No products in the cart.
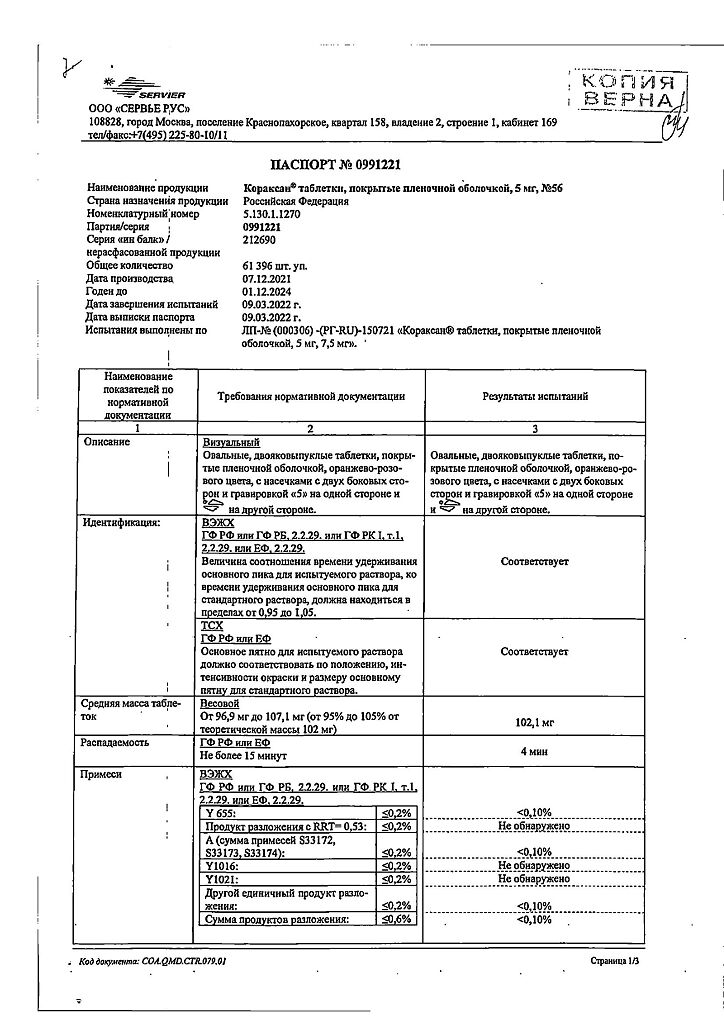
Coraxan, 5 mg 56 pcs
€33.30 €27.75
Description
Ivabradine is a heart rhythm slowing drug whose mechanism of action consists in selective and specific inhibition of If sinus node channels that control spontaneous diastolic depolarization in the sinus node and regulate heart rate (HR). Ivabradine has a selective effect on the sinus node without affecting the timing of impulse conduction along the intraatrial, atrial-ventricular and intraventricular conduction pathways, as well as on myocardial contractility and ventricular repolarization.
Ivabradine may also interact with the Ih channels of the retina, similar to the If channels of the heart, involved in causing temporary changes in the visual perception system by changing the retinal response to bright light stimuli.
In provocative circumstances (e.g., a rapid change in brightness in the visual field), partial inhibition of the Ih channels by ivabradine causes the phenomenon of changes in light perception (photopsia). Photopsia is characterized by a transient change in brightness in a limited area of the visual field (see section “Side effects”). The main pharmacological feature of ivabradine is the ability of dose-dependent reduction of heart rate (HR). Analysis of dose-related HR slows-down was performed with gradual increase of iwabradine dose up to 20 mg twice daily and showed the tendency to reach the “plateau” effect (no increase of therapeutic effect with further dose increase), which reduces the risk of bradycardia (HR under 40 bpm) (see section “Side effect”).
When administering the drug in the recommended doses, the degree of HR reduction depends on its initial value and is about 10-15 beats/min at rest and during physical activity. As a result, heart work decreases and myocardial oxygen demand decreases.
Ivabradine has no effect on intracardiac conduction, myocardial contractility (does not cause negative inotropic effect) and the process of ventricular repolarization. In clinical electrophysiological studies, ivabradine had no effect on the pulse conduction time along the atrial-ventricular or intraventricular conduction pathways, as well as on the corrected QT intervals. In studies involving patients with left ventricular dysfunction (left ventricular ejection fraction (LVEF) 30-45%) it has been shown that ivabradine has no effect on myocardial contractility.
