No products in the cart.
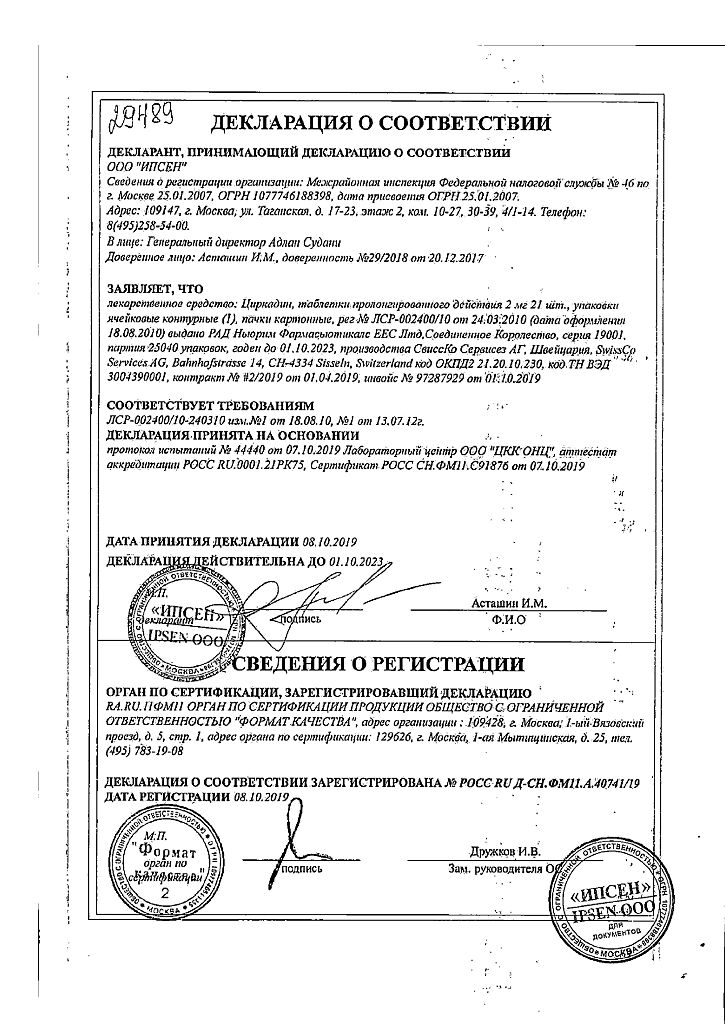
Circadin, 2 mg 21 pcs
€23.48 €20.35
Out of stock
(E-mail when Stock is available)
EAN: 4630001120429
SKU: 216260
Categories: Medicine, Neurology and Psychiatry, Sedatives and hypnotics
Description
Pharmacodynamics
Melatonin is a synthetic analog of the hormone produced by the epiphysis, its chemical structure is similar to serotonin. Under physiological conditions, melatonin secretion increases shortly after dark, peaks at 2-4am and decreases during the second half of the night. Melatonin is thought to control circadian rhythms and the perception of the day-night cycle.
It has a hypnotic effect and improves sleep. The effects of melatonin on the MT1, MT2 and MT3 receptors are thought to increase the sleeping effect, since these receptors (predominantly MT1 and MT2) are involved in the regulation of circadian rhythms and sleep. Endogenous melatonin content decreases with age, so the drug may significantly improve the quality of sleep in primary insomnia, especially in patients older than 55 years.
Cirkadine at a dose of 2 mg/day in the evening improves sleep duration and quality, and also improves activity during waking hours, without worsening psychomotor reactions during the day.
Pharmacokinetics
Absorption. Melatonin after oral administration in adults is rapidly absorbed in the gastrointestinal tract, in the elderly the absorption rate may be reduced by 50%. The kinetics of melatonin in the range of 2-8 mg is linear. Bioavailability is 15%. There is a significant effect of primary passage through the liver with a primary metabolism value of 85%. Tmax is 3 h in the saturated state. Food intake affects the absorption of melatonin and its Cmax when taking Circadin at a dose of 2 mg. Concomitant food intake slowed melatonin absorption, resulting in a later Tmax (Tmax = 3 h versus Tmax = 0.75 h) and lower Cmax (Cmax = 1020 pg/mL versus Cmax = 1176 pg/mL).
Distribution. In in vitro studies, the binding of melatonin to plasma proteins is 60%. Melatonin primarily binds to albumin, α1-acid glycoprotein and HDL.
