No products in the cart.
Convullex, 300 mg 50 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmgroup:
antiepileptic drug
Pharmic action:
Convulex is an antiepileptic drug.
It also has central myorelaxant and sedative effects.
The mechanism of action is caused mainly by increase of GABA content in CNS due to inhibition of GABA-transferase enzyme. GABA decreases excitability and seizure readiness of motor areas of the brain. In addition, a significant role in the mechanism of action of the drug is played by the effect of valproic acid on GABA receptors (activation of GABA-ergic transmission) as well as the effect on potential-dependent sodium channels.
Another hypothesis is that it acts on post-synaptic receptor sites to mimic or enhance the inhibitory effect of GABA. A possible direct effect on membrane activity is associated with changes in conductivity for potassium ions.
Improves the mental state and mood of patients, has antiarrhythmic activity.
Pharmacokinetics:
Absorption
Valproic acid is almost completely absorbed from the GI tract, bioavailability when ingested is 100%. Food intake does not reduce the absorption rate. Cmax in blood plasma after taking tablets of prolonged action is reached after 4 hours, Cmax in blood plasma after oral drops – after 1-3 hours. The therapeutic plasma concentration of valproic acid is 50-150 mg/l.
The prolonged form is characterized by slow absorption, lower (by 25%) but more stable plasma concentrations between 4 and 14 h.
Distribution
Css is reached on days 2-4 of treatment, depending on dosage intervals.
At plasma concentrations up to 50 mg/L, the binding of valproic acid to plasma proteins is 90-95%; at concentrations of 50-100 mg/L, 80-85%.
The values of the concentration in the cerebrospinal fluid correlate with the value of the non-protein-bound fraction of the active substance. Valproic acid penetrates the placental barrier and is excreted with breast milk. The concentration in breast milk is 1-10% of the concentration in maternal plasma.
Metabolism
Valproic acid undergoes glucuronidation and oxidation in the liver. Valproic acid (1-3% of dose) and its metabolites are excreted by the kidneys, small amounts are excreted in the feces and exhaled air. T1/2 of valproic acid in monotherapy and in healthy volunteers is 8-20 hours.
Pharmacokinetics in special clinical cases
In uremia, hypoproteinemia and cirrhosis the binding of valproic acid to plasma proteins is reduced.
In combination with other medicinal agents T1/2 may be 6-8 h due to induction of metabolic enzymes.
In patients with impaired liver function, elderly patients and children under 18 months of age a significant increase in T1/2 is possible.
Indications
Indications
— epilepsy of various etiologies (idiopathic, cryptogenic and symptomatic);
– generalized epileptic seizures in adults and children (clonic, tonic, tonic-clonic, absence seizures, myoclonic, atonic);
– partial epileptic seizures in adults and children (with or without secondary generalization);
– specific syndromes (West, Lennox-Gastaut);
— behavioral disorders caused by epilepsy;
– febrile convulsions in children, childhood tics;
– treatment and prevention of bipolar affective disorders (for oral drops);
– treatment and prevention of bipolar affective disorders resistant to treatment with lithium or other drugs (for extended-release tablets).
Pharmacological effect
Pharmacological effect
Pharmgroup:
antiepileptic drug
Pharmaceutical action:
Konvulex is an antiepileptic drug.
It also has a central muscle relaxant and sedative effect.
The mechanism of action is primarily due to an increase in GABA content in the central nervous system due to inhibition of the GABA transferase enzyme. GABA reduces the excitability and convulsive readiness of the motor areas of the brain. In addition, in the mechanism of action of the drug, a significant role is played by the effect of valproic acid on GABAA receptors (activation of GABA-ergic transmission), as well as the effect on voltage-dependent sodium channels.
According to another hypothesis, it acts on postsynaptic receptor sites, simulating or enhancing the inhibitory effect of GABA. A possible direct effect on membrane activity is associated with changes in conductivity for potassium ions.
Improves the mental state and mood of patients, has antiarrhythmic activity.