Ivabradine in a dose of 5 mg twice daily was found to improve exercise test values after 3-4 weeks of therapy. The efficacy was also confirmed for the dose of 7.5 mg 2 times daily. In particular, an additional effect of increasing the dose from 5 to 7.5 mg 2 times a day was established in a comparative study with atenolol. Exercise time increased by about 1 minute after 1 month of using ivabradine at a dose of 5 mg 2 times a day, and after an additional 3-month course of taking ivabradine at a dose of 7.5 mg 2 times a day orally, a further increase of 25 seconds in this parameter was noted. Antianginal and anti-ischemic activity of ivabradine was also confirmed for patients aged 65 years and older. The efficacy of ivabradine when used in doses of 5 mg and 7.5 mg 2 times daily was observed for all exercise test parameters (total exercise duration, time to limiting angina attack, time to onset of angina attack and time to ST-segment depression by 1 mm) and was accompanied by approximately 70% reduction of angina attack frequency. Administration of ivabradine 2 times a day provided continuous therapeutic efficacy for 24 hours.
In patients taking ivabradine additional efficacy of ivabradine in all exercise test parameters was shown when added to the maximum dose of atenolol (50 mg) at the therapeutic decline (12 hours after oral administration).
No improvement in the efficacy of ivabradine has been shown when added to the maximum dose of amlodipine at the onset of therapeutic activity (12 hours after oral administration), whereas at the peak of activity (3 to 4 hours after oral administration) additional efficacy of ivabradine has been demonstrated.
In clinical efficacy studies, the effects of ivabradine were fully sustained over 3 and 4 month treatment periods. There were no signs of tolerance (decrease in efficacy) during treatment, and no “withdrawal” syndrome was observed after discontinuation of treatment. Antianginal and anti-ischemic effects of ivabradine were associated with dose-dependent reduction of HR, as well as with a significant reduction of the work product (HR × systolic blood pressure), both at rest and during physical activity. The effects on blood pressure (BP) and total peripheral vascular resistance (TPR) were insignificant and clinically insignificant.
Sustained HR slowing was noted in patients taking ivabradine for at least 1 year. No effect on carbohydrate metabolism and lipid profile was observed.
In patients with diabetes mellitus the efficacy and safety of ivabradine were similar to those in the general patient population.
. No differences were found between the groups of patients who received ivabradine against standard therapy and patients with stable angina and left ventricular dysfunction (LVEF less than 40%), 86.9% of whom received beta-adrenoblockers, and placebo, in the cumulative incidence of cardiovascular deaths, hospitalization for acute myocardial infarction, hospitalization for new cases of heart failure or increased symptoms of chronic heart failure (CHF), and in a subgroup of patients with a HR of at least 70 bpm./min.
The use of ivabradine in patients with HR of 70 bpm or higher was shown to decrease the rate of hospitalizations for fatal and non-fatal myocardial infarction by 36% and the rate of revascularization by 30%.
In patients with angina pectoris on ivabradine 24 % decrease of relative risk of complications (rate of cardiovascular deaths, hospitalization for acute myocardial infarction, hospitalization for new cases of heart failure or increase of CHF symptoms) was noted. The noted therapeutic benefit is achieved primarily due to a 42% reduction in the rate of hospitalization for acute myocardial infarction.
Reduction of hospitalization rate for fatal and non-fatal myocardial infarction in patients with HR over 70 bpm is even more significant and reaches 73 %. In general, good tolerability and safety of the drug were noted.
In iwabradine use in patients with CHF of II-IV functional class according to NYHA classification with LVEF less than 35 % showed clinically and statistically significant 18 % decrease of relative risk of complications (incidence of cardiovascular deaths and decrease of hospitalization rate due to elevated symptoms of CHF). The absolute risk reduction was 4.2%. Expressed therapeutic effect was observed after 3 months from the therapy start.
The decrease of cardiovascular mortality and decrease of hospitalizations due to the worsening of CHF symptoms was observed regardless of age, sex, functional class of CHF, beta-adrenoblockers use, ischemic or non-ischemic etiology of CHF, presence of diabetes mellitus or hypertension in anamnesis.
Patients with symptoms of CHF with sinus rhythm and a HR of at least 70 bpm received standard therapy./min received standard therapy including beta-adrenoblockers (89%), angiotensin-converting enzyme (ACE) inhibitors and/or angiotensin II receptor antagonists (91%), diuretics (83%), and aldosterone antagonists (60%).
The use of ivabradine for 1 year has been shown to prevent one death or one hospitalization due to cardiovascular disease for every 26 patients taking the drug. Improvement of functional class of coronary artery disease according to NYHA classification was shown during use of ivabradine.
In patients with an HR of 80 bpm there was an average decrease in HR of 15 bpm.
Pharmacokinetics
Ivabradine is an S-enantiomer, with no bioconversion according to in vivo studies. The main active metabolite of the drug is the N-desmethylated derivative of ivabradine.
Absorption and bioavailability
Ivabradine is rapidly and almost completely absorbed in the gastrointestinal tract after oral administration. Maximum concentration (Cmax ) in blood plasma is reached approximately 1 hour after oral administration on an empty stomach. Bioavailability is approximately 40%, which is due to the effect of “first passage” through the liver.
