No products in the cart.
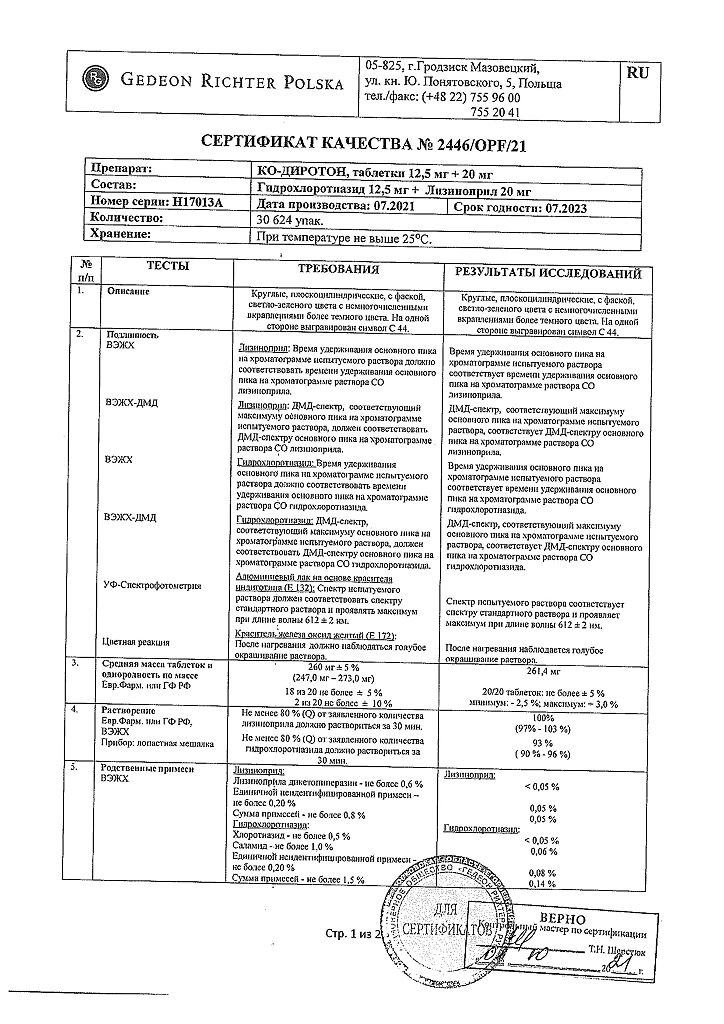
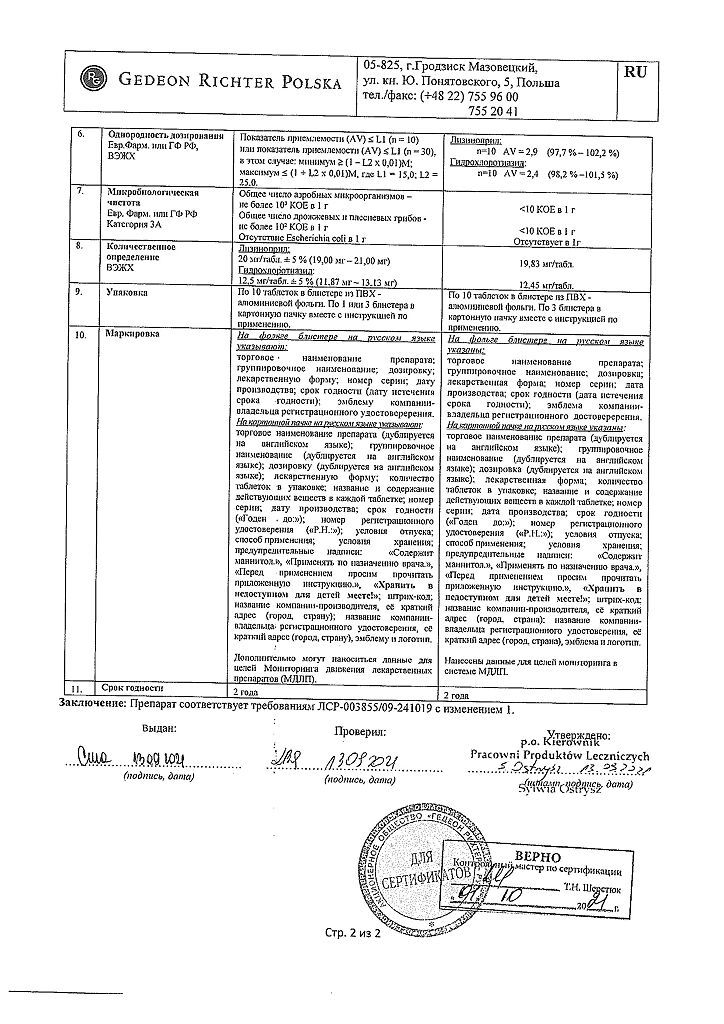
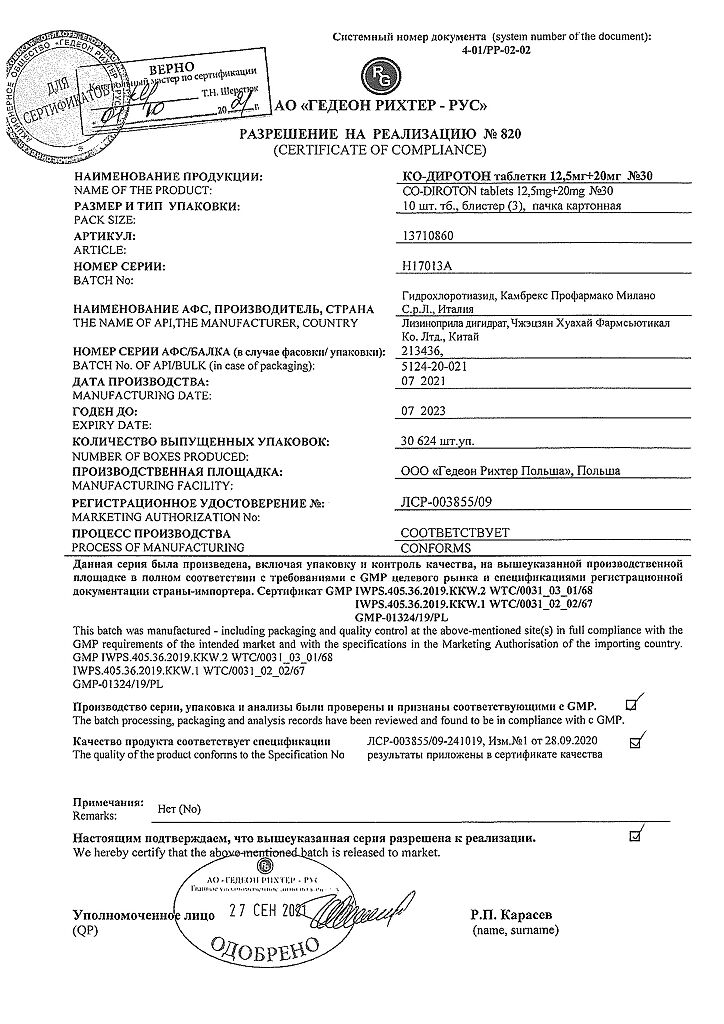
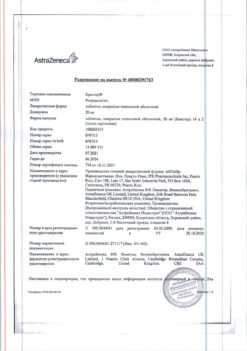
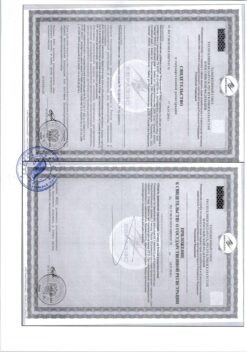
Co-Diroton, tablets 20 mg+12, 5 mg 30 pcs.
€26.15 €22.67
Description
Arterial hypertension (in patients who are indicated for combination therapy).
Indications
Indications
Arterial hypertension (in patients for whom combination therapy is indicated).
Pharmacological effect
Pharmacological effect
Co-Diroton has antihypertensive and diuretic effects.
Special instructions
Special instructions
Most often, a pronounced decrease in blood pressure occurs with a decrease in fluid volume caused by diuretic therapy, reducing the amount of salt in food, dialysis, diarrhea or vomiting.
In patients with chronic heart failure with or without simultaneous renal failure, a pronounced decrease in blood pressure is possible. It is more often detected in patients with severe chronic heart failure, as a result of the use of large doses of diuretics, hyponatremia or impaired renal function. In such patients, treatment should be started under the strict supervision of a physician. Similar rules must be followed when prescribing to patients with coronary artery disease or cerebrovascular insufficiency, in whom a sharp decrease in blood pressure can lead to myocardial infarction or stroke.
Transient arterial hypotension is not a contraindication for further use of the drug.
Before starting treatment, if possible, the sodium concentration should be normalized and/or the lost volume of fluid should be replenished, and the effect of the initial dose of the drug on the patient should be carefully monitored.
In patients with chronic heart failure, a pronounced decrease in blood pressure after initiation of treatment with ACE inhibitors may lead to further deterioration of renal function. Cases of acute renal failure have been reported.
In patients with bilateral renal artery stenosis or stenosis of the artery of a solitary kidney who received ACE inhibitors, there was an increase in serum urea and creatinine, usually reversible after discontinuation of treatment. It was more common in patients with renal failure.