Pharmacokinetics:
Suction
Valproic acid is almost completely absorbed from the gastrointestinal tract, bioavailability when taken orally is 100%. Eating does not reduce the rate of absorption. Cmax in blood plasma after taking extended-release tablets is achieved after 4 hours, Cmax in blood plasma after taking oral drops is achieved after 1-3 hours. The therapeutic concentration of valproic acid in blood plasma is 50-150 mg/l.
The prolonged form is characterized by slow absorption, lower (25%), but more stable plasma concentrations between 4 and 14 hours.
Distribution
Css is achieved on days 2-4 of treatment, depending on the intervals between doses.
At a concentration in blood plasma of up to 50 mg/l, the binding of valproic acid to plasma proteins is 90-95%, at a concentration of 50-100 mg/l – 80-85%.
Concentration values in the cerebrospinal fluid correlate with the value of the non-protein-bound fraction of the active substance. Valproic acid penetrates the placental barrier and is excreted in breast milk. The concentration in breast milk is 1-10% of the concentration in maternal plasma.
Metabolism
Valproic acid undergoes glucuronidation and oxidation in the liver.
Removal
Valproic acid (1-3% of the dose) and its metabolites are excreted by the kidneys, small amounts – with feces and exhaled air. T1/2 of valproic acid in monotherapy and in healthy volunteers is 8-20 hours.
Pharmacokinetics in special clinical situations
With uremia, hypoproteinemia and cirrhosis, the binding of valproic acid to plasma proteins decreases.
When combined with other drugs, T1/2 may be 6-8 hours due to the induction of metabolic enzymes.
In patients with impaired liver function, elderly patients and children under 18 months of age, a significant increase in T1/2 is possible.
Special instructions
Special instructions
Due to reports of severe and fatal cases of liver failure and pancreatitis when using valproic acid preparations, the following should be kept in mind:
– a high-risk group includes infants and children under 3 years of age with severe epilepsy, often associated with brain damage and congenital metabolic or degenerative diseases;
– in most cases, liver dysfunction developed in the first 6 months (usually between 2 and 12 weeks) of treatment, more often with combined antiepileptic treatment;
— cases of pancreatitis were observed regardless of the patient’s age and duration of treatment, although the risk of developing pancreatitis decreased with the patient’s age;
— insufficiency of liver function in pancreatitis increases the risk of death;
— early diagnosis (before the icteric stage) is based mainly on clinical observation – identification of early symptoms such as asthenia, anorexia, extreme fatigue, drowsiness, sometimes accompanied by vomiting and abdominal pain; in this case, a relapse of epileptic seizures may occur against the background of unchanged antiepileptic therapy.
In such cases, you should immediately consult a doctor for a clinical examination and liver function test.
During treatment, especially in the first 6 months, it is necessary to periodically check liver function – the activity of liver transaminases, the level of prothrombin, fibrinogen, coagulation factors, bilirubin concentration, as well as amylase activity (every 3 months, especially when combined with other antiepileptic drugs) and the picture of peripheral blood, in particular, blood platelets.
In patients receiving other antiepileptic drugs, transfer to valproic acid should be carried out gradually, reaching a clinically effective dose after 2 weeks, after which gradual withdrawal of other antiepileptic drugs is possible. In patients not treated with other antiepileptic drugs, a clinically effective dose should be achieved after 1 week.
The risk of side effects from the liver is increased during combination anticonvulsant therapy, as well as in children. Drinks containing ethanol are not allowed.
Before surgery, a general blood test (including platelet count), determination of bleeding time, and coagulogram parameters are required.
If symptoms of an “acute” abdomen occur during treatment, before surgery, it is recommended to determine the activity of amylase in the blood to exclude acute pancreatitis.
During treatment, one should take into account the possible distortion of the results of urine tests in diabetes mellitus (due to an increase in the content of ketone bodies) and indicators of thyroid function.
If any acute serious side effects develop, you should immediately discuss with your doctor the advisability of continuing or stopping treatment.
To reduce the risk of developing dyspeptic disorders, it is possible to take antispasmodics and enveloping agents.
Abruptly stopping taking Convulex may lead to an increase in epileptic seizures.
