No products in the cart.
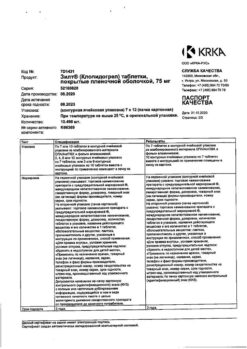
Clopidogrel, 75 mg 30 pcs
€21.02 €17.51
Description
Pharmacotherapeutic group: anti-aggregant drug
ATX code: B01AC04
Pharmacological properties
Pharmacodynamics
Clopidogrel is a prodrug, one of the active metabolites of which is an inhibitor of platelet aggregation. The active metabolite of clopidogrel selectively inhibits adenosine diphosphate (ADP) binding to the P2Y12 receptor of platelets and subsequent ADP-mediated activation of the glycoprotein IIb/IIIa complex, leading to suppression of platelet aggregation. Through irreversible binding, platelets remain immune to ADP stimulation for the remainder of their lives (approximately 7-10 days), and recovery of normal platelet function occurs at a rate consistent with the rate of platelet renewal. Platelet aggregation caused by agonists other than ADP is also inhibited by blocking enhanced platelet activation by the released ADP.
Because formation of the active metabolite occurs via cytochrome P450 system isoenzymes, some of which may be polymorphic or may be inhibited by other drugs, not all patients may adequately inhibit platelet aggregation (see subsection “Pharmacogenetics” under “Pharmacological properties”).
Clopidogrel is able to prevent the development of atherothrombosis in any localization of atherosclerotic vascular lesions, in particular in cerebral, coronary or peripheral arteries.
When clopidogrel is taken daily at a dose of 75 mg a significant suppression of ADP-induced platelet aggregation is noted from the first day of administration, which gradually increases after 3-7 days and then reaches a constant level (when equilibrium state is reached). In the equilibrium state platelet aggregation is suppressed by an average of
40-60%. Platelet aggregation and bleeding time return to baseline on average within 5 days after discontinuation of clopidogrel.
In a small study comparing the pharmacodynamic properties of clopidogrel in men and women, less inhibition of
ADP-induced platelet aggregation was observed in women, but there was no difference in prolongation of bleeding time. In the large controlled CAPRIE trial (clopidogrel versus acetylsalicylic acid (ASA) in patients at risk for ischemic events), the rates of clinical outcomes, other adverse events, and abnormal clinical and laboratory parameters were similar in both men and women.
Pharmacokinetics
Indications
Indications
Prevention of atherothrombotic complications:
· in patients with myocardial infarction (with a duration of several days to 35 days), ischemic stroke (with a duration of 7 days to 6 months) or with diagnosed occlusive peripheral artery disease.
in patients with acute coronary syndrome:
– without ST segment elevation (unstable angina or non-Q wave myocardial infarction), including patients who underwent stenting during percutaneous coronary intervention (in combination with acetylsalicylic acid);
– with ST segment elevation (acute myocardial infarction) with drug treatment and the possibility of thrombolysis (in combination with acetylsalicylic acid).
Prevention of atherothrombotic and thromboembolic complications, including stroke, in atrial fibrillation (atrial fibrillation)
Patients with atrial fibrillation (atrial fibrillation) who have at least one risk factor for the development of vascular complications cannot take indirect anticoagulants and have a low risk of bleeding (in combination with ASA).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antiplatelet agent
ATX code: B01AC04
Pharmacological properties
Pharmacodynamics
Clopidogrel is a prodrug, one of the active metabolites of which is an inhibitor of platelet aggregation. The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to the platelet P2Y12 receptor and subsequent ADP-mediated activation of the glycoprotein IIb/IIIa complex, leading to suppression of platelet aggregation. Due to irreversible binding, platelets remain immune to ADP stimulation for the remainder of their life (approximately 7-10 days), and restoration of normal platelet function occurs at a rate consistent with platelet turnover. Platelet aggregation induced by agonists other than ADP is also inhibited by blocking enhanced platelet activation by released ADP.
Since the formation of the active metabolite occurs with the help of isoenzymes of the cytochrome P450 system, some of which may differ in polymorphism or can be inhibited by other drugs, adequate inhibition of platelet aggregation is not possible in all patients (see the “Pharmacogenetics” subsection of the “Pharmacological properties” section).
Clopidogrel is able to prevent the development of atherothrombosis in any localization of atherosclerotic vascular lesions, in particular in lesions of the cerebral, coronary or peripheral arteries.