Angioedema of the face, extremities, lips, tongue, epiglottis and/or larynx has been reported rarely in patients treated with ACE inhibitors, including lisinopril, and may occur during any period of treatment. In this case, treatment with lisinopril should be stopped as soon as possible and the patient should be monitored until complete regression of symptoms. In cases where swelling of only the face and lips occurs, the condition most often goes away without treatment, however, it is possible to prescribe antihistamines. Angioedema with laryngeal edema can be fatal. When the tongue, epiglottis or larynx are involved, airway obstruction may occur, so appropriate therapy (0.3-0.5 ml of epinephrine (adrenaline) solution 1:1000 s.c.) and/or measures to ensure airway patency must be immediately carried out.
Patients who have a history of angioedema not related to previous treatment with ACE inhibitors may be at increased risk of developing it during treatment with an ACE inhibitor.
Cough has been reported when using an ACE inhibitor. The cough is dry and prolonged, which disappears after stopping treatment with an ACE inhibitor. When making a differential diagnosis of cough, cough caused by the use of an ACE inhibitor must also be taken into account.
Anaphylactic reactions have also been reported in patients undergoing hemodialysis using high-flux dialysis membranes (AN69®) who are also taking ACE inhibitors. In such cases, the use of a different type of dialysis membrane or another antihypertensive agent should be considered.
When using drugs that lower blood pressure in patients undergoing major surgery or during general anesthesia, lisinopril can block the formation of angiotensin II.
A pronounced decrease in blood pressure, which is considered a consequence of this mechanism, can be eliminated by increasing the volume of blood volume.
Before surgery (including dentistry), it is necessary to warn the anesthesiologist about the use of ACE inhibitors.
In some cases, hyperkalemia was observed. Risk factors for the development of hyperkalemia include renal failure, diabetes mellitus, and taking potassium supplements or drugs that increase potassium levels in the blood (eg, heparin), especially in patients with impaired renal function.
In patients at risk of symptomatic hypotension (those on a low-salt or salt-free diet) with or without hyponatremia, as well as in patients who have received high doses of diuretics, the above conditions must be compensated for (loss of fluid and salts) before starting treatment.
Thiazide diuretics can affect glucose tolerance, so it is necessary to adjust the dose of oral hypoglycemic agents. Thiazide diuretics may reduce renal calcium excretion and cause hypercalcemia. Severe hypercalcemia may be a symptom of latent hyperparathyroidism. It is recommended to discontinue treatment with thiazide diuretics until a test to assess parathyroid function is performed.
During treatment with the drug, regular monitoring of blood plasma potassium, glucose, urea, and lipids is necessary.
During the treatment period, it is not recommended to drink alcoholic beverages, because alcohol enhances the hypotensive effect of the drug.
Caution should be exercised when performing physical exercises in hot weather (risk of dehydration and excessive reduction in blood pressure due to a decrease in blood volume).
Impact on the ability to drive vehicles and operate machinery
During the treatment period, you should refrain from driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions, because Dizziness is possible, especially at the beginning of treatment.
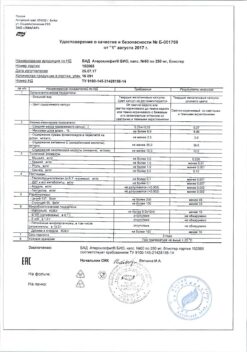
Active ingredient
Active ingredient
Hydrochlorothiazide, Lisinopril
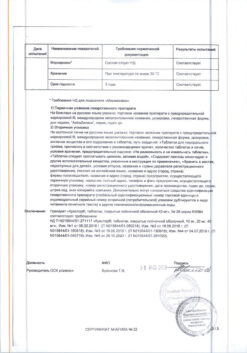
Composition
Composition
1 tablet contains lisinopril dihydrate 21.77 mg, which corresponds to the content of lisinopril 20 mg;
hydrochlorothiazide 12.5 mg.
Pregnancy
Pregnancy
The use of lisinopril during pregnancy is contraindicated. If pregnancy is established, the drug should be stopped as soon as possible.
Taking ACE inhibitors in the second and third trimesters of pregnancy has an adverse effect on the fetus (a marked decrease in blood pressure, renal failure, hyperkalemia, hypoplasia of the skull bones, and intrauterine death are possible). There is no data on the negative effects of the drug on the fetus when used during the first trimester.
It is recommended to monitor newborns and infants who have been exposed to ACE inhibitors in utero for timely detection of a pronounced decrease in blood pressure, oliguria, and hyperkalemia.
During treatment with the drug, breastfeeding should be discontinued.
