocytopenia during post-marketing surveillance. The presence of transportable factors in plasma that can bind to eptifibatide and glycoprotein IIb/IIIa receptors means that an immune thrombocytopenic response may develop when receiving glycoprotein IIb/IIIa receptor inhibitors for the first time or in patients repeatedly receiving eptifibatide.
The mechanism (immune and/or non-immune) of the effect of eptifibatide on the development of thrombocytopenia has not been fully studied. Because repeated exposure to any glycoprotein IIb/IIIa receptor inhibitor (including abciximab or eptifibatide) or primary exposure to glycoprotein IIb/IIIa receptor inhibitors may be accompanied by a thrombocytopenic immune-mediated response, caution should be exercised and monitored for possible cases of thrombocytopenia accompanied by hypotension and/or other symptoms of hypersensitivity.
If a decrease in platelet count to < 100,000/mm3 or acute deep thrombocytopenia is confirmed, discontinuation of treatment with any drugs that may have a thrombocytopenic effect, including. eptifibatide, heparin and clopidogrel. It is necessary to begin maintenance therapy, as well as monitor the platelet count to adjust treatment and establish the etiology. If thrombocytopenia is not associated with the use of eptifibatide, therapy with it can be resumed after the platelet count has normalized.
Increased bleeding time
Bleeding time when using IV eptifibatide as a bolus and infusion increases up to 5 times. This increase is quickly reversible after stopping the infusion; this indicator returns to the initial level within 2-6 hours. When used as monotherapy, eptifibatide does not have a significant effect on PT and aPTT.
Use of heparin
The combined use of eptifibatide and heparin is recommended in all cases, in the absence of contraindications to the use of heparin, incl. history of thrombocytopenia associated with heparin use.
Patients with unstable angina or non-Q wave myocardial infarction. For patients weighing 70 kg or more, the recommended bolus dose is 5000 units, followed by a continuous infusion of 1000 units/hour. For patients weighing less than 70 kg, the bolus dose is 60 units/kg, followed by infusion 12 units/kg/hour. APTT should be monitored to maintain values in the range of 50–70 s.
Coronary angioplasty. When performing PTCA in patients, it is necessary to monitor ABC; its values should be within 300–350 s. If the ABC value exceeds 300 s, heparin use should be stopped and not resumed until the value drops below 300 s.
Non-emergency PTCA with intracoronary stenting. For patients who have not received heparin within 6 hours before surgery, an initial heparin bolus of 60 units/kg is recommended. The target ABC during the procedure is 200–300 s. During the PTCA procedure, an additional bolus of heparin may be administered to maintain the ABC value in this range.
Patients with liver failure
Experience with eptifibatide in patients with hepatic impairment is extremely limited (see “Contraindications”). In case of liver failure, the drug should be used with caution, because In such patients, the drug may affect blood clotting.
Patients with kidney failure
For mild renal failure (Cl creatinine ≥50 ml/min according to the Cockcroft-Gault formula), eptifibatide can be safely used at standard dosages. In moderate to severe renal failure (Cl creatinine < 50 ml/min according to the Cockcroft-Gault formula), the clearance of eptifibatide is reduced by approximately 50%, and plasma Css are approximately doubled. Patients with moderate or severe renal impairment receiving conventional infusions at a dose of 2 mcg/kg/min are at increased risk of bleeding. Therefore, in such patients, the infusion dose should be reduced to 1 mcg/kg/min (see “Dosage and Administration”). No clinical studies have been conducted in patients undergoing dialysis.
Children under 18 years old
The safety and effectiveness of eptifibatide in patients under 18 years of age have not been established; therefore, use in this category of patients is not recommended.