Eating increases absorption time by about 1 hour and increases plasma concentration from 20% to 30%. In order to reduce the variability of concentrations the drug is recommended to be taken simultaneously with meals (see section “Dosage and administration”).
Distribution
The binding to plasma proteins is approximately 70%. The volume of distribution in the equilibrium state is about 100 l. Cmax in plasma after long-term use at the recommended dose of 5 mg twice daily is approximately 22 ng/ml (coefficient of variation = 29 %). Mean equilibrium plasma concentration is 10 ng/ml (coefficient of variation=38%).
The metabolism of Ivabradine is largely metabolized in the liver and intestine by oxidation involving only cytochrome P450 3A4 (CYP3A4 isoenzyme). The main active metabolite is N-desmethylated derivative (S 18982), which accounts for 40% of the dose concentration of ivabradine. Metabolism of the active metabolite of ivabradine also occurs in the presence of CYP3A4 isoenzyme. Ivabradine has low affinity to CYP3A4 isoenzyme and does not induce or inhibit it. Therefore, it is unlikely that ivabradine affects the metabolism or plasma concentrations of CYP3A4 isoenzyme substrates. On the other hand, concomitant use of potent cytochrome P450 inhibitors or inducers may significantly affect the plasma concentration of ivabradine (see sections “Interaction with other medicinal products” and “Cautions”).
Elimination
The elimination half-life (T1/2 ) of ivabradine is, on average, 2 hours (70-75% of the area under the concentration-time curve (AUC)), effective T1/2 is 11 hours. Total clearance is approximately 400 ml/min, renal clearance approximately 70 ml/min. Metabolites are excreted at the same rate through the kidneys and intestines. About 4% of the taken dose is excreted unchanged by the kidneys.
Linearity and nonlinearity
The pharmacokinetics of ivabradine are linear in the dose range of 0.5 to 24 mg.
Indications
Indications
Stable angina
Treatment of stable angina in patients with normal sinus rhythm:
– if you are intolerant or have contraindications to the use of beta-blockers
– in combination with beta-blockers with inadequate control of stable angina against the background of the optimal dose of beta-blocker
Chronic heart failure
To reduce the incidence of cardiovascular complications (mortality from cardiovascular diseases and hospitalization due to increased symptoms of heart failure) in patients with chronic heart failure, with sinus rhythm and a heart rate of at least 70 beats/min.
Pharmacological effect
Pharmacological effect
Ivabradine is a drug that slows the heart rate, the mechanism of action of which is the selective and specific inhibition of If channels of the sinus node, which control spontaneous diastolic depolarization in the sinus node and regulate heart rate (HR). Ivabradine has a selective effect on the sinus node, without affecting the timing of impulses along the intra-atrial, atrioventricular and intraventricular pathways, as well as on myocardial contractility and ventricular repolarization.
Ivabradine may also interact with the Ih channels of the retina, similar to the If channels of the heart, which are involved in causing temporary changes in the visual perception system by changing the retinal response to bright light stimuli.
Under provoking circumstances (for example, a rapid change in brightness in the visual field), partial inhibition of Ih channels by ivabradine causes the phenomenon of changes in light perception (photopsia). Photopsia is characterized by a transient change in brightness in a limited area of the visual field (see section “Side effects”). The main pharmacological feature of ivabradine is the ability to dose-dependently reduce heart rate (HR). An analysis of the dependence of the magnitude of the decrease in heart rate on the dose of the drug was carried out with a gradual increase in the dose of ivabradine to 20 mg twice a day and revealed a tendency to achieve a “plateau” effect (no increase in the therapeutic effect with a further increase in the dose), which reduces the risk of developing severe bradycardia (heart rate less than 40 beats/min) (see section “Side effects”).
When the drug is prescribed in recommended doses, the degree of decrease in heart rate depends on its initial value and is approximately 10-15 beats/min at rest and during physical activity. As a result, the work of the heart decreases and the myocardium’s need for oxygen decreases.
Ivabradine does not affect intracardiac conduction, myocardial contractility (does not cause a negative inotropic effect) and the process of repolarization of the ventricles of the heart. In clinical electrophysiological studies, ivabradine had no effect on the timing of impulses along the atrioventricular or intraventricular pathways, as well as on corrected QT intervals. In studies involving patients with left ventricular dysfunction (left ventricular ejection fraction (LVEF) 30-45%), ivabradine was shown to have no effect on myocardial contractility.
It was found that ivabradine at a dose of 5 mg 2 times a day improved the performance of stress tests after 3-4 weeks of therapy. Efficacy was also confirmed for a dose of 7.5 mg 2 times a day. In particular, an additional effect when increasing the dose from 5 to 7.5 mg 2 times a day was established in a comparative study with atenolol. The time required to perform physical activity increased by approximately 1 minute after 1 month of using ivabradine at a dose of 5 mg 2 times a day, while after an additional 3-month course of taking ivabradine at a dose of 7.5 mg 2 times a day orally, a further increase of this indicator by 25 seconds was noted. The antianginal and anti-ischemic activity of ivabradine was also confirmed in patients aged 65 years and older. The effectiveness of ivabradine when used in doses of 5 mg and 7.5 mg 2 times a day was observed in relation to all indicators of stress tests (total duration of physical activity, time to a limiting attack of angina, time to the onset of an angina attack and time to the development of ST segment depression by 1 mm), and was also accompanied by a decrease in the incidence of angina attacks by approximately 70%. The use of ivabradine 2 times a day provided constant therapeutic efficacy for 24 hours.
