No products in the cart.
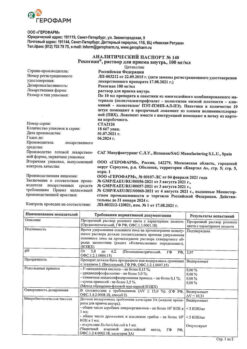
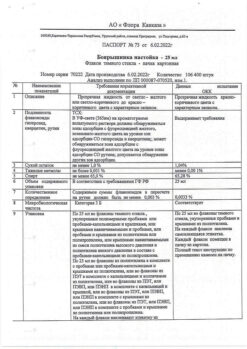
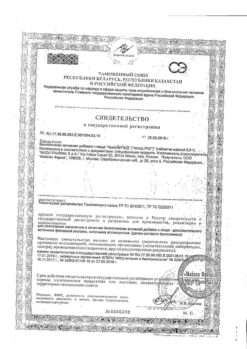
Clexane, 6000 anti-ha me/0.6 ml 0.6 ml syringes 10 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Sodium enoxaparin is a low molecular weight heparin with an average molecular weight of about 4500 daltons (Da): less than 2000 Da – < 20%, 2000 to 8000 Da – > 68%, more than 8000 Da – < 18%. Enoxaparin sodium is obtained by alkaline depolymerization of heparin benzyl ester isolated from pig small intestinal mucosa. Its structure is characterized by a nonreducible fragment of 2-O-sulfo-4-enpyrazino-suronic acid and a reducible fragment of 2-#,6-O-disulfo-O-glucopyranoside. The structure of enoxaparin sodium contains about 20% (ranging from 15% to 25%) of the 1,6-anhydro derivative in the reducing fragment of the polysaccharide chain.
Pharmacodynamics
In a purified in vitro system, sodium enoxaparin has high anti-Xa activity (approximately 100 IU/ml) and low anti-IIa or antithrombin activity (approximately 28 IU/ml). This anticoagulant activity acts through antithrombin III (AT-H), providing anticoagulant activity in humans. In addition to anti-Xa/Pa activity, additional anticoagulant and anti-inflammatory properties of enoxaparin sodium have also been identified in both healthy humans and patients and in animal models. These include AT-S-dependent inhibition of other clotting factors like factor U11a, activation of tissue factor pathway inhibitor (TFP) release, and reduction of Willebrand factor release from the vascular endothelium into the bloodstream. These factors provide the anticoagulant effect of enoxaparin sodium in general.
When used in prophylactic doses, it slightly changes the activated partial thromboplastin time (APT) and has almost no effect on platelet aggregation and on the degree of binding of fibrinogen to platelet receptors.
Pharmacokinetics
Bioavailability and absorption
The absolute bioavailability of enoxaparin sodium with subcutaneous (p/k) administration, estimated on the basis of anti-Xa activity, is close to 100%. Average maximum anti-Xa activity in blood plasma is 3-5 hours after a single n/c injection and reaches approximately 0.2, 0.4, 1.0 and 1.3 anti-Xa IU/ml after a single n/c injection of the drug in doses of 20 mg, 40 mg, 1 mg/kg and 1.5 mg/kg. An intravenous bolus injection of 30 mg followed by immediate subcutaneous administration of 1 mg/kg every 12 hours provides an initial maximum anti-Xa activity of 1.16 IU/ml (n=16), with a mean blood exposure of approximately 88% of the equilibrium state, which is reached on the second day of therapy.
The pharmacokinetics of enoxaparin sodium in the indicated dosing regimens is linear. The variability within and between patient groups is low. After repeated subcutaneous administration of 40 mg of enoxaparin sodium once daily and subcutaneous administration of 1.5 mg/kg body weight once daily in healthy volunteers the equilibrium concentration is reached by day 2, with the area under the pharmacokinetic curve being on average 15% higher than after a single 2 of 30 injections. After repeated subcutaneous injections of enoxaparin sodium at a daily dose of 1 mg/kg body weight twice daily, the equilibrium concentration is reached after 3-4 days, with the area under the pharmacokinetic curve (AUC) on average 65% higher than after a single injection, and the mean values of maximum concentrations are 1.2 IU/ml and 0.52 IU/ml, respectively.