Contraindications
Contraindications
Hypersensitivity (including to other ACE inhibitors and sulfonamide derivatives), anuria, angioedema (including a history of the use of ACE inhibitors), hemodialysis using high-flow membranes, hypercalcemia, hyponatremia, porphyria, precoma, hepatic coma, diabetes mellitus (severe forms), pregnancy, lactation, age under 18 years (efficacy and safety have not been established).
With caution. Aortic stenosis, hypertrophic cardiomyopathy, bilateral renal artery stenosis, stenosis of the artery of a single kidney with progressive azotemia, condition after kidney transplantation, chronic renal failure (creatinine clearance more than 30 ml/min.), severe chronic renal failure (creatinine clearance less than 30 ml/min), primary hyperaldosteronism, arterial hypotension, bone marrow hypoplasia, hyponatremia (increased risk of developing arterial hypotension in patients on a low-salt or salt-free diet), conditions accompanied by a decrease in BCC (including diarrhea, vomiting), connective tissue diseases (SLE, scleroderma), diabetes mellitus, gout, hyperuricemia, hyperkalemia, liver failure, cerebrovascular insufficiency, severe CHF, old age.
Side Effects
Side Effects
Frequent: dizziness, headache.
Less frequent. From the cardiovascular system: marked decrease in blood pressure, chest pain, rarely – orthostatic hypotension, tachycardia, bradycardia, the appearance of symptoms of heart failure, impaired AV conduction, myocardial infarction.
From the digestive system: nausea, vomiting, abdominal pain, dry mouth, diarrhea, dyspepsia, anorexia, taste change, pancreatitis, hepatitis (hepatocellular and cholestatic), jaundice.
From the nervous system: mood lability, impaired concentration, paresthesia, increased fatigue, drowsiness, convulsive twitching of the muscles of the limbs and lips, rarely – asthenic syndrome, confusion.
From the respiratory system: dyspnea, bronchospasm, apnea.
From the skin: urticaria, sweating, alopecia, photosensitivity.
Allergic reactions: angioedema of the face, extremities, lips, tongue, epiglottis and/or larynx, skin rash, itching, fever, vasculitis, positive results for antinuclear antibodies, increased ESR, eosinophilia.
From the hematopoietic organs: leukopenia, thrombocytopenia, neutropenia, agranulocytosis, anemia (decrease in Hb, hematocrit, erythropenia).
From the genitourinary system: uremia, oliguria/anuria, impaired renal function, acute renal failure, decreased potency.
Laboratory indicators: hyperkalemia and/or hypokalemia, hyponatremia, hypomagnesemia, hypochloremia, hypercalcemia, hyperuricemia, hyperglycemia, increased urea and creatinine in the blood plasma, rarely – increased activity of liver transaminases, hyperbilirubinemia, hypercholesterolemia, hypertriglyceridemia, decreased glucose tolerance.
Other: dry cough, arthralgia/arthritis, myalgia, impaired fetal kidney development, exacerbation of gout, vasculitis.
Interaction
Interaction
When used simultaneously with potassium-sparing diuretics (spironolactone, triamterene, amiloride), potassium preparations, salt substitutes containing potassium, the risk of developing hyperkalemia increases, especially in patients with impaired renal function. Therefore, they can be prescribed together only on the basis of an individual physician’s decision with regular monitoring of serum potassium levels and renal function.
When used simultaneously with vasodilators, barbiturates, phenothiazines, tricyclic antidepressants, and ethanol, an increased hypotensive effect is observed.
When used simultaneously with NSAIDs (indomethacin and others), estrogens, a decrease in the antihypertensive effect of lisinopril is observed.
When used simultaneously with lithium preparations, the elimination of lithium from the body slows down (increased cardiotoxic and neurotoxic effects of lithium).
When used simultaneously with antacids and cholestyramine, absorption in the gastrointestinal tract is reduced.
The drug enhances the neurotoxicity of salicylates, weakens the effect of hypoglycemic drugs for oral administration, norepinephrine, epinephrine and anti-gout drugs, enhances the effects (including side effects) of cardiac glycosides, the effect of peripheral muscle relaxants, and reduces the excretion of quinidine.
Reduces the effect of oral contraceptives.
Ethanol enhances the hypotensive effect of the drug.
When taking methyldopa simultaneously, the risk of hemolysis increases.
Overdose
Overdose
Symptoms: marked decrease in blood pressure, dry mouth, drowsiness, urinary retention, constipation, anxiety, increased irritability.
Treatment: symptomatic therapy, intravenous fluid administration, blood pressure control; therapy aimed at correcting dehydration and water-salt balance disorders. Monitoring serum urea, creatinine and electrolytes, as well as diuresis.
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Gedeon Richter Poland, Poland
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Gedeon Richter Poland, Poland |
| Medication form | pills |
| Brand | Gedeon Richter Poland |
Related products
Buy Co-Diroton, tablets 20 mg+12, 5 mg 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.