In patients taking ivabradine, additional effectiveness of ivabradine was shown in relation to all indicators of stress tests when added to the maximum dose of atenolol (50 mg) at the decline of therapeutic activity (12 hours after oral administration).
There is no improvement in the effectiveness of ivabradine when added to the maximum dose of amlodipine at the decline in therapeutic activity (12 hours after oral administration), while at the maximum of activity (3 to 4 hours after oral administration), the additional effectiveness of ivabradine has been proven.
In clinical efficacy studies of the drug, the effects of ivabradine were fully maintained over the 3- and 4-month treatment periods. During treatment, there were no signs of the development of tolerance (decreased effectiveness), and after cessation of treatment, no withdrawal syndrome was observed. The antianginal and anti-ischemic effects of ivabradine were associated with a dose-dependent decrease in heart rate, as well as a significant decrease in the work product (heart rate × systolic blood pressure), both at rest and during exercise. The effect on blood pressure (BP) and total peripheral vascular resistance (TPVR) was minor and clinically insignificant.
A sustained decrease in heart rate was observed in patients taking ivabradine for at least 1 year. No effect on carbohydrate metabolism and lipid profile was observed.
In patients with diabetes mellitus, the efficacy and safety of ivabradine were similar to those in the general patient population.
There were no differences between the groups of patients taking ivabradine against the background of standard therapy, and in patients with stable angina and left ventricular dysfunction (LVEF less than 40%), 86.9% of whom received beta-blockers, and placebo, in the total incidence of deaths from cardiovascular diseases, hospitalization for acute myocardial infarction, hospitalization for new cases of heart failure or worsening symptoms of chronic heart disease failure (CHF) and in the subgroup of patients with a heart rate of at least 70 beats/min.
When using ivabradine in patients with a heart rate of at least 70 beats/min. showed a reduction in the rate of hospitalization for fatal and non-fatal myocardial infarction by 36% and a decrease in the rate of revascularization by 30%.
In patients with angina pectoris while taking ivabradine, there was a reduction in the relative risk of complications (the incidence of deaths from cardiovascular diseases, hospitalization for acute myocardial infarction, hospitalization for new cases of heart failure or increased symptoms of CHF) by 24%. The noted therapeutic benefit is achieved primarily by reducing the frequency of hospitalization for acute myocardial infarction by 42%.
The reduction in the incidence of hospitalization for fatal and non-fatal myocardial infarction in patients with heart rate more than 70 beats/min is even more significant and reaches 73%. In general, the drug was well tolerated and safe.
The use of ivabradine in patients with CHF II-IV functional class according to the NYHA classification with LVEF less than 35% showed a clinically and statistically significant reduction in the relative risk of complications (the incidence of deaths from cardiovascular diseases and a reduction in the frequency of hospitalizations due to increased symptoms of CHF) by 18%. The absolute risk reduction was 4.2%. A pronounced therapeutic effect was observed 3 months from the start of therapy.
A decrease in mortality from cardiovascular diseases and a decrease in the frequency of hospitalizations due to increased symptoms of CHF was observed regardless of age, gender, functional class of CHF, the use of beta-blockers, ischemic or non-ischemic etiology of CHF, the presence of diabetes mellitus or a history of arterial hypertension.
Patients with symptoms of CHF in sinus rhythm and with a heart rate of at least 70 beats/min received standard therapy, including the use of beta-blockers (89%), angiotensin-converting enzyme (ACE) inhibitors and/or angiotensin II receptor antagonists (91%), diuretics (83%), and aldosterone antagonists (60%).
It has been shown that use of ivabradine for 1 year can prevent one death or one hospitalization due to cardiovascular disease for every 26 patients taking the drug. The use of ivabradine showed an improvement in the functional class of CHF according to the NYHA classification.
In patients with a heart rate of 80 beats/min, a decrease in heart rate by an average of 15 beats/min was noted.
Pharmacokinetics
Ivabradine is the S-enantiomer, with no bioconversion based on in vivo studies. The main active metabolite of the drug is the N-desmethylated derivative of ivabradine.
Absorption and bioavailability
Ivabradine is quickly and almost completely absorbed from the gastrointestinal tract after oral administration. The maximum concentration (Cmax) in the blood plasma is reached approximately 1 hour after ingestion on an empty stomach. Bioavailability is approximately 40%, which is due to the “first pass” effect through the liver.