The anti-IIa activity in plasma is about 10 times lower than the anti-Xa activity. The average maximum anti-Xa activity is observed approximately 3-4 h after subcutaneous administration and reaches 0.13 IU/ml and 0.19 IU/ml after repeated administration of 1 mg/kg body weight with twice-daily administration and 1.5 mg/kg body weight with once-daily administration, respectively.
Distribution
The volume of distribution of the anti-Xa activity of enoxaparin sodium is approximately 4.3 L and approximates the volume of circulating blood.
Elimination
Enoxaparin sodium is a low clearance drug. After intravenous administration for 6 h at a dose of 1.5 mg/kg body weight, the average anti-Xa plasma clearance is 0.74 L/h.
The excretion of the drug is monophasic with half-lives (T1/2) of about 5 hours (after single subcutaneous administration) and about 7 hours (after multiple administration of the drug).
Enoxaparin sodium is mainly metabolized in the liver by desulfation and/or depolymerization to form low molecular weight substances with very low biological activity. Excretion through the kidneys of active drug fragments is approximately 10% of the administered dose, and total excretion of active and inactive fragments is approximately 40% of the administered dose.
Particular patient groups
Patients in the elderly (over 75 years): The pharmacokinetic profile of enoxaparin sodium does not differ in elderly patients and younger patients with normal renal function. However, as a result of decreased renal function with age, slower excretion of enoxaparin sodium may be observed in elderly patients.
Hepatic disorders: In a study involving patients with advanced liver cirrhosis who received enoxaparin sodium at a dose of 4000 IU (40 mg) once daily, decreased maximum anti-Xa activity was associated with increased severity of liver function impairment (as assessed by the Child-Pugh score). This decrease page 3 of 30 was mainly due to decreased AT-III levels secondary to decreased AT-III synthesis in patients with impaired liver function.
Kidney function impairment: decreased clearance of enoxaparin sodium has been noted in patients with impaired renal function. After repeated subcutaneous administration of 40 mg of enoxaparin sodium once daily there is increase of anti-Xa activity represented by area under pharmacokinetic curve (AUC) in patients with mild (creatinine clearance (CK) >50 and <80 ml/min) and moderate renal impairment (CK >30 and <50 ml/min). In patients with severe renal impairment (CKR <30 ml/min), the AUC at equilibrium is on average 65% higher with repeated subcutaneous administration of 40 mg of the drug once daily.
Hemodialysis: The pharmacokinetics of enoxaparin sodium were comparable to those in the control population after single IV doses of 25 IU, 50 IU or 100 IU/kg (0.25, 0.50 or 1.0 mg/kg), but the AUC was twice as high as in the control population.
Body weight: After repeated p/q doses of 1.5 mg/kg once daily, the average AUC of anti-Xa activity at equilibrium was slightly higher in overweight patients (BMI 30-48 kg/m2) compared to patients with normal average body weight, while maximum plasma anti-Xa activity was not increased. In overweight patients with subcutaneous administration of the drug, clearance is slightly lower. If no dose adjustment is made for patient weight, after a single subcutaneous injection of 40 mg of sodium enoxaparin, anti-Xa activity will be 52% higher in women with a body weight less than 45 kg and 27% higher in men with a body weight less than 57 kg compared to patients with normal average body weight.
Indications
Indications
Prevention of venous thrombosis and embolism in surgical interventions in moderate- and high-risk patients, especially in orthopedic and general surgical interventions, including cancer.
Prevention of venous thrombosis and embolism in bedridden patients due to acute therapeutic conditions, including acute heart failure and decompensation of chronic heart failure (NYHA class III or IV), respiratory failure, and in severe infections and rheumatic diseases at increased risk of venous thrombosis.