Biotransformation. Experimental studies suggest that the CYP1A1, CYP1A2, and possibly CYP2C19 isoenzymes of the cytochrome P450 system are involved in the metabolism of melatonin. The main metabolite of melatonin, 6-sulfatoxymelatonin, is inactive. The process of presystemic metabolism occurs in the liver. Excretion of the metabolite is completed within 12 hours after oral administration.
Excretion. T1/2 is 3.5 h. Excretion is 89% by the kidneys as sulfated and glucuronated 6-hydroxymelatonin conjugates, and 2% is excreted unchanged.
Gender. There is a 3-4-fold increase in Cmax in women compared with men.
There is also a five-fold interindividual variability in Cmax within the same sex.
However, despite differences in plasma concentrations, no pharmacodynamic differences were found between males and females.
Elderly patients. Melatonin metabolism is known to slow down with age. At different doses of melatonin, higher AUC and Cmax values were obtained in the elderly, reflecting reduced melatonin metabolism in this group of patients. While Cmax in adults (18-45 years) is 500 pg/mL, in the elderly (55-69 years) it is 1200 pg/mL; AUC in adults is 3000 pg-h/ml and 5000 pg-h/ml in the elderly.
Patients with impaired renal function. No cumulation of melatonin has been noted with long-term treatment. These data are consistent with the short half-life of melatonin in humans. After 1 and 3 weeks of treatment with Circadin at a dose of 2 mg blood samples were taken at 23:00 (2 hours after oral administration). Concentration was (411.4±56.5) and (432±83.2) pg, respectively, and similar to that in healthy volunteers taking 2 mg of Circadin once daily.
Patients with impaired liver function. The liver is the main organ involved in melatonin metabolism, so liver disease leads to increased concentrations of endogenous melatonin.
In patients with liver cirrhosis, the plasma concentration of melatonin was significantly increased during the daytime. Compared with the control group, there was a significant decrease in total excretion of 6-sulfatoxymelatonin.
Indications
Indications
Short-term treatment of primary insomnia characterized by poor sleep quality in patients over 55 years of age (as monotherapy).
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Melatonin is a synthetic analogue of the hormone produced by the pineal gland; its chemical structure is close to serotonin. Under physiological conditions, melatonin secretion increases shortly after dark, reaches its maximum values at 2–4 am and decreases during the second half of the night. Melatonin is thought to control circadian rhythms and perception of the day-night cycle.
Has a hypnotic effect and improves sleep. It is assumed that the effect of melatonin on the MT1, MT2 and MT3 receptors enhances the hypnotic effect, since these receptors (mainly MT1 and MT2) are involved in the regulation of circadian rhythms and sleep. The content of endogenous melatonin decreases with age, so the drug can significantly improve the quality of sleep in primary insomnia, especially in patients over 55 years of age.
Circadin at a dose of 2 mg/day in the evening increases the duration and improves the quality of sleep, and also improves activity during wakefulness, without worsening psychomotor reactions during the day.
Pharmacokinetics
Absorption. After oral administration in adults, melatonin is rapidly absorbed into the gastrointestinal tract; in the elderly, the rate of absorption can be reduced by 50%. The kinetics of melatonin in the range of 2–8 mg is linear. Bioavailability is 15%. There is a significant effect of first pass through the liver with a primary metabolism value of 85%. Tmax – 3 hours in a fed state. Food intake affects the absorption of melatonin and its Cmax when taking Circadin at a dose of 2 mg. Concomitant meals delayed melatonin absorption, resulting in a later Tmax (Tmax = 3 hours vs. Tmax = 0.75 hours) and lower Cmax (Cmax = 1020 pg/mL vs. Cmax = 1176 pg/mL).
Distribution. In in vitro studies, the binding of melatonin to plasma proteins is 60%. Melatonin binds primarily to albumin, α1-acid glycoprotein, and HDL.
Biotransformation. Experimental studies suggest that isoenzymes CYP1A1, CYP1A2 and, possibly, CYP2C19 of the cytochrome P450 system are involved in the metabolism of melatonin. The main metabolite of melatonin, 6-sulfatoxymelatonin, is inactive. The process of first-pass metabolism occurs in the liver. Excretion of the metabolite is completed within 12 hours after oral administration.