Laboratory monitoring
Changes in laboratory parameters during treatment with eptifibatide are a consequence of the known pharmacological properties of the drug, incl. inhibition of platelet aggregation. Thus, changes in laboratory parameters characterizing bleeding (including bleeding time) are observed frequently and are expected. When using eptifibatide and when using placebo, there were no obvious differences in indicators such as Hb, hematocrit, platelet count, liver function parameters (AST, ALT, bilirubin, ALP concentration) and kidney function (serum creatinine, blood urea nitrogen concentrations).
Influence on the ability to drive vehicles and machinery. Eptifibatide is intended for use in hospital settings. There are no data on the use of eptifibatide in outpatients.
Active ingredient
Active ingredient
Eptifibatide
Composition
Composition
1 ml of solution for intravenous administration contains:
Active ingredient: eptifibatide – 0.75 mg or 2.0 mg;
Excipients: citric acid monohydrate – 5.25 mg, sodium hydroxide – up to pH 5.25 (from 1.7 to 220 mg), water for injection – q.s. up to 1.0 ml.
Pregnancy
Pregnancy
No clinical studies have been conducted on the use of eptifibatide in pregnant women. However, reproductive studies were conducted in rats and rabbits using doses 8 and 4 times higher than the human dose, respectively. In these studies, there was no evidence of impaired fertility or adverse effects on the fetus associated with the use of eptifibatide.
Since animal studies are not considered sufficient to predict possible reactions in humans, eptifibatide should be used during pregnancy only when the benefit to the mother outweighs the potential risk to the fetus.
There is no data on the penetration of eptifibatide into breast milk. It is recommended to discontinue breastfeeding while using eptifibatide.
Contraindications
Contraindications
Hypersensitivity to eptifibatide or any other component of the drug;
stomach or intestinal bleeding, serious genital (excluding menstrual bleeding) and urological bleeding or other significant abnormal bleeding during the last 30 days;
acute cerebrovascular accident within the last 30 days or a history of hemorrhagic stroke;
intracranial diseases (neoplasia, arteriovenous malformation, aneurysm);
“major” surgery or major trauma within the last 6 weeks;
history of hemorrhagic diathesis;
thrombocytopenia (< 100,000 cells/mm³);
prothrombin time (PT) more than 1.2 from the PT of control plasma or international normalized ratio (INR) >2.0;
severe arterial hypertension (systolic blood pressure above 200 mm Hg or diastolic blood pressure above 110 mm Hg) during antihypertensive therapy;
clinically significant liver failure;
severe renal failure (creatinine clearance <30 ml/min) or the need for hemodialysis;
simultaneous or planned use of another glycoprotein IIb/IIIa platelet receptor inhibitor for parenteral administration;
Children under 18 years of age (no experience of use).
With caution
Caution should be exercised when using eptifibatide simultaneously with other drugs that affect the hemostatic system: thrombolytics, oral anticoagulants, dextran solutions, adenosine, non-steroidal anti-inflammatory drugs, including sulfinpyrazone, drugs containing prostacyclin, dipyridamole, ticlopidine and clopidogrel.
The risk of bleeding with simultaneous use of the drug eptifibatide and streptokinase, used to treat acute myocardial infarction, increases.
The combined use of eptifibatide and heparin is recommended in all cases, unless there is a contraindication to the use of heparin, for example, a history of thrombocytopenia associated with heparin use.
Due to the lack of clinical experience, the use of eptifibatide simultaneously with low molecular weight heparin should be used with caution.
Side Effects
Side Effects
Most adverse events with eptifibatide are related to bleeding or cardiac or cardiovascular events, which are common in this patient population.
Clinical data
The incidence of adverse events presented below was based on two phase III clinical studies (PURSUIT and ESPRIT).
PURSUIT was a double-blind, randomized study of the efficacy and safety of eptifibatide versus placebo to reduce mortality and recurrent myocardial infarction in patients with unstable angina or non-Q wave myocardial infarction.
ESPRIT was a double-blind, multicenter, randomized, placebo-controlled, parallel-group study examining the safety and efficacy of eptifibatide in patients scheduled for non-emergency PCI with intracoronary stenting.