The treatment of deep vein thrombosis with or without pulmonary embolism, except in cases of pulmonary embolism requiring thrombolytic therapy or surgery.
Prevention of thrombosis in the extracorporeal circulation system during hemodialysis.
Acute coronary syndrome:
Active ingredient
Active ingredient
Composition
Composition
Composition per syringe:
active ingredient: enoxaparin sodium 60 mg*;
solvent: water for injection up to 0.6 ml;
* – mass is calculated based on the content of enoxaparin sodium used (theoretical activity of 100 anti-Ha IU/mg).
How to take, the dosage
How to take, the dosage
Subcutaneously, except in special cases.
Prevention of venous thrombosis and embolism in surgical procedures in moderate- and high-risk patients.
In patients at moderate risk of thrombosis and embolism (e.g., abdominal surgeries), the recommended dose of Clexane® is 20 mg once daily subcutaneously. The first injection should be given two hours before surgery.
. Patients at high risk of thrombosis and embolism (e.g., orthopedic surgery, oncologic surgery, patients with additional non-surgical risk factors such as congenital or acquired thrombophilia malignant neoplasm, bed rest for more than three days, obesity, venous thrombosis in anamnesis, varicose veins of lower limbs, pregnancy) the drug is recommended in a dose of 40 mg once a day subcutaneously, with the first dose administered 12 hours before the surgical intervention. If earlier preoperative prophylaxis is necessary (e.g., in patients at high risk of thrombosis and thromboembolism awaiting delayed orthopedic surgery) the last injection should be given 12 hours before surgery and 12 hours after surgery.
The duration of treatment with Clexane® is on average 7-10 days. If necessary, therapy may be continued as long as the risk of thrombosis and embolism persists and as long as the patient remains ambulatory.
In major orthopedic surgeries, it may be appropriate to continue treatment after initial therapy with a dose of 40 mg once daily for five weeks.
In patients at high risk of venous thromboembolism who have undergone surgery, abdominal and pelvic surgery due to cancer, it may be appropriate to increase the duration of administration of Clexane® at a dose of 40 mg once daily for four weeks.
Prevention of venous thrombosis and embolism in bed-ridden patients with acute medical conditions The recommended dose of Clexane® is 40 mg once daily, subcutaneously, for 6-14 days. Therapy should be continued until the patient is fully ambulatory (maximum 14 days).
The treatment of deep vein thrombosis with or without pulmonary embolism
The drug is administered subcutaneously at a rate of 1.5 mg/kg body weight once daily or 1 mg/kg body weight twice daily. The dosing regimen should be chosen by a physician based on the assessment of the risk of thromboembolism and risk of bleeding. In patients without thromboembolic complications and at low risk of venous thromboembolism, the drug is recommended to be administered subcutaneously at a rate of 1.5 mg/kg body weight once daily. In all other patients, including patients with obesity, symptomatic pulmonary thromboembolism, cancer, recurrent venous thromboembolism and proximal thrombosis (in the iliac vein), the drug is recommended at a dose of 1 mg/kg twice daily. The duration of treatment is on average 10 days. It is necessary to start therapy with indirect anticoagulants immediately, at that, treatment with Clexane® should be continued until therapeutic anticoagulant effect is achieved (INR value [International Normalized Ratio] should be 2.0-3.0).
Prevention of thrombosis in extracorporeal circulation during hemodialysis
The recommended dose of Clexane® is on average 1 mg/kg body weight. If the risk of bleeding is high, the dose should be reduced to 0.5 mg/kg body weight for dual vascular access or 0.75 mg/kg for single vascular access.
In hemodialysis, Clexane® should be administered to the arterial shunt site at the beginning of the hemodialysis session. A single dose is usually sufficient for a four-hour session; however, if fibrin rings are detected during longer hemodialysis, an additional dose of 0.5-1 mg/kg body weight may be administered. No data are available for patients using enoxaparin sodium for prophylaxis or treatment and during hemodialysis sessions.