Excretion. T1/2 is 3.5 hours. 89% of excretion is carried out by the kidneys in the form of sulfated and glucuronidated 6-hydroxymelatonin conjugates, and 2% is excreted unchanged.
Floor. Women experience a 3–4-fold increase in Cmax compared to men.
A fivefold interindividual variability of Cmax within one sex was also noted.
However, despite differences in plasma concentrations, no pharmacodynamic differences have been identified between men and women.
Elderly patients. Melatonin metabolism is known to slow down with age. At different doses of melatonin, higher AUC and Cmax values were obtained in the elderly, reflecting reduced melatonin metabolism in this group of patients. While the Cmax in adults (18–45 years) is 500 pg/ml, in the elderly (55–69 years) it is 1200 pg/ml; AUC in adults is 3000 pg h/ml and 5000 pg h/ml in the elderly.
Patients with impaired renal function. With long-term treatment, no accumulation of melatonin was observed. These data are consistent with the short half-life of melatonin in humans. After 1 and 3 weeks of course treatment with Circadin at a dose of 2 mg, blood was drawn at 23:00 (2 hours after taking the drug orally), the concentration was (411.4 ± 56.5) and (432 ± 83.2) pg, respectively, and was similar to that after a single dose of 2 mg of Circadin to healthy volunteers.
Patients with impaired liver function. The liver is the main organ involved in melatonin metabolism, so liver diseases lead to increased concentrations of endogenous melatonin.
In patients with liver cirrhosis, plasma melatonin concentrations increased significantly during the daytime. Compared with the control group, there was a significant decrease in the total excretion of 6-sulfatoxymelatonin.
Special instructions
Special instructions
Circadin may cause drowsiness. Therefore, the drug should be prescribed with caution if the resulting drowsiness threatens the safety of the patient.
There are no clinical data on the use of Circadin in patients with autoimmune diseases; therefore, Circadin is not recommended for use in patients with autoimmune diseases. This drug should not be used in patients with rare hereditary galactose intolerance, Lapp lactase deficiency or glucose-galactose malabsorption.
Impact on the ability to drive vehicles and machinery. Circadin has a moderate effect on driving and operating machinery. Circadin may cause drowsiness and should be used with caution if the effects of drowsiness may pose a safety concern.
Active ingredient
Active ingredient
Melatonin
Composition
Composition
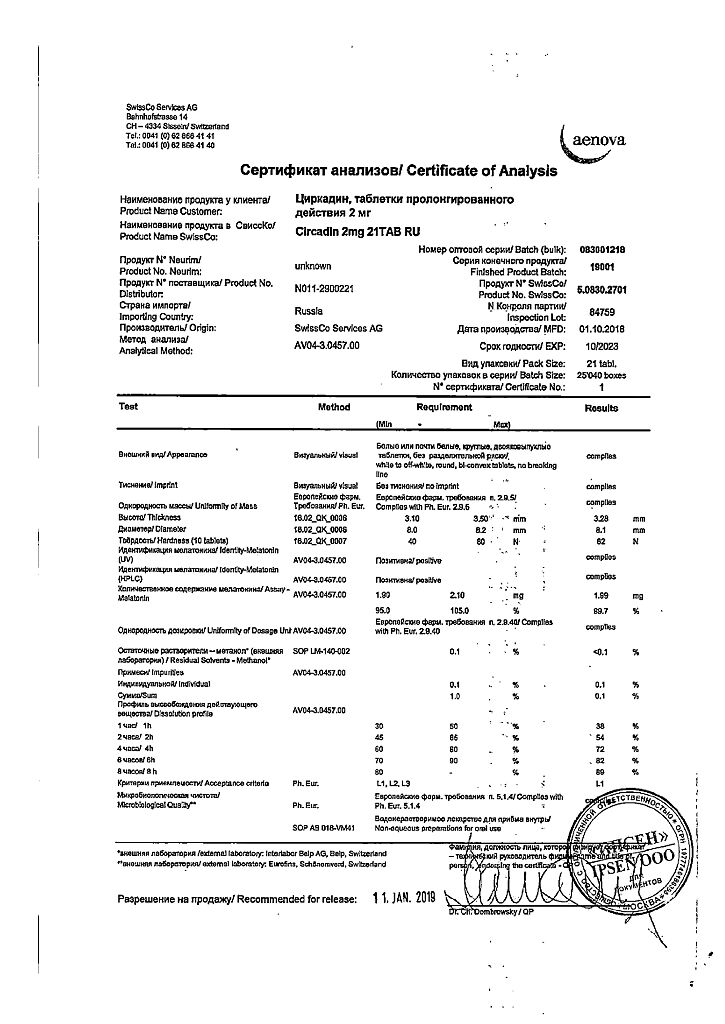
1 extended-release tablet contains:
active ingredient:
melatonin 2 mg,
excipients:
methyl methacrylate,
trimethylammonioethyl methacrylate chloride and ethyl acrylate copolymer [1:2:0.1] – 40 mg;
calcium hydrogen phosphate dihydrate – 40 mg;
lactose monohydrate – 80 mg;
colloidal silicon dioxide – 2 mg;
talc – 4 mg;
magnesium stearate – 2 mg
Pregnancy
Pregnancy
There are no clinical data on the effects of melatonin on pregnancy. Data from preclinical studies do not indicate an adverse effect on pregnancy, fetal development, delivery or postnatal development of newborns. Due to the lack of clinical data, the use of Circadin during pregnancy in women planning pregnancy is not recommended.