Eating increases the absorption time by approximately 1 hour and increases the plasma concentration from 20% to 30%. To reduce the variability of concentration, it is recommended to take the drug simultaneously with food (see section “Method of administration and dosage”).
Distribution
The binding to plasma proteins is approximately 70%. The volume of distribution at equilibrium is about 100 liters. Cmax in blood plasma after long-term use at the recommended dose of 5 mg 2 times a day is approximately 22 ng/ml (coefficient of variation = 29%). The average equilibrium concentration in blood plasma is 10 ng/ml (coefficient of variation = 38%).
Metabolism Ivabradine is largely metabolized in the liver and intestines by oxidation involving only cytochrome P450 3A4 (CYP3A4 isoenzyme). The main active metabolite is the N-desmethylated derivative (S 18982), which accounts for 40% of the dose concentration of ivabradine. Metabolism of the active metabolite ivabradine also occurs in the presence of the CYP3A4 isoenzyme. Ivabradine has low affinity for the CYP3A4 isoenzyme and does not induce or inhibit it. In this regard, it is unlikely that ivabradine affects the metabolism or concentration of CYP3A4 isoenzyme substrates in blood plasma. On the other hand, simultaneous use of potent inhibitors or inducers of cytochrome P450 can significantly affect the concentration of ivabradine in the blood plasma (see sections “Interaction with other drugs” and “Special instructions”).
Removal
The half-life (T1/2) of ivabradine is, on average, 2 hours (70-75% of the area under the concentration-time curve (AUC)), the effective T1/2 is 11 hours. Total clearance is approximately 400 ml/min, renal clearance is approximately 70 ml/min. Metabolites are excreted at the same rate through the kidneys and intestines. About 4% of the dose taken is excreted unchanged by the kidneys.
Linearity and nonlinearity
The pharmacokinetics of ivabradine is linear over the dose range from 0.5 to 24 mg.
Special instructions
Special instructions
Heart rhythm disturbances
Coraxan is not effective for the treatment or prevention of arrhythmias. Its effectiveness decreases against the background of the development of tachyarrhythmia (for example, ventricular or supraventricular tachycardia). The drug is not recommended for patients with atrial fibrillation (atrial fibrillation) or other types of arrhythmias associated with sinus node function.
During therapy, patients should be clinically monitored for atrial fibrillation (paroxysmal or permanent). For clinical indications (for example, worsening of angina, the appearance of palpitations, irregular heart rhythm), an ECG should be included in routine monitoring.
Use in patients with bradycardia
Coraxan is contraindicated if, before starting therapy, the resting heart rate is less than 60 beats/min. If during therapy the resting heart rate decreases to values less than 50 beats/min, or the patient experiences symptoms associated with bradycardia (such as dizziness, fatigue or hypotension), it is necessary to reduce the dose of the drug. If, when the dose of the drug is reduced, the heart rate remains less than 50 beats/min, or symptoms associated with bradycardia persist, then taking the drug Coraxan should be stopped.
Combined use as part of antianginal therapy
The use of Coraxan in combination with BMCCs that reduce heart rate, such as verapamil or diltiazem, is not recommended. With the combined use of ivabradine with nitrates and BMCA derivatives of the dihydropyridine series, such as amlodipine, no changes in the safety profile of the therapy were noted. It has not been established that combined use with BMCC increases the effectiveness of ivabradine.
Stroke
It is not recommended to prescribe the drug immediately after a stroke, because There are no data on the use of the drug during this period.
Functions of visual perception
Coraxan affects the function of the retina. Currently, no toxic effects of ivabradine on the retina have been identified, but the effect of the drug on the retina with long-term use (over 1 year) is currently unknown. If visual impairments that are not described in these instructions occur, you should consider stopping taking the drug Coraxan?. Patients with retinitis pigmentosa should take Coraxan with caution.
Excipients
The drug contains lactose, so Coraxan is not recommended for patients with lactase deficiency, lactose intolerance, or glucose-galactose malabsorption syndrome.
Arterial hypotension
Due to insufficient clinical data, the drug should be prescribed with caution to patients with arterial hypotension.
Coraxan is contraindicated in severe arterial hypotension (systolic blood pressure less than 90 mm Hg and diastolic blood pressure less than 50 mm Hg).
Atrial fibrillation (atrial fibrillation) – cardiac arrhythmias
There is no proven increase in the risk of developing severe bradycardia while taking the drug Coraxan when restoring sinus rhythm during pharmacological cardioversion. However, due to the lack of sufficient data, if it is possible to delay electrical cardioversion, Coraxan should be discontinued 24 hours before it is performed.
Use in patients with congenital long QT syndrome or patients taking drugs that prolong the QT interval
Coraxan should not be prescribed for congenital long QT syndrome, or in combination with drugs that prolong the QT interval. If such therapy is necessary, strict ECG monitoring is necessary.