The treatment of unstable angina and myocardial infarction without ST-segment elevation Clexane® is administered at a rate of 1 mg/kg body weight every 12 hours, subcutaneously, with concomitant use of antiplatelet therapy. Average therapy duration is at least 2 days and continues until patient’s clinical condition stabilizes. Usually the drug is administered for 2 to 8 days. Acetylsalicylic acid is recommended for all patients with no contraindications, with an initial dose of 150-300 mg orally followed by a maintenance dose of 75-325 mg once daily.
The treatment of acute ST-segment elevation myocardial infarction, drug or percutaneous coronary intervention Treatment begins with a single intravenous bolus injection of enoxaparin sodium at a dose of 30 mg. Immediately thereafter, enoxaparin sodium is administered subcutaneously at a dose of 1 mg/kg body weight. The drug is then administered subcutaneously at 1 mg/kg of body weight every 12 hours (maximum 100 mg of sodium enoxaparin for each of the first two subcutaneous injections, then 1 mg/kg of body weight for the remaining subcutaneous doses, that is, if the body weight exceeds 100 kg, the single dose may not exceed 100 mg). As soon as possible after detection of acute myocardial infarction with ST-segment elevation, patients should be simultaneously prescribed acetylsalicylic acid and, if there are no contraindications, administration of acetylsalicylic acid (in doses of 75-325 mg) should be continued daily for at least 30 days.
The recommended duration of treatment with Clexane® is 8 days or until discharge from hospital (if hospitalization is less than 8 days).
When combined with thrombolytics (fibrin-specific and fibrin-unspecific), enoxaparin sodium must be administered between 15 minutes before and 30 minutes after initiation of thrombolytic therapy.
In patients aged 75 years and older, an initial intravenous bolus injection is not used. The drug is administered subcutaneously at a dose of 0.75 mg/kg every 12 hours (maximum 75 mg of enoxaparin sodium for each of the first two subcutaneous injections, then 0.75 mg/kg body weight for the remaining subcutaneous doses, that is, if the body weight exceeds 100 kg, the single dose may not exceed 75 mg).
In patients undergoing percutaneous coronary intervention, if the last subcutaneous injection of enoxaparin sodium was given less than 8 hours before the balloon catheter inserted into the coronary artery constriction was inflated, no additional injection of enoxaparin sodium is required. If the last subcutaneous injection of sodium enoxaparin was given more than 8 hours before the balloon catheter was inflated, an additional intravenous bolus injection of sodium enoxaparin at a dose of 0.3 mg/kg should be given.
Interaction
Interaction
Clexan® should not be mixed with other medicines!
Do not recommend combinations:
Drugs that affect hemostasis (systemic salicylates, acetylsalicylic acid in doses with anti-inflammatory effects, nonsteroidal anti-inflammatory drugs (NSAIDs), including ketorolac, other thrombolytics (alteplase, reteplase, streptokinase, tenecteplase, urokinase)) should be stopped before starting therapy with Enoxaparin Sodium. If concomitant use with enoxaparin sodium is necessary, caution should be exercised and close clinical observation and monitoring of relevant laboratory parameters should be performed.
Combinations requiring caution
Other drugs affecting hemostasis, such as:
– Platelet aggregation inhibitors, including acetylsalicylic acid at doses with antiaggregant effects (cardioprotection), clopidogrel, ticlopidine, and glycoprotein IIb/IIIa receptor antagonists indicated for acute coronary syndrome due to increased risk of bleeding;
– dextran with a molecular weight of 40 kDa;
– systemic glucocorticosteroids.
Potassium increasing drugs When concomitant use with drugs that increase potassium content in the blood serum, clinical and laboratory monitoring should be performed.
Directions for use
Directions for use
Perfections of administration:
The pre-filled disposable syringe is ready for use.
The product should not be injected intramuscularly!