When taking clopidogrel daily at a dose of 75 mg, from the first day of administration there is a significant suppression of ADP-induced platelet aggregation, which gradually increases after 3-7 days and then reaches a constant level (when an equilibrium state is reached). At steady state, platelet aggregation is suppressed on average by
40-60%. Platelet aggregation and bleeding time return to baseline levels within an average of 5 days after discontinuation of clopidogrel.
In a small study comparing the pharmacodynamic properties of clopidogrel in men and women, less inhibition
ADP-induced platelet aggregation was observed in women, but there was no difference in prolongation of bleeding time. In the large controlled trial CAPRIE (clopidogrel versus acetylsalicylic acid (ASA) in patients at risk of ischemic events), the incidence of clinical outcomes, other adverse events and abnormal clinical laboratory parameters was similar in both men and women.
Pharmacokinetics
Special instructions
Special instructions
When treating with clopidogrel, especially during the first weeks of treatment and/or after invasive cardiac procedures/surgery, patients must be carefully monitored to exclude signs of bleeding, incl. hidden.
Due to the risk of bleeding and hematological undesirable effects (see section “Side Effects”), if clinical symptoms indicating the possibility of bleeding appear during treatment, it is urgent to do a clinical blood test, determine the activated partial thromboplastin time (aPTT), platelet count, indicators of platelet functional activity and conduct other necessary studies.
Clopidogrel, as well as other antiplatelet drugs, should be used with caution in patients who have an increased risk of bleeding associated with trauma, surgery or other pathological conditions, as well as in patients receiving ASA, NSAIDs, including COX-2 inhibitors, heparin or glycoprotein IIb/IIIa inhibitors, SSRIs and thrombolytic drugs.
The combined use of clopidogrel with warfarin may increase the intensity of bleeding (see section “Interaction with other drugs”), so caution should be exercised when using clopidogrel and warfarin together.
If the patient is undergoing elective surgery and there is no need for an antiplatelet effect, clopidogrel should be discontinued 7 days before surgery.
Clopidogrel prolongs bleeding time and should be used with caution in patients with diseases predisposing to the development of bleeding (especially gastrointestinal and intraocular). Drugs that can cause damage to the gastrointestinal mucosa (such as ASA, NSAIDs) should be used with caution in patients taking clopidogrel.
Patients should be warned that when taking clopidogrel (alone or in combination with ASA), bleeding may take longer to stop and that if they experience unusual bleeding (in location or duration) they should notify their prescriber. Before any upcoming surgery and before starting any new drug, patients should tell their doctor (including their dentist) that they are taking clopidogrel.
Very rarely, after the use of clopidogrel (sometimes even short-term), there have been cases of the development of thrombotic thrombocytopenic purpura, which is characterized by thrombocytopenia and microangiopathic hemolytic anemia, accompanied by neurological disorders, renal dysfunction and fever, and is a potentially life-threatening condition requiring immediate treatment, including plasmapheresis.
During treatment, it is necessary to monitor the functional activity of the liver. In case of severe liver damage, keep in mind the risk of developing hemorrhagic diathesis.
The drug should be prescribed with caution to patients with impaired renal function.
Taking clopidogrel is not recommended for acute stroke less than 7 days old (as there is no data on its use in this condition).
In patients with a recent history of transient cerebrovascular accident or stroke, who are at high risk of developing recurrent ischemic complications, the combination of ASA and clopidogrel increases the incidence of major bleeding. Therefore, such combination therapy should be carried out with caution and only in case of proven clinical benefit from its use.
Cases of acquired hemophilia have been reported when taking clopidogrel. With a confirmed isolated increase in aPTT, accompanied or not accompanied by the development of bleeding, the possibility of developing acquired hemophilia should be considered. Patients with a confirmed diagnosis of acquired hemophilia should be observed and treated by specialists in this disease and stop taking clopidogrel.
In patients with low activity of the CYP2C19 isoenzyme, when clopidogrel is used in recommended doses, less of the active metabolite of clopidogrel is formed and its antiplatelet effect is less pronounced, and therefore, when taking the usually recommended doses of clopidogrel in acute coronary syndrome or percutaneous coronary intervention, a higher incidence of cardiovascular complications is possible than in patients with normal isoenzyme activity CYP2C19. Tests are available to determine the CYP2C19 genotype. These tests can be used to help select a therapeutic strategy. The issue of using higher doses of clopidogrel in patients with low activity of the CYP2C19 isoenzyme is being considered (see the “Pharmacogenetics” subsection of the “Pharmacological properties” section, sections “With caution”, “Dosage and administration”).