Moderate liver failure
In case of moderately severe liver failure (less than 9 points on the Child-Pugh scale), therapy with Coraxan should be carried out with caution.
Severe renal failure
In case of severe renal failure (creatinine clearance less than 15 ml/min), therapy with Coraxan should be carried out with caution.
Active ingredient
Active ingredient
Ivabradin
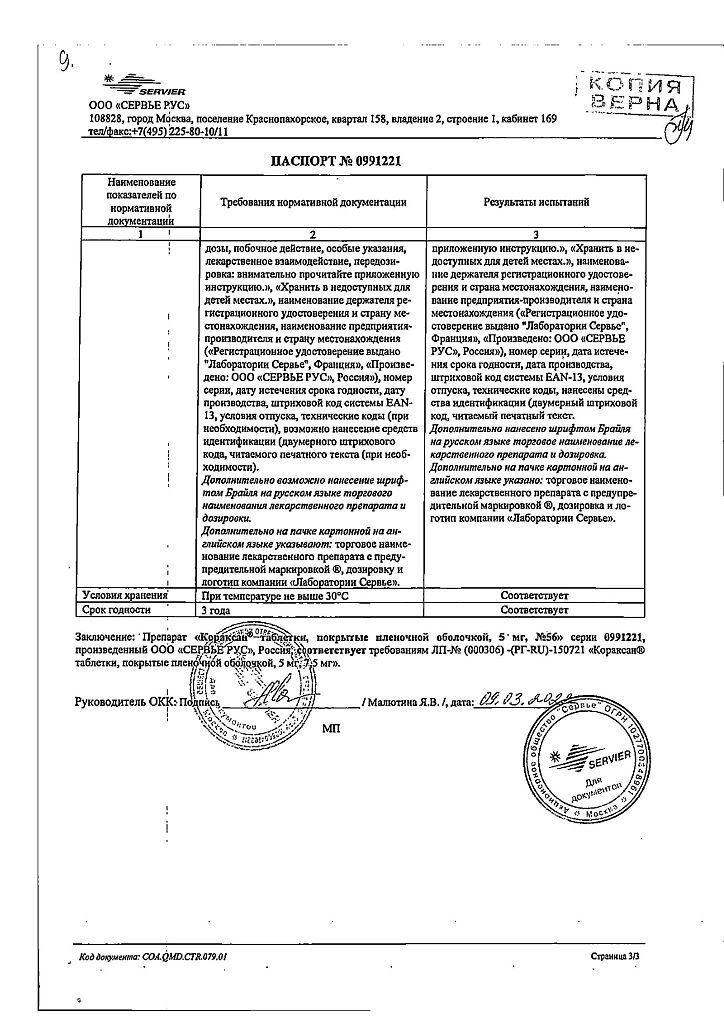
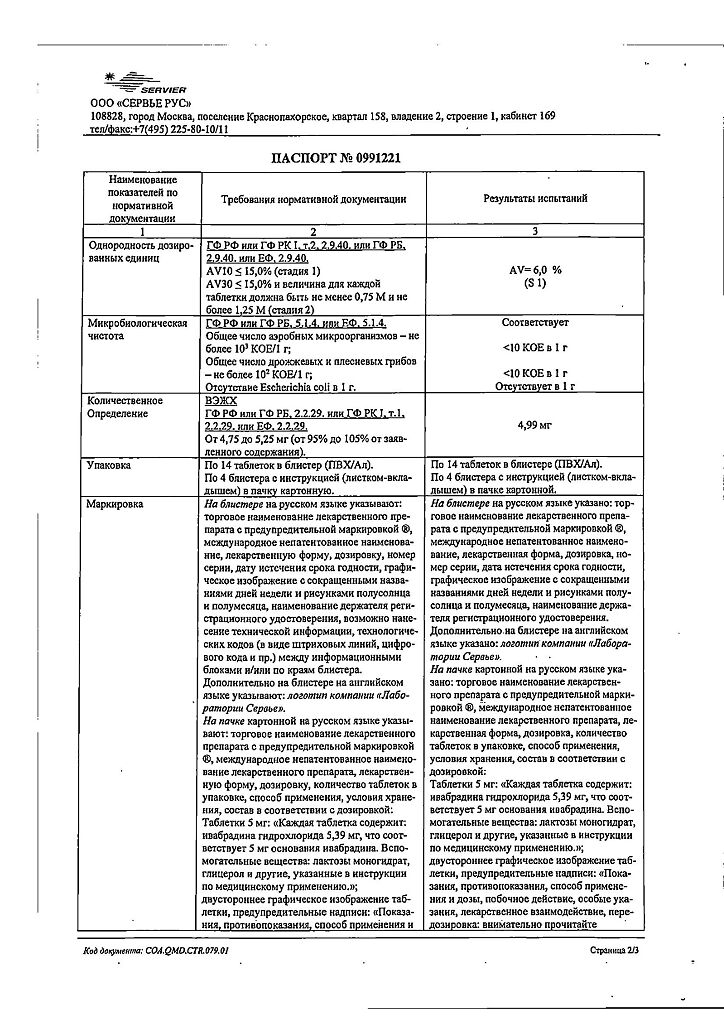
Composition
Composition
1 tablet of 5 mg contains:
Active substance:
ivabradine hydrochloride 5.39 mg, corresponding to 5.0 mg base.