Impact on the ability to drive vehicles and operate machinery
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Valproic acid
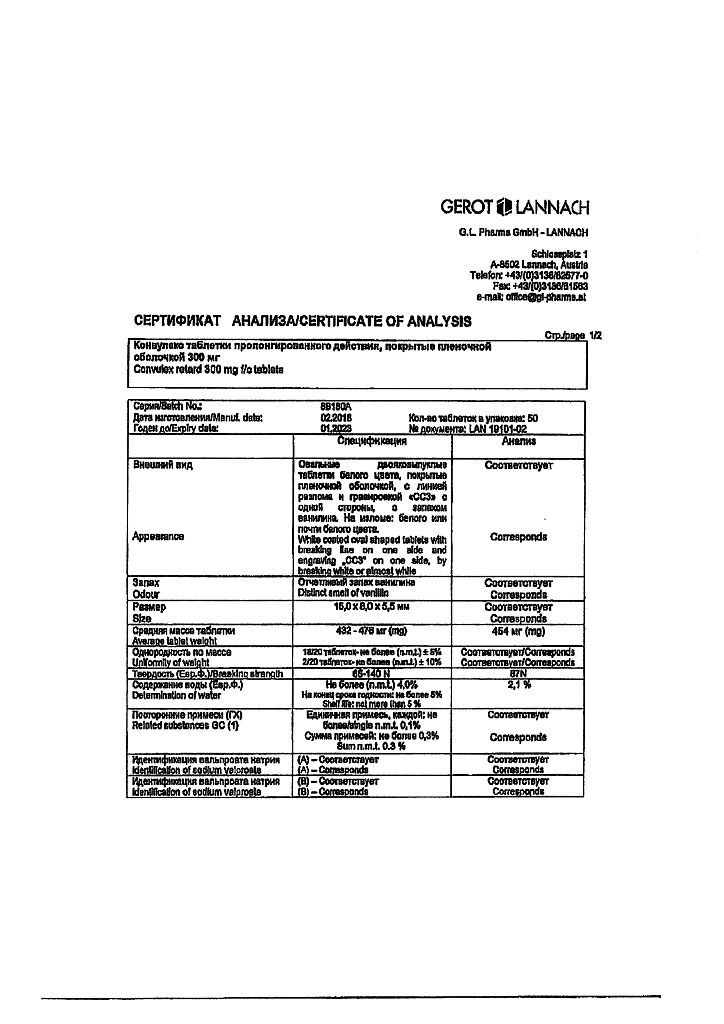
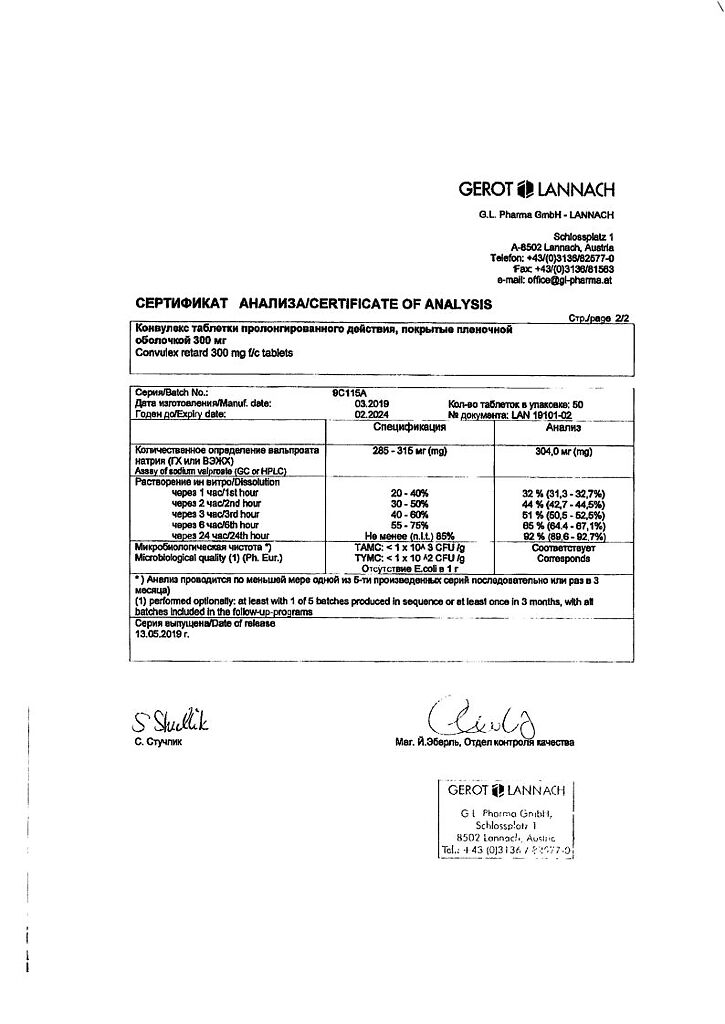
Composition
Composition
1 tab.:
– sodium valproate 300 mg.