Subcutaneous injection:
Injections should preferably be done in the supine position of the patient. If using 20 mg and 40 mg pre-filled syringes, do not remove any air bubbles from the syringe before injection to avoid loss of medication. Injections should be given alternately on the left or right anterolateral or posterolateral surface of the abdomen.
The needle should be inserted full length, vertically (not laterally), into the skin fold, gathered and held between the thumb and forefinger until the injection is complete. The skin fold should not be released until the injection is complete. The injection site should not be massaged after the injection.
Intravenous bolus injection:
Intravenous bolus injection of sodium enoxaparin should be performed through a venous catheter. Enoxaparin sodium should not be mixed or administered with other medications. In order to avoid the presence of traces of other drugs in the infusion system and their interaction with sodium enoxaparin, the venous catheter should be flushed with sufficient amounts of 0.9% sodium chloride solution or 5% dextrose solution before and after intravenous bolus injection of sodium enoxaparin. Enoxaparin sodium can be administered safely with 0.9% sodium chloride solution and 5% dextrose solution.
In order to perform a 30 mg bolus infusion of enoxaparin sodium in the treatment of acute ST-segment elevation myocardial infarction, the 60 mg, 80 mg and 100 mg glass syringes are discarded so that only 30 mg (0.3 ml) remains. The 30 mg dose can be given directly intravenously.
Pre-filled 60 mg, 80 mg and 100 mg hypodermic syringes may be used for intravenous bolus injection of enoxaparin sodium via a venous catheter. The 60 mg syringe is recommended because it reduces the amount of drug removed from the syringe. The 20 mg syringe is not used because it does not contain enough preparation for a 30 mg bolus of enoxaparin sodium. The 40 mg syringe is not used because it has no graduations and therefore cannot accurately measure the 30 mg. To improve the accuracy of additional intravenous bolus injection of small volumes into a venous catheter during percutaneous coronary interventions, it is recommended that the drug be diluted to a concentration of 3 mg/ml. Dilution of the solution is recommended immediately prior to administration.
To obtain 3 mg/ml Enoxaparin sodium solution using a pre-filled 60 mg syringe, it is recommended to use a 50 ml infusion solution container (i.e. 0.9% sodium chloride solution or 5% dextrose solution). From the container with the infusion solution using a standard syringe 30 ml of the solution is extracted and removed. Enoxaparin sodium (the contents of the 60 mg hypodermic syringe) is injected into the remaining 20 ml of the infusion solution in the container. The contents of the container with the diluted sodium enoxaparin solution are mixed gently. A syringe is used to extract the required volume of diluted enoxaparin sodium solution, which is calculated according to the formula:
Volume of diluted solution = Patient body weight (kg) x 0.1
Special Instructions
Special Instructions
General
Low molecular weight heparins are not interchangeable, since they differ in manufacturing process, molecular weight, specific anti-Xa activity, dosing units and dosing regimen, with associated differences in their pharmacokinetics and biological activity (antithrombin activity and interaction with platelets). Therefore, it is necessary to strictly follow the recommendations for the use of each drug belonging to the class of low molecular weight heparins.
Bleeding
As with other anticoagulants, administration of Clexane® may cause bleeding of any localization
If bleeding occurs, the source of bleeding must be found and appropriate treatment administered.
Enoxaparin sodium, like other anticoagulants, should be used with caution in conditions with increased risk of bleeding, such as:
Bleeding in elderly patients
When using enoxaparin sodium in prophylactic doses in elderly patients no increased risk of bleeding was noted.
When using the drug in therapeutic doses in elderly patients (especially those aged 80 years and older) there is an increased risk of bleeding. Close monitoring of these patients is recommended. The use of drugs that affect hemostasis (salicylates of systemic action, including acetylsalicylic acid in doses that have an anti-inflammatory effect, NSAIDs, including ketorolac, other thrombolytics (alteplase, reteplase, streptokinase, tenecteplase, urokinase)) is recommended to cancel before treatment with Enoxaparin sodium, except when their use is necessary. If their concomitant use with enoxaparin sodium is indicated, close clinical observation and monitoring of relevant laboratory parameters should be performed.