Data on adverse events, incl. bleeding in the PURSUIT study were administered from hospital discharge to the 30-day visit. Bleeding events in the ESPRIT study were recorded for 48 hours, and non-bleeding events were recorded for 30 days. The TIMI (Thrombolysis in Myocardial Infarction Study Group) bleeding criteria were used to classify the incidence of major and minor bleeding in the PURSUIT and ESPRIT studies. Data from the PURSUIT study were collected for 30 days, while data from the ESPRIT study were limited to events that occurred within 48 hours or before discharge, whichever occurred first.
When used at the recommended therapeutic doses used in the PURSUIT study (involving approximately 11,000 patients), bleeding was the most common complication of eptifibatide therapy. Invasive cardiac procedures (coronary artery bypass surgery or femoral artery access) were most often associated with bleeding.
In the PURSUIT study, minor bleeding was defined as spontaneous gross hematuria, spontaneous hematemesis, bleeding with a decrease in Hb concentration ≥3 g/dL, or a decrease in Hb concentration ≥4 g/dL in the absence of a visible source of bleeding. Minor bleeding was a very common complication of eptifibatide (>1/10 or 13.1% with eptifibatide versus 7.6% with placebo). Bleeding was observed more frequently in patients concomitantly receiving heparin during PCI when the activated clotting time (ACT) exceeded 350 s (see “Special Instructions”, Use of Heparin).
In the PURSUIT study, major bleeding was defined as intracranial bleeding or Hb concentration ≥5 g/dL. Major bleeding was very common with eptifibatide in this study (>1/10 or 10.8% with eptifibatide versus 9.3% with placebo), excluding the vast majority of patients who did not undergo coronary artery bypass grafting within 30 days of enrollment, in whom this event was observed infrequently. In patients undergoing coronary artery bypass grafting, the incidence of bleeding was not increased with eptifibatide compared with patients receiving placebo. In the subgroup of patients undergoing PCI, major bleeding was common: 9.7% of patients treated with eptifibatide compared with 4.6% of patients treated with placebo.
The incidence of severe or life-threatening bleeding with eptifibatide was 1.9% compared with 1.1% with placebo. When using eptifibatide, the need for blood transfusions moderately increased (11.8% – eptifibatide, 9.3% – placebo).
The adverse events presented below are listed according to the damage to organs and organ systems and the frequency of occurrence. The frequency of occurrence is determined as follows: very often (≥1/10); often (≥1/100 and <1/10); uncommon (≥1/1000 and <1/100); rare (≥1/10000 and <1/1000); very rare (≥1/10000, including isolated cases). The absolute frequency of reports is indicated without taking into account the frequency when using placebo. When individual adverse event data were available from two studies (PURSUIT and ESPRIT), the highest reported incidence was used to determine the incidence of adverse events.
It should be noted that a relationship with the use of the drug was not established for all adverse events.
The incidence of serious adverse events not related to bleeding (including hypotension) with eptifibatide did not differ from that with placebo.
From the blood and lymphatic system: very often – bleeding (massive and light bleeding, including bleeding during coronary artery bypass grafting and access through the femoral artery, gastrointestinal bleeding, genitourinary bleeding, retroperitoneal and intracranial bleeding, hematemesis, hematuria, intraoral/oropharyngeal bleeding, bleeding that reduces hematocrit/Hb); infrequently – thrombocytopenia.
From the nervous system: infrequently – cerebral ischemia.
From the heart: often – cardiac arrest, ventricular fibrillation, ventricular tachycardia, congestive heart failure, AV block, atrial fibrillation.
From the side of blood vessels: often – cardiogenic shock, arterial hypotension, phlebitis.
Cardiac arrest, congestive heart failure, atrial fibrillation, hypotension, and cardiogenic shock, which were frequently reported in the PURSUIT study, were events related to the underlying disease.