Excipients:
citric acid,
ethylcellulose,
methyl methacrylate copolymer,
trimethylammonioethyl methacrylate chloride and ethyl acrylate (1:2:0.1) (eudragit RS30D),
purified talc,
colloidal silicon anhydrous,
magnesium stearate.
Contraindications
Contraindications
– liver failure;
– acute and chronic hepatitis;
– dysfunction of the pancreas;
– porphyria;
– hemorrhagic diathesis;
– severe thrombocytopenia;
— disorders of urea metabolism (including family history);
– combination with mefloquine, St. John’s wort, lamotrigine;
– lactation period;
– children weighing less than 7.5 kg (for oral drops);
– children weighing less than 20 kg (for extended-release tablets);
– children under 3 years of age (for extended-release tablets);
– hypersensitivity to valproic acid and its salts or components of the drug Convulex.
With caution:
– with anamnestic data on diseases of the liver and pancreas (including family history);
– with suppression of bone marrow hematopoiesis (leukopenia, thrombocytopenia, anemia);
— in case of renal failure;
— for congenital enzymopathies;
– for organic diseases of the brain;
— with hypoproteinemia;
— during pregnancy (especially the first trimester);
– children with mental retardation;
– children weighing more than 7.5 kg (for oral drops).
Side Effects
Side Effects
In general, Konvulex® is well tolerated by patients. Side effects are possible mainly when the drug concentration in plasma is above 100 mg/l or during combination therapy.
From the digestive system: nausea, vomiting, gastralgia, decreased or increased appetite, diarrhea, hepatitis, constipation, pancreatitis, up to severe injuries with a fatal outcome (in the first 6 months of treatment, more often for 2-12 weeks).
From the side of the central nervous system: tremor, diplopia, nystagmus, flashing “floaters” before the eyes, changes in behavior, mood or mental state (depression, feeling tired, hallucinations, aggressiveness, hyperactive state, psychosis, unusual agitation, restlessness or irritability), ataxia, dizziness, drowsiness, headache, encephalopathy, dysarthria, enuresis, stupor, impaired consciousness, coma
From the hematopoietic system: anemia, leukopenia, thrombocytopenia, decreased fibrinogen content and platelet aggregation, leading to the development of hypocoagulation (accompanied by prolongation of bleeding time, petechial hemorrhages, bruises, hematomas, bleeding).
From the metabolic side: decrease or increase in body weight.
From the endocrine system: dysmenorrhea, secondary amenorrhea, breast enlargement, galactorrhea.
Laboratory parameters: hypercreatininemia, hyperammonemia, hyperbilirubinemia, slight increase in the activity of liver transaminases, LDH (dose-dependent).
Allergic reactions: skin rash, urticaria, angioedema, photosensitivity, malignant exudative erythema (Stevens-Johnson syndrome).
Other: peripheral edema, hair loss (usually restored after discontinuation of the drug).
Overdose: Symptoms: nausea, vomiting, dizziness, diarrhea, respiratory dysfunction, muscle hypotonia, hyporeflexia, miosis, coma.
Treatment: gastric lavage (no later than 10-12 hours) followed by the administration of activated charcoal, hemodialysis. Forced diuresis, maintaining vital functions.
Interaction
Interaction
– Contraindicated combinations
Mefloquine: risk of epileptic seizures due to increased metabolism of valproic acid and a decrease in its plasma concentration and, on the other hand, the convulsant effect of mefloquine.