Excipients:
lactose monohydrate 63.91 mg,
magnesium stearate 0.5 mg,
corn starch 20 mg,
maltodextrin 10 mg,
colloidal silicon dioxide anhydrous 0.20 mg.
Shell:
glycerol 0.08740 mg,
hypromellose 1.45276 mg,
iron dye yellow oxide (E172) 0.01457 mg,
iron oxide red dye (E172) 0.00485 mg,
macrogol 6000 0.09276 mg,
magnesium stearate 0.08740 mg,
titanium dioxide (E171) 0.26026 mg.
Pregnancy
Pregnancy
The drug Coraxan is contraindicated for use during pregnancy. Currently, there is insufficient data on the use of the drug during pregnancy. Preclinical studies of ivabradine revealed embryotoxic and teratogenic effects.
The use of Coraxan during breastfeeding is contraindicated. There is no information on the penetration of ivabradine into breast milk.
Contraindications
Contraindications
Hypersensitivity to ivabradine or any of the excipients of Coraxan;
Bradycardia (heart rate at rest less than 60 beats/min (before treatment));
cardiogenic shock;
acute myocardial infarction;
severe arterial hypotension (systolic blood pressure less than 90 mm Hg and diastolic blood pressure less than 50 mm Hg);
severe liver failure (more than 9 points on the Child-Pugh scale);
sick sinus syndrome;
sinoatrial block;
presence of an artificial pacemaker;
unstable angina;
atrioventricular (AV) block of the third degree;
simultaneous use with powerful inhibitors of isoenzymes of the cytochrome P450 3A4 system, such as antifungals of the azole group (ketoconazole, itraconazole), antibiotics of the macrolide group (clarithromycin, erythromycin for oral administration, josamycin, telithromycin), HIV protease inhibitors (nelfinavir, ritonavir) and nefazodone;
pregnancy and lactation;
age under 18 years (the effectiveness and safety of the drug in this age group has not been studied);
lactase deficiency, lactose intolerance, glucose-galactose malabsorption syndrome.
With caution:
Moderate liver failure (less than 9 points on the Child-Pugh scale); severe renal failure (creatinine clearance less than 15 ml/min); congenital prolongation of the QT interval (see section “Interaction with other drugs); simultaneous use of drugs that prolong the QT interval; simultaneous use of moderate inhibitors of cytochrome CYP3A4 isoenzymes and grapefruit juice; asymptomatic left ventricular dysfunction; atrioventricular block of the second degree; recent stroke; pigmentary degeneration of the retina (retinitis pigmentosa); arterial hypotension; simultaneous use with slow calcium channel blockers (SCBCs) that reduce heart rate, such as verapamil or diltiazem.
Side Effects
Side Effects
From the side of the organ of vision:
Very common: changes in light perception (photopsia): observed in 14.5% of patients and described as a transient change in brightness in a limited area of the visual field. As a rule, such phenomena were provoked by a sharp change in the intensity of illumination in the visual field. Basically, photopsia appeared in the first two months of treatment with subsequent recurrence. The severity of photopsia was usually mild or moderate. The appearance of photopsia stopped while therapy was continued (in 77.5% of cases) or after its completion. In less than 1% of patients, the appearance of photopsia was the reason for refusal of treatment.
Common: blurred vision.
From the cardiovascular system:
Often: bradycardia: in 3.3% of patients, especially in the first 2-3 months of therapy, in 0.5% of patients severe bradycardia developed with a heart rate of no more than 40 beats/min; AV block of the first degree; ventricular extrasystole.
Uncommon: palpitations, supraventricular extrasystole.
Unspecified frequency: hypotension, possibly associated with bradycardia
The following adverse events identified in clinical studies occurred with equal frequency in both the group of patients receiving ivabradine and in the control group, which suggests that they are related to the disease itself and not to the use of ivabradine: sinus arrhythmia; angina pectoris, including unstable; atrial fibrillation; myocardial ischemia; myocardial infarction and ventricular tachycardia.
From the digestive system: uncommon: nausea, constipation, diarrhea.
From the central nervous system:
Often: headache, especially in the first month of therapy; dizziness, possibly associated with bradycardia.
Uncommon: shortness of breath, vertigo, muscle spasms.
Unspecified frequency: syncope, possibly associated with bradycardia.
Laboratory indicators: uncommon: hyperuricemia, eosinophilia, increased plasma creatinine concentration.
From the skin and subcutaneous fat: skin rash, itching, erythema, angioedema, urticaria.