Renal failure
In patients with impaired renal function, there is an increased risk of bleeding as a result of increased systemic exposure to enoxaparin sodium. In patients with severe renal impairment (CKR >15 and <30 ml/min) there is a significant increase in exposure of enoxaparin sodium, therefore it is recommended to perform dose adjustment both during prophylactic and therapeutic use of the drug. Although there is no need to perform dose adjustment in patients with renal dysfunction of mild (CK >30 and <50 ml/min) and moderate severity (CK >50 and <80 ml/min), it is recommended to monitor closely such patients, and biological monitoring with measurement of anti-Xa activity may be considered. The use of enoxaparin sodium is not recommended in patients with end-stage chronic kidney disease (CK <15 ml/min) due to lack of data, except for the prevention of thrombosis in the extracorporeal circulation system during hemodialysis.
Low body weight
There has been increased exposure to enoxaparin sodium when used prophylactically in women with a body weight less than 45 kg and in men with a body weight less than 57 kg, which may lead to an increased risk of bleeding. Close monitoring of such patients is recommended.
Patients with obesity
Patients with obesity have an increased risk of thrombosis and embolism. The safety and efficacy of enoxaparin sodium in prophylactic doses in obese patients (BMI greater than 30 kg/m2) is not fully defined and there is no general consensus on dose adjustment. It is recommended that patients be monitored for signs and symptoms of thrombosis and embolism.
Control of peripheral blood platelet counts.
The risk of antibody-mediated heparin-induced thrombocytopenia (HIT) also exists with the use of low-molecular-weight heparins, with a higher risk in patients who have undergone heart surgery and patients with cancer. If thrombocytopenia develops, it is usually detected between day 5 and 21 after the start of therapy with enoxaparin sodium. Therefore, it is recommended to monitor the peripheral blood platelet count regularly before and during treatment with Enoxaparin sodium. Blood platelet counts should be determined in the presence of symptoms suggestive of HIT (new episode of arterial and/or venous thromboembolic complications, painful skin lesions at the injection site, allergic or anaphylactic reactions during treatment). The treating physician should be informed if any of these symptoms occur. If there is a confirmed significant decrease in the platelet count (30-50% compared to the baseline), Enoxaparin sodium should be immediately withdrawn and the patient should be transferred to another anticoagulant therapy without the use of heparins.
Spinal/epidural anesthesia
There have been reports of neuroaxial hematomas when using enoxaparin sodium concomitantly with spinal/epidural anesthesia with the development of long-standing or irreversible paralysis. The risk of these phenomena is reduced when using the drug at a dose of 40 mg or lower. The risk increases when using higher doses of Enoxaparin sodium, as well as when using permanent catheters after surgery, or when concomitant use of additional drugs that affect hemostasis, such as NSAIDs (see section “Interaction with other medicinal products”). The risk also increases with traumatic or repeated spinal tap or in patients with a history of spinal surgery or spinal deformity.
In order to reduce the possible risk of bleeding associated with the use of enoxaparin sodium and epidural or spinal anesthesia/analgesia, the pharmacokinetic profile of the drug should be considered (see section “Pharmacokinetics”). Catheter placement or removal is better performed when the anticoagulant effect of enoxaparin sodium is low, but the exact time to achieve sufficient reduction of anticoagulant effect in different patients is unknown. Additionally, note that in patients with a CK of 15-30 mL/min, excretion of enoxaparin sodium is delayed.
If anticoagulant therapy is prescribed by a physician during epidural/spinal anesthesia or lumbar puncture, the patient should be continuously monitored for any neurological symptoms such as back pain, sensory and motor disturbances (numbness or weakness in the lower extremities), impaired bowel and/or bladder function. The patient should be instructed to inform the physician immediately if the above symptoms occur. If symptoms characteristic of a spinal cord hematoma are suspected, prompt diagnosis and treatment, including spinal cord decompression if necessary, are necessary.