St. John’s wort: risk of decreased plasma valproic acid concentration.
– Not recommended combinations
Lamotrigine: increased risk of severe skin reactions (toxic epidermal necrolysis). Valproic acid inhibits microsomal liver enzymes that ensure the metabolism of lamotrigine, which slows down its T1/2 to 70 hours in adults and up to 45-55 hours in children and increases plasma concentrations. If combination is necessary, careful clinical and laboratory monitoring is required.
– Combinations requiring special precautions
Carbamazepine: Valproic acid increases the plasma concentration of the active metabolite of carbamazepine to the point of signs of overdose. In addition, carbamazepine enhances the hepatic metabolism of valproic acid and reduces its concentration. These circumstances require the attention of a doctor and determination of drug concentrations in plasma and a possible revision of their doses.
Phenobarbital, primidone: Valproic acid increases plasma concentrations of phenobarbital or primidone to the point of signs of overdose, more often in children. In turn, phenobarbital or primidone enhance the hepatic metabolism of valproic acid and reduce its concentration. Clinical observation is recommended during the first 2 weeks of combination treatment with an immediate reduction in the dose of phenobarbital or primidone when signs of sedation appear, and determination of the level of anticonvulsants in the blood.
Phenytoin: changes in the concentration of phenytoin in plasma are possible; phenytoin increases the hepatic metabolism of valproic acid and reduces its concentration. Clinical observation is recommended, determining the level of anticonvulsants in the blood, changing dosages if necessary.
Clonazepam: The addition of valproic acid to clonazepam in isolated cases may lead to an increase in the severity of absence status.
Ethosuximide: Valproic acid can either increase or decrease the serum concentrations of ethosuximide due to changes in its metabolism. Clinical observation is recommended, determining the level of anticonvulsants in the blood, changing dosages if necessary.
Topiramate: Increases the risk of hyperammonemia and encephalopathy.
Felbamate: increased plasma concentrations of valproic acid by 35-50%, with risk of overdose. Clinical observation, determination of the level of valproic acid in the blood, and changes in the dosage of valproic acid when combined with felbamate and after its discontinuation are recommended.
Neuroleptics, MAO inhibitors, antidepressants, benzodiazepines: neuroleptics, tricyclic antidepressants, MAO inhibitors, which lower the seizure threshold, reduce the effectiveness of the drug. In turn, valproic acid potentiates the effect of these psychotropic drugs, as well as benzodiazepines.
Cimetidine, erythromycin: suppress the hepatic metabolism of valproic acid and increase its plasma concentration.
Zidovudine: Valproic acid increases the plasma concentration of zidovudine, leading to increased toxicity.
Carbapenems, monobactams: meropenem, panipenem, as well as aztreonam and imipenem reduce the concentration of valproic acid in plasma, which may lead to a decrease in the anticonvulsant effect.
– Combinations to take into account
Acetylsalicylic acid: increased effects of valproic acid due to its displacement from plasma proteins. Valproic acid enhances the effect of acetylsalicylic acid.
Indirect anticoagulants: valproic acid enhances the effect of indirect anticoagulants; careful monitoring of the prothrombin index is necessary when administered together with vitamin K-dependent anticoagulants.
Nimodipine: increased hypotensive effect of nimodipine due to an increase in its concentration in plasma due to the suppression of its metabolism by valproic acid.
Myelotoxic drugs: increased risk of bone marrow hematopoiesis suppression.
Ethanol and hepatotoxic drugs: increase the likelihood of developing liver damage.
– Other combinations
Oral contraceptives: valproic acid does not induce liver microsomal enzymes and does not reduce the effectiveness of hormonal oral contraceptives.
Manufacturer
Manufacturer
G.L.Pharma GmbH, Austria
Additional information
| Manufacturer | G.L. Pharma GmbH, Austria |
|---|---|
| Medication form | sustained release tablets |
| Brand | G.L. Pharma GmbH |
Other forms…
Related products
Buy Convullex, 300 mg 50 pcs with delivery to USA, UK, Europe and over 120 other countries.