It is necessary to clarify whether patients have a history of allergic and/or hematological reactions to other thienopyridine derivatives (ticlopidine, prasugrel), because Cases of cross allergic and/or hematological reactions between thienopyridines have been described (see section “Side effects”). Patients who have previously experienced allergic and/or hematological reactions to other thienopyridine derivatives require careful monitoring throughout the entire period of therapy to identify signs of hypersensitivity to clopidogrel.
Clopidogrel should not be taken by patients with rare hereditary galactose intolerance, lactose deficiency and glucose-galactose malabsorption syndrome.
The effect of the drug on the performance of potentially hazardous activities that require increased concentration and speed of psychomotor reactions
Clopidogrel does not have a significant effect on the abilities required to drive a car or engage in potentially hazardous activities.
Active ingredient
Active ingredient
Clopidogrel
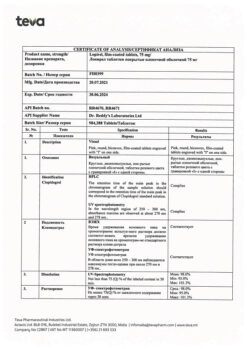
Composition
Composition
1 film-coated tablet contains:
Tablet core composition:
Active ingredient: clopidogrel hydrosulfate –
97.87 mg (in terms of clopidogrel – 75.0 mg);
Excipients: anhydrous lactose – 60.0 mg; microcrystalline cellulose – 69.93 mg; colloidal silicon dioxide –
6.0 mg; crospovidone – 12.0 mg; hyprolose – 1.2 mg; glyceryl dibehenate – 3.0 mg.
Tablet shell composition: opadry II pink (85F34610) – 8.00 mg (polyvinyl alcohol – 40%, titanium dioxide – 24.24%, macrogol 3350 – 20.2%, talc – 14.8%, yellow iron oxide – 0.37%, red iron oxide – 0.36%, black iron oxide – 0.03%).
Pregnancy
Pregnancy
Pregnancy
Animal studies have not revealed direct or indirect adverse effects on pregnancy, embryonic development, childbirth or postnatal development. Because animal studies may not always predict response in humans, and due to the lack of controlled clinical trial data on clopidogrel use in pregnant women, as a precautionary measure, clopidogrel use during pregnancy is not recommended unless, in the judgment of a physician, its use is strictly necessary.
Breastfeeding period
Studies in rats have shown that clopidogrel and/or its metabolites are excreted into breast milk. There are no data on the excretion of clopidogrel into breast milk in humans. In case of treatment with clopidogrel, breastfeeding should be discontinued.
Contraindications
Contraindications
· Hypersensitivity to clopidogrel and/or any other component of the drug;
· Severe liver failure;
· Acute bleeding, such as bleeding from a peptic ulcer or intracranial hemorrhage;
· Rare hereditary galactose intolerance, lactase deficiency and glucose-galactose malabsorption;
· Pregnancy and breastfeeding (see section “Pregnancy and breastfeeding”);
· Children under 18 years of age (safety and effectiveness of use have not been established).
With caution
· In moderate liver failure, which may predispose to bleeding (limited clinical experience with use).
· For mild to moderate chronic renal failure (limited clinical experience).
· In diseases in which there is a predisposition to the development of bleeding (especially gastrointestinal and intraocular), and in patients simultaneously taking medications that can cause damage to the mucous membrane of the gastrointestinal tract (such as ASA and nonsteroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors).
· In patients who have an increased risk of bleeding: due to trauma, surgery or other pathological conditions, as well as in patients receiving treatment with ASA, heparin, oral anticoagulants, glycoprotein IIb/IIIa inhibitors, NSAIDs, including selective COX-2 inhibitors, or selective serotonin reuptake inhibitors (SSRIs) (see section “Special Instructions”).
· If there is a history of allergic and hematological reactions to other thienopyridines (such as ticlopidine, prasugrel) due to the possibility of cross-reactions (see section “Special instructions”).
· If you have recently suffered a transient cerebrovascular accident or ischemic stroke (when used simultaneously with ASA, see section “Special Instructions”).
Side Effects
Side Effects
To assess the incidence of adverse events, the following WHO classification is used:
Very common (≥ 1/10)
Often (≥ 1/100 and < 1/10)
Uncommon (≥ 1/1000 and < 1/100)
Rare (≥ 1/10,000 and < 1/1000)
Very rare (≥ 1/10,000)
Frequency unknown (based on available data, it is not possible to determine the frequency of development of an adverse event).