Heparin-induced thrombocytopenia
The use of enoxaparin sodium in patients with a history of heparin-induced thrombocytopenia within the past 100 days or in the presence of circulating antibodies is contraindicated. Circulating antibodies may persist for several years. Enoxaparin sodium should be used with special caution in patients with a history (more than 100 days) of heparin-induced thrombocytopenia without circulating antibodies. The decision to use enoxaparin sodium in this situation should be made only after a benefit/risk assessment and in the absence of heparin-free alternative therapy.
Prescope coronary angioplasty
In order to minimize the risk of bleeding associated with invasive vascular instrumentation in the treatment of unstable angina and myocardial infarction without Q-wave and acute myocardial infarction with ST-segment elevation, these procedures should be performed in intervals between drug administrations. This is necessary to achieve hemostasis at the catheter insertion site after percutaneous coronary intervention. If a femoral artery intraductor device is used, the femoral artery intraductor can be removed immediately. If manual compression is used, the femoral artery intromedullary tube should be removed 6 h after the last intravenous or subcutaneous injection of sodium enoxaparin. If treatment with sodium enoxaparin is continued, the next dose should not be administered before 6-8 h after removal of the femoral artery intraductor. The site of insertion of the intraductor should be monitored to detect timely signs of bleeding and hematoma formation.
Patients with mechanical artificial heart valves
The use of enoxaparin sodium for prophylaxis of thrombosis in patients with mechanical artificial heart valves has not been well studied. There have been isolated reports of heart valve thrombosis in patients with mechanical artificial heart valves on therapy with enoxaparin sodium for prophylaxis of thrombosis. Because of insufficient clinical data and ambiguous factors, including underlying disease, it is difficult to evaluate such reports.
Pregnant women with mechanical artificial heart valves
The use of enoxaparin sodium for prophylaxis of thrombosis in pregnant women with mechanical artificial heart valves has not been well studied.
In a clinical study involving pregnant women with mechanical artificial heart valves, when enoxaparin sodium was used at a dose of 1 mg/kg body weight twice daily to reduce the risk of thrombosis and embolism, 2 of 8 women developed thrombi that resulted in heart valve block and death to the mother and fetus. There have been anecdotal post-marketing reports of heart valve thrombosis in pregnant women with mechanical artificial heart valves treated with enoxaparin sodium to prevent thrombus formation. Pregnant women with mechanical artificial heart valves may have an increased risk of thrombosis and embolism.
Skin necrosis/skin vasculitis
The development of skin necrosis and skin vasculitis has been reported with the use of low molecular weight heparins. If skin necrosis/skin vasculitis develops, the use of the drug should be discontinued.
The use of heparin is not recommended in patients with acute infective endocarditis due to the risk of hemorrhagic stroke. If the use of the drug is considered absolutely necessary, the decision should be made only after careful individual evaluation of the benefit-risk ratio.
Laboratory tests
In doses used for prevention of thromboembolic complications, the drug Clexane® has no significant effect on bleeding time and clotting parameters, as well as on platelet aggregation or their binding to fibrinogen. The ACTV and activated clotting time may be prolonged when increasing the dose. Increase of ACTV and activated clotting time are not in direct linear dependence on increase of anticoagulant activity of the drug, therefore there is no need to monitor them.
Hyperkalemia
Heparins may inhibit aldosterone secretion by the adrenal glands, resulting in the development of hyperkalemia, especially in patients with diabetes, chronic renal failure, prior metabolic acidosis, taking medications that increase potassium content. Plasma potassium levels should be monitored regularly, especially in patients in the risk group.
Prevention of venous thrombosis and embolism in patients with acute therapeutic conditions who are on bed rest
In case of acute infection, acute rheumatic conditions, prophylactic use of enoxaparin sodium is justified only if the above conditions are combined with one of the following risk factors for venous thrombosis
Hepatic disorders
Enoxaparin sodium should be used with caution in patients with liver dysfunction due to increased risk of bleeding. Dose adjustment based on monitoring of anti-Xa activity in patients with cirrhosis is unreliable and is not recommended.