Post-registration observation data
From the blood and lymphatic system: very rarely – fatal bleeding (mainly affecting the central and peripheral nervous system: hemorrhagic stroke or intracranial bleeding), pulmonary hemorrhage, acute deep thrombocytopenia, hematoma.
From the immune system: very rarely – anaphylactic reactions.
From the skin and subcutaneous tissues: very rarely – skin rash, adverse events at the injection site (including urticaria).
Interaction
Interaction
Eptifibatide does not cause an increased risk of major or minor bleeding when used concomitantly with warfarin and dipyridamole. In patients with a PT value of 14.5 seconds receiving eptifibatide concomitantly with warfarin, there was no increased risk of bleeding.
There are limited data on the use of eptifibatide in patients receiving thrombolytic agents. There is no confirmed data indicating that eptifibatide increases the risks of tissue plasminogen activator-related major and minor bleeding in either patients undergoing PTCA or patients with acute myocardial infarction. However, in clinical studies, eptifibatide increased the risk of bleeding when administered with streptokinase in patients with acute myocardial infarction. In a study of 181 patients with acute myocardial infarction, eptifibatide (bolus dose up to 180 mcg/kg, followed by infusion up to 2 mcg/kg/min for up to 72 hours) was administered simultaneously with streptokinase (1.5 million units over 60 minutes). At the highest infusion rates (1.3 mcg/kg/min and 2 mcg/kg/min), eptifibatide was associated with an increased incidence of bleeding and transfusion requirements compared with streptokinase monotherapy.
In a clinical trial in patients with acute ST-segment elevation myocardial infarction, coadministration of a reduced-dose combination of tenecteplase and eptifibatide resulted in a significant increase in the risk of major and minor bleeding (compared to placebo and eptifibatide without tenecteplase).
Eptifibatide is not compatible with furosemide.
In clinical studies, 95% of patients undergoing non-emergency PCI with intracoronary stenting were prescribed clopidogrel concomitantly with acetylsalicylic acid before or within 48 hours after PCI and daily after PCI.
No specific studies have been conducted to study the PCF of eptifibatide with other drugs. In clinical studies, no PCF was detected between eptifibatide and drugs commonly used in patients with cardiovascular diseases, such as amlodipine, atenolol, atropine, captopril, cefazolin, diazepam, digoxin, diltiazem, diphenhydramine, enalapril, fentanyl, furosemide, heparin, lidocaine, lisinopril, metoprolol, midazolam, morphine, nitrates, nifedipine, warfarin.
Overdose
Overdose
Information on eptifibatide overdose is very limited. There is no information about serious adverse reactions associated with accidental overdose with jet or drip administration, as well as when the cumulative dose is exceeded.
The PURSUIT clinical trial reported on 9 patients who received bolus and/or infusion doses greater than 2 times the recommended dose. However, none of the patients experienced unstoppable bleeding; one of the patients underwent coronary artery bypass surgery and experienced only moderate bleeding; No patients experienced intracranial bleeding.
Potentially, an overdose of eptifibatide may cause bleeding.
Treatment: due to the short T1/2 and high clearance, the effect of the drug can be quickly stopped by stopping administration.
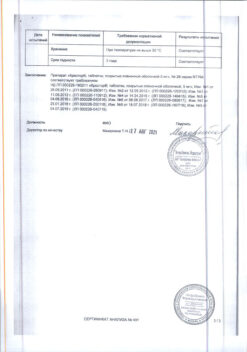
Storage conditions
Storage conditions
At temperatures from 2 to 8 °C. Do not freeze.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Manufacturer
Manufacturer
Jodas Expoim Pvt.Ltd, India
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | At a temperature of 2 to 8 ° C. Do not freeze. Keep out of reach of children. |
| Manufacturer | Jodas Expoim Pvt. Ltd, India |
| Medication form | solution for injection |
| Brand | Jodas Expoim Pvt. Ltd |
Related products
Buy Coromax 2 mg/ml 10 ml with delivery to USA, UK, Europe and over 120 other countries.