From the blood and lymphatic system:
uncommon – thrombocytopenia, leukopenia, eosinophilia;
rarely – neutropenia, including severe neutropenia;
very rarely – thrombotic thrombocytopenic purpura, aplastic anemia, pancytopenia, agranulocytosis, severe thrombocytopenia, granulocytopenia, anemia;
frequency unknown – acquired hemophilia A.
From the immune system:
very rarely – anaphylactic reactions, serum sickness;
frequency unknown – cross-hypersensitivity to other thienopyridines (for example, ticlopidine, prasugrel);
From the nervous system:
uncommon – intracranial hemorrhage (several cases with fatal outcome), headache, paresthesia, dizziness;
very rarely – disturbances in taste perception.
Mental disorders:
very rarely – confusion, hallucinations.
From the side of the organ of vision:
uncommon – retinal hemorrhage, conjunctival hemorrhage, hemophthalmos.
Hearing and labyrinth disorders:
rarely – vertigo.
For the skin and subcutaneous tissues:
often – “bruises” (local subcutaneous hemorrhages);
uncommon – skin rash and itching, thrombocytopenic purpura;
very rarely – angioedema, erythematous rash, urticaria, bullous dermatitis (toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme), eczema, lichen planus, drug hypersensitivity syndrome, drug rash with eosinophilia and systemic manifestations (DRESS syndrome), exfoliative rash.
From the kidneys and urinary tract:
uncommon – hematuria;
very rarely – glomerulopathy (including glomerulonephritis), hypercreatininemia.
From the musculoskeletal and connective tissue side:
very rarely – hemorrhages in muscles and joints, arthritis, arthralgia, myalgia.
From the gastrointestinal tract:
very often – gastrointestinal bleeding, diarrhea, abdominal pain, dyspepsia;
uncommon – peptic ulcer of the stomach and duodenum, gastritis, vomiting, nausea, constipation, flatulence;
rarely – retroperitoneal hemorrhage;
very rarely – gastrointestinal bleeding and retroperitoneal hemorrhage with fatal outcome, pancreatitis, colitis (including ulcerative colitis or lymphocytic colitis), stomatitis.
From the liver and biliary tract:
very rarely – acute liver failure, hepatitis (non-infectious).
From the respiratory system, chest and mediastinal organs:
often – nosebleeds;
very rarely – bleeding from the respiratory tract (hemoptysis, pulmonary hemorrhage), interstitial pneumonitis, bronchospasm, eosinophilic pneumonia.
From the cardiovascular system:
often – hematoma;
very rarely – severe bleeding, bleeding from the surgical wound, vasculitis, decreased blood pressure.
Laboratory and instrumental data:
uncommon – prolongation of bleeding time, decrease in the number of neutrophils and/or platelets in the peripheral blood, abnormal liver function tests, increased concentration of creatinine in the blood plasma.
General disorders and disorders at the injection site:
often – bleeding from the site of vascular puncture;
very rarely – increased body temperature.
Interaction
Interaction
Oral anticoagulants: simultaneous use of clopidogrel and oral anticoagulants may increase the intensity of bleeding, and therefore the use of this combination is not recommended. Clopidogrel does not affect the pharmacokinetics of warfarin and does not change the international normalized ratio (INR) in patients taking warfarin for a long time. However, concomitant use of warfarin with clopidogrel may increase the risk of bleeding due to the independent effects of these drugs on hemostasis.
Prescribing glycoprotein IIb/IIIa inhibitors together with clopidogrel requires caution in patients with an increased risk of bleeding (in case of trauma and surgery or other pathological conditions) (see section “Special Instructions”).
Acetylsalicylic acid: ASA does not change the effect of clopidogrel, which inhibits ADP-induced platelet aggregation, but clopidogrel enhances the effect of ASA on collagen-induced platelet aggregation. However, simultaneous administration of 500 mg ASA with clopidogrel 2 times a day for 1 day did not lead to a significant increase in the bleeding time caused by taking clopidogrel. There may be a pharmacodynamic interaction between clopidogrel and ASA, which leads to an increased risk of bleeding. Therefore, caution should be exercised when using them simultaneously, although in clinical studies patients received combination therapy with clopidogrel and ASA for up to one year.
Heparin: According to a clinical study conducted in healthy volunteers, when taking clopidogrel, no change in the dose of heparin was required and its anticoagulant effect did not change. Concomitant use of heparin did not change the inhibitory effect of clopidogrel on platelet aggregation. There may be a pharmacodynamic interaction between clopidogrel and heparin, which may increase the risk of bleeding, so the simultaneous use of this combination requires caution.