Synopsis
Synopsis
Contraindications
Contraindications
Hypersensitivity to enoxaparin sodium, heparin or its derivatives, including other low molecular weight heparins.
Spinal or epidural anesthesia or locoregional anesthesia when sodium enoxaparin has been used for treatment in the previous 24 h.
Immune-mediated heparin-induced thrombocytopenia (history) within the past 100 days or the presence of circulating antiplatelet antibodies in the blood.
Children under 18 years of age because efficacy and safety have not been established in this patient population.
Side effects
Side effects
Blood and lymphatic system disorders:
often: bleeding, thrombocytopenia, thrombocytosis;
rarely: cases of autoimmune thrombocytopenia with thrombosis; in some cases, thrombosis was complicated by the development of organ infarction or limb ischemia
Intensive immune system disorders:
often: allergic reactions.
Liver and biliary tract disorders:
very often: increased activity of “liver” enzymes, mainly increased activity of transaminases, more than three times the upper limit of normal.
Skin and subcutaneous tissue disorders:
often: urticaria, skin itching, erythema.
infrequent: bullous dermatitis.
General disorders and disorders at the site of administration:
often: injection site hematoma, injection site pain, injection site edema, bleeding, hypersensitivity reactions, inflammation, formation of lumps at the injection site.
Infrequent: irritation at the injection site, necrosis of the skin at the injection site.
Overdose
Overdose
Accidental overdose of Clexane® in intravenous, extracorporeal or subcutaneous administration may lead to hemorrhagic complications. When administered orally, even large doses are unlikely to be absorbed.
The anticoagulant effects can mainly be neutralized by slow intravenous administration of protamine sulfate, the dose of which depends on the dose administered. One mg (1 mg) of protamine sulfate will neutralize the anticoagulant effect of one mg (1 mg) of Clexane® (see information on the use of protamine sulfate preparations) if enoxaparin sodium was administered no more than 8 hours before protamine administration. 0.5 mg of protamine will neutralize anticoagulant effect of 1 mg of the drug if more than 8 hours have passed since the last injection or if it is necessary to administer the second protamine dose. If, however, 12 hours or more have elapsed since the administration of enoxaparin sodium, no protamine administration is required. However, even with high doses of protamine sulfate, the anti-Xa activity of Clexane® is not completely neutralized (maximum 60 %).
Pregnancy use
Pregnancy use
There is no evidence that enoxaparin sodium crosses the placental barrier during pregnancy. Because adequate and well-controlled studies involving pregnant women are lacking, and animal studies do not always predict response to enoxaparin sodium administration during pregnancy in humans, it should only be used during pregnancy in exceptional cases where there is an urgent medical need for its use.
Patients should be monitored for signs of bleeding or excessive anticoagulation, and patients should be advised of the risk of bleeding.
There is no evidence of an increased risk of bleeding, thrombocytopenia, or osteoporosis in pregnant women, except as noted in patients with artificial heart valves.
If epidural anesthesia is planned, it is recommended that enoxaparin sodium be withdrawn before it is performed.
Breast-feeding period
It is not known whether unchanged enoxaparin sodium is excreted into breast milk. Absorption of enoxaparin sodium in the gastrointestinal tract in the infant is unlikely. Clexane® may be used during breastfeeding.
Similarities
Similarities
Additional information
| Shelf life | 3 years. Do not use the drug after the expiration date stated on the package. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25°C. Keep out of reach of children. |
| Manufacturer | Pharmstandard-UfaVITA, Russia |
| Medication form | solution for injection |
| Brand | Pharmstandard-UfaVITA |
Related products
Buy Clexane, 6000 anti-ha me/0.6 ml 0.6 ml syringes 10 pcs with delivery to USA, UK, Europe and over 120 other countries.