Because endogenous melatonin is detected in breast milk, it is likely that exogenous melatonin can also pass into breast milk. Data from animals including rodents, sheep, cattle and primates indicate transfer of melatonin through the placenta or milk from mother to fetus. Therefore, it is not recommended to take melatonin during breastfeeding.
Contraindications
Contraindications
hypersensitivity to the components of the drug Circadin (active and auxiliary substances);
congenital galactose intolerance, glucose-galactose malabsorption syndrome, congenital lactase deficiency;
autoimmune diseases;
liver failure;
age under 18 years (efficacy and safety of use have not been established).
Side Effects
Side Effects
In clinical trials, 48.8% of patients treated with Circadin reported adverse reactions compared to 37.8% in the placebo group. Comparing the rate of patients with adverse reactions per 100 week-patients, the rate in the placebo group was higher than in the Circadin group (5.743 placebo vs. 3.013 Circadin). The most common adverse reactions were headache, nasopharyngitis, back pain and joint pain, which were common in both groups. The list below includes only those adverse reactions from clinical trials that were observed in patients at an equal or greater frequency than in the placebo group.
The frequency of adverse reactions is classified as follows: very often (≥1/10); often (≥1/100 to
Infectious and parasitic diseases: rarely – herpes zoster.
From the blood and lymphatic system: rarely – leukopenia, thrombocytopenia.
From the immune system: frequency unknown – hypersensitivity reactions.
Metabolism and nutrition: rarely – hypertriglyceridemia, hypokalemia, hyponatremia.
Mental disorders: infrequently – irritability, nervousness, anxiety, insomnia, unusual dreams, nightmares, anxiety; rarely – mood swings, aggression, agitation, tearfulness, symptoms of stress, disorientation, early morning awakening, increased libido, decreased mood, depression.
From the nervous system: infrequently – migraine, headache, lethargy, psychomotor hyperactivity, dizziness, drowsiness; rarely – fainting, memory impairment, impaired concentration, dreamlike state, restless leg syndrome, poor quality of sleep, paresthesia.
From the organ of vision: rarely – decreased visual acuity, blurred vision, increased lacrimation.
From the organ of hearing and labyrinthine disorders: rarely – vertigo, positional vertigo.
From the side of the heart: rarely – angina pectoris, palpitations.
From the side of blood vessels: infrequently – arterial hypertension, rarely – hot flashes.
From the gastrointestinal tract: uncommon – abdominal pain, abdominal pain in the upper abdomen, dyspepsia, ulcerative stomatitis, dry mouth, nausea; rarely – gastroesophageal reflux disease, gastrointestinal disorder or disorder, blistering of the oral mucosa, ulcerative glossitis, vomiting, abnormal bowel sounds, bloating, hypersecretion of saliva, bad breath, abdominal discomfort, indigestion, gastritis.
From the liver and biliary tract: rarely – hyperbilirubinemia.
From the skin and subcutaneous tissues: uncommon – dermatitis, night sweats, itching and generalized itching, rash, dry skin; rarely – eczema, erythema, hand dermatitis, psoriasis, generalized rash, itchy rash, nail damage; frequency unknown – Quincke’s edema, swelling of the mouth, swelling of the tongue.
From the musculoskeletal and connective tissue side: infrequently – pain in the limb; rarely – arthritis; muscle spasm, neck pain, night cramps.