General disorders and symptoms: asthenia, fatigue, malaise, possibly associated with bradycardia.
Interaction
Interaction
Pharmacodynamic interaction
Not recommended combinations
Drugs that prolong the QT interval (for example, quinidine, disopyramide, bepridil, sotalol, ibutilide, amiodarone).
Drugs that prolong the QT interval, not related to cardiovascular drugs (for example, pimozide, ziprasidone, sertindole, mefloquine, halofantrine, pentamidine, cisapride, erythromycin IV).
Concomitant use with drugs that prolong the QT interval may increase the decrease in heart rate, so careful cardiac monitoring should be performed if coadministration is necessary.
Pharmacokinetic interaction
Cytochrome P4503A4 (CYP3A4). Ivabradine is metabolized in the liver by enzymes of the cytochrome P450 (CYP3A4) system and is a very weak inhibitor of this cytochrome. Ivabradine does not have a significant effect on the metabolism and plasma concentrations of other cytochrome CYP3A4 substrates. At the same time, CYP3A4 inhibitors and inducers interact with ivabradine and affect its metabolism and pharmacokinetic properties. It was found that inhibitors of cytochrome CYP3A4 increase, and inducers of cytochrome CYP3A4 decrease, plasma concentrations of ivabradine. An increase in the concentration of ivabradine in the blood plasma increases the risk of developing severe bradycardia.
Contraindicated combinations
Concomitant use with strong cytochrome P450 inhibitors, such as azole antifungals (ketoconazole, itraconazole), macrolide antibiotics (clarithromycin, oral erythromycin, josamycin, telithromycin), HIV protease inhibitors (nelfinavir, ritonavir) and nefazodone, ketoconazole (at a dose of 200 mg 1 time per day) or josamycin (at a dose of 1 g 2 times a day), increase the average concentration of ivabradine in the blood plasma by 7–8 times.
Not recommended combinations
Moderate CYP3A4 inhibitors. The combined use of ivabradine and drugs that reduce heart rate – diltiazem or verapamil, was well tolerated by patients and was accompanied by an increase in ivabradine concentration by 2-3 times, with an additional decrease in heart rate of approximately 5 beats/min.
This combination is not recommended.
Combinations requiring caution when using
Moderate CYP3A4 inhibitors. Concomitant use of ivabradine with other CYP3A4 inhibitors (eg fluconazole) should begin with an initial dose of 2.5 mg 2 times a day. When heart rate is less than 60 beats/min, careful monitoring of heart rate is necessary.
Grapefruit juice. When taking grapefruit juice, there was a 2-fold increase in the concentration of ivabradine in the blood. During ivabradine therapy, grapefruit juice intake should be kept to a minimum.
Inducers of CYP3A4, such as rifampicin, barbiturates, phenytoin and herbal preparations containing St. John’s wort (Hypericum perforatum), when used together, may lead to a decrease in the blood concentration and activity of ivabradine and require the selection of a higher dose of ivabradine. During therapy with ivabradine, the use of drugs and products containing St. John’s wort should be kept to a minimum.
Combined use with other drugs
The absence of a clinically significant effect on the pharmacodynamics and pharmacokinetics of ivabradine for the following drugs was demonstrated: proton pump inhibitors (omeprazole, lansoprazole), phosphodiesterase-5 inhibitors (sildenafil), HMG-CoA reductase inhibitors (simvastatin), CCB derivatives of the dihydropyridine series (amlodipine, lacidipine), digoxin and warfarin.
It has been shown that ivabradine does not have a clinically significant effect on the pharmacokinetics of simvastatin, amlodipine, lacidipine, the pharmacokinetics and pharmacodynamics of digoxin, warfarin and the pharmacodynamics of acetylsalicylic acid.
In a phase III pilot study, the use of the following drugs did not have special restrictions, and therefore they can be prescribed in combination with ivabradine without special precautions: ACE inhibitors, angiotensin II receptor antagonists, diuretics, short- and long-acting nitrates, HMG-CoA reductase inhibitors, fibrates, proton pump inhibitors, oral hypoglycemic agents, acetylsalicylic acid acid and other antithrombotic agents.
Overdose
Overdose
Symptoms: severe and prolonged bradycardia.
Treatment of severe bradycardia should be symptomatic and carried out in specialized departments. In case of development of bradycardia in combination with hemodynamic disturbances, symptomatic treatment with intravenous administration of beta-adrenergic agonists, such as isoprenaline, is indicated.
If necessary, an artificial pacemaker can be installed.
Storage conditions
Storage conditions
No special storage conditions required
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Servier Rus LLC, Russia
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | No special storage conditions required |
| Manufacturer | Servier Rus LLC, Russia |
| Medication form | pills |
| Brand | Servier Rus LLC |
Related products
Buy Coraxan, 5 mg 56 pcs with delivery to USA, UK, Europe and over 120 other countries.