Thrombolytics: The safety of concomitant use of clopidogrel, fibrin-specific or non-fibrin-specific thrombolytic drugs and heparin has been studied in patients with acute myocardial infarction. The incidence of clinically significant bleeding was similar to that observed in the case of combined use of thrombolytic agents and heparin with ASA.
Nonsteroidal anti-inflammatory drugs (NSAIDs): In a clinical study in healthy volunteers, coadministration of clopidogrel and naproxen increased occult GI blood loss. However, due to the lack of interaction studies between clopidogrel and other NSAIDs, it is currently unknown whether there is an increased risk of gastrointestinal bleeding when clopidogrel is taken with other NSAIDs. Therefore, the use of NSAIDs, including COX-2 inhibitors, in combination with clopidogrel should be used with caution.
Selective serotonin reuptake inhibitors (SSRIs): Because SSRIs impair platelet activation and increase the risk of bleeding, concomitant use of SSRIs with clopidogrel should be done with caution.
CYP2C19 inhibitors
Since clopidogrel is metabolized to its active metabolite in part by the CYP2C19 isoenzyme, the use of drugs that inhibit this isoenzyme may lead to a decrease in the level of the active metabolite of clopidogrel and a decrease in its clinical effectiveness. The clinical significance of this interaction has not been established. As a precaution, it is recommended to avoid the combined use of clopidogrel with drugs that inhibit the CYP2C19 isoenzyme (omeprazole, esomeprazole, fluvoxamine, fluoxetine, moclobemide, voriconazole, fluconazole, ticlopidine, ciprofloxacin, cimetidine, carbamazepine, oxcarbazepine, chloramphenicol).
Proton pump inhibitors
If it becomes necessary to prescribe proton pump inhibitors concomitantly with clopidogrel, the drug with the least CYP2C19 inhibition (pantoprazole or lansoprazole) should be used.
Other combination therapy
A number of clinical studies have been conducted with clopidogrel and other concomitantly administered drugs to examine possible pharmacodynamic and pharmacokinetic interactions, which have shown that:
– when clopidogrel was used together with atenolol, nifedipine, or with both drugs at the same time, no clinically significant pharmacodynamic interaction was observed;
– simultaneous use of phenobarbital, cimetidine and estrogens did not have a significant effect on the pharmacodynamics of clopidogrel;
– the pharmacokinetic parameters of digoxin and theophylline did not change when they were used together with clopidogrel;
– antacids did not reduce the absorption of clopidogrel;
– According to the results of the CAPRIE study, phenytoin and tobutamide can be safely used in combination with clopidogrel. It is unlikely that clopidogrel can affect the metabolism of other drugs such as phenytoin and tolbutamide, as well as NSAIDs that are metabolized by the CYP2C19 isoenzyme;
– in clinical studies, no clinically significant adverse interactions of clopidogrel with angiotensin-converting enzyme inhibitors, diuretics, beta-blockers, blockers of “slow” calcium channels, lipid-lowering drugs, coronary vasodilators, hypoglycemic drugs (including insulin), antiepileptic drugs, drugs for hormone replacement therapy were revealed.
Overdose
Overdose
Symptoms: increased bleeding time with subsequent complications in the form of bleeding.
Treatment: if bleeding occurs, appropriate
therapeutic measures, platelet transfusion. Specific antidote
No.
Storage conditions
Storage conditions
In a place protected from light at a temperature not exceeding 25 C.
Keep out of the reach of children.
Shelf life
Shelf life
2 years 6 months
Do not use the drug after the expiration date.
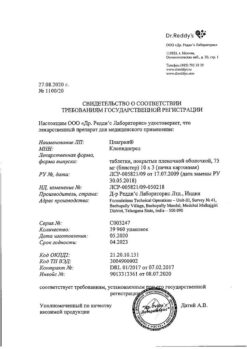
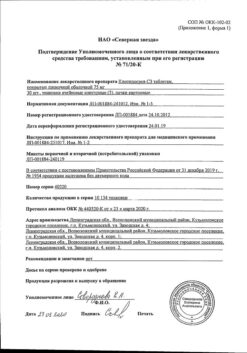
Manufacturer
Manufacturer
Izvarino Pharma, Russia
Additional information
| Shelf life | 2 years 6 months. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In the dark place at a temperature not exceeding 25 C. Store out of the reach of children. |
| Manufacturer | Izvarino Pharma, Russia |
| Medication form | pills |
| Brand | Izvarino Pharma |
Other forms…
Related products
Buy Clopidogrel, 75 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.