From the kidneys and urinary tract: infrequently – glucosuria, proteinuria; rarely – polyuria, hematuria, nocturia.
From the genital organs and mammary gland: infrequently – menopausal symptoms; rarely – priapism, prostatitis; frequency unknown – galactorrhea.
General disorders and disorders at the injection site: uncommon – asthenia, chest pain; rarely – fatigue, pain, thirst.
Laboratory and instrumental data: infrequently – deviation from the norm in laboratory parameters of liver function, increase in body weight; rarely – increased activity of liver transaminases, abnormal levels of electrolytes in the blood, abnormal results of laboratory tests.
Interaction
Interaction
Pharmacokinetic interaction
It is known that at concentrations significantly higher than therapeutic levels, melatonin induces the CYP3A isoenzyme in vitro. The clinical significance of this phenomenon is not fully understood. If signs of induction develop, you should consider reducing the dose of concomitantly used drugs. At concentrations significantly higher than therapeutic levels, melatonin does not induce CYP1A isoenzymes in vitro. Therefore, the interaction of melatonin with other drugs due to the effect of melatonin on isoenzymes of the CYP1A group is apparently insignificant. Melatonin metabolism is mainly mediated by CYP1A isoenzymes. Therefore, it is possible that melatonin may interact with other drugs due to the effect of melatonin on isoenzymes of the CYP1A group.
Caution should be exercised in patients taking fluvoxamine, which increases melatonin concentrations (17-fold increase in AUC and 12-fold increase in Cmax) due to inhibition of its metabolism by cytochrome P450 isoenzymes (CYP): CYP1A2 and CYP2C19. This combination should be avoided. Caution should be exercised in patients taking 5- and 8-methoxypsoralen, which increases melatonin concentrations due to inhibition of its metabolism. Caution should be exercised in patients taking cimetidine (an inhibitor of CYP2D isoenzymes) as it increases plasma melatonin levels by inhibiting the latter.
Smoking can reduce melatonin concentrations due to the induction of the CYP1A2 isoenzyme.
Caution should be exercised in patients taking estrogens (such as contraceptives or hormone replacement therapy), which increase melatonin concentrations by inhibiting their metabolism by CYP1A1 and CYP1A2 isoenzymes.
Inhibitors of CYP1A2 isoenzymes, such as quinolones, can increase melatonin exposure.
Inducers of the CYP1A2 isoenzyme, such as carbamazepine and rifampicin, can reduce plasma concentrations of melatonin.
In modern literature there is a lot of data regarding the effect of agonists/antagonists of adrenergic and opioid receptors, antidepressants, PG inhibitors, benzodiazepines, tryptophan and alcohol on the secretion of endogenous melatonin. Studies of the mutual influence of these drugs on the dynamics or kinetics of Circadin have not been conducted.
Pharmacodynamic interaction
You should not drink alcohol while taking Circadin, because… it reduces the effectiveness of the drug.
Circadin potentiates the sedative effects of benzodiazepine and non-benzodiazepine hypnotics such as zaleplon, zolpidem and zopiclone. In a clinical study, clear evidence of a transient pharmacodynamic interaction between Circadin and zolpidem was observed 1 hour after dosing. Combined use may lead to progressive impairment of attention, memory and coordination compared to zolpidem monotherapy.
During the studies, Circadin was prescribed together with thioridazine and imipramine, drugs that affect the central nervous system. In none of the cases was a clinically significant pharmacokinetic interaction detected. However, concomitant use with Circadin resulted in increased feelings of calmness and difficulty performing certain tasks compared with imipramine monotherapy, as well as increased feelings of brain fog compared with thioridazine monotherapy.
Overdose
Overdose
There have been no cases of overdose of Circadin. The drug was used at a dose of 5 mg/day in clinical studies lasting more than 12 months, with no change in the nature of the reported side effects.
There is literature data on the use of Circadin in a daily dose of up to 300 mg without the occurrence of clinically significant side effects. In case of overdose, drowsiness is expected to develop. Clearance of the active substance is expected within 12 hours after oral administration. No special treatment is required.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C
Shelf life
Shelf life
5 years
Manufacturer
Manufacturer
SwissCo Services AG, Switzerland
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | SwissCo Services AG, Switzerland |
| Medication form | slow-release tablets |
| Brand | SwissCo Services AG |
Related products
Buy Circadin, 2 mg 21 pcs with delivery to USA, UK, Europe and over 120 other countries.