No products in the cart.
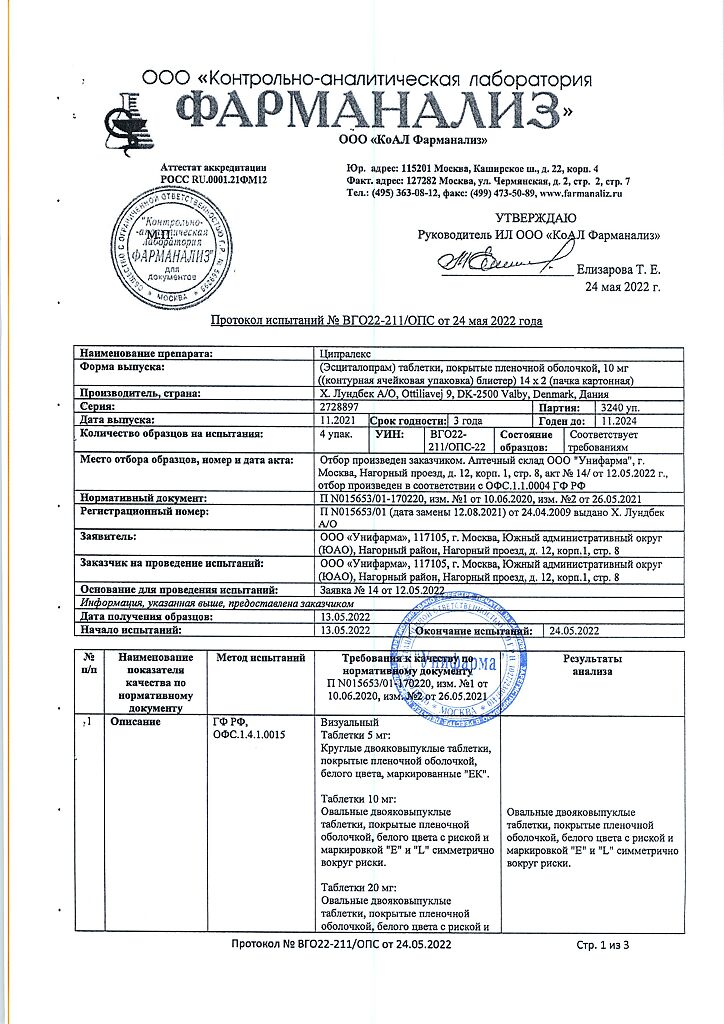
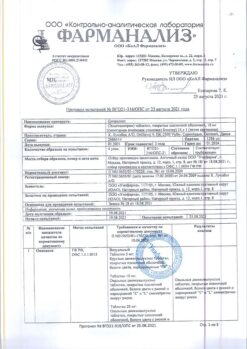
Cipralex, 10 mg 28 pcs
€84.34 €70.28
Description
Cipralex is an antidepressant, a selective inhibitor of serotonin reuptake.
Inhibition of serotonin reuptake leads to increased concentration of this neurotransmitter in the synaptic cleft, increases and prolongs its effect on postsynaptic receptor sites.
Escitalopram has no or very weak ability to bind to a number of receptors, including: serotonin 5-HT1A-, 5-HT2-receptors, dopamine D1- and D2-receptors, a1-, a2-, b-adrenergic receptors, histamine H1-receptors, m-cholinoreceptors, benzodiazepine and opioid receptors.
Indications
Indications
Depressive episodes of any severity;
Panic disorders with/without agoraphobia.
Pharmacological effect
Pharmacological effect
Cipralex is an antidepressant, selective serotonin reuptake inhibitor.
Inhibition of serotonin reuptake leads to an increase in the concentration of this neurotransmitter in the synaptic cleft, enhancing and prolonging its effect on postsynaptic receptor sites.
Escitalopram has no or very weak ability to bind to a number of receptors, including: serotonin 5-HT1A, 5-HT2 receptors, dopamine D1 and D2 receptors, a1-, a2-, b-adrenergic receptors, histamine H1 receptors, m-cholinergic receptors, benzodiazepine and opioid receptors.
Special instructions
Special instructions
Escitalopram should not be administered concomitantly with MAO inhibitors. Escitalopram can be prescribed 14 days after stopping treatment with irreversible MAO inhibitors and at least 1 day after stopping therapy with reversible MAO type A inhibitors (including moclobemide). At least 7 days must pass after stopping escitalopram before treatment with non-selective MAO inhibitors can be started.
Some patients with panic disorder may experience increased anxiety when starting treatment with selective serotonin reuptake inhibitors (including escitalopram). This paradoxical reaction usually disappears within 2 weeks of treatment. To reduce the likelihood of an anxiogenic effect, it is recommended to use the drug in low initial doses.
Escitalopram should be discontinued if seizures develop. The use of the drug in patients with unstable epilepsy is not recommended; Controlled seizures require careful monitoring. If the frequency of seizures increases, selective serotonin reuptake inhibitors, including escitalopram, should be discontinued.
Escitalopram should be used with caution in patients with a history of mania/hypomania. If a manic state develops, escitalopram should be discontinued.
When treating patients with diabetes mellitus with escitalopram, changes in blood glucose levels may occur. Therefore, dose adjustments of insulin and/or oral hypoglycemic drugs may be required.
Clinical experience with escitalopram and other selective serotonin reuptake inhibitors indicates a possible increased risk of suicide in the first weeks of therapy. Careful monitoring of patients during this period is important.
Hyponatremia, possibly associated with impaired ADH secretion, occurs rarely with escitalopram and usually disappears when therapy is discontinued. Escitalopram and other selective serotonin reuptake inhibitors should be prescribed with caution to patients at risk of developing hyponatremia: the elderly, patients with liver cirrhosis, and those taking drugs that can cause hyponatremia.
When taking escitalopram, skin hemorrhages (ecchymosis and purpura) may develop.
Escitalopram should be used with caution in patients with a tendency to bleed, as well as those taking oral anticoagulants and medications that affect blood clotting.
Clinical experience with the use of escitalopram in combination with electroconvulsive therapy is limited, so caution should be used in this case.
The simultaneous use of escitalopram and MAO type A inhibitors is not recommended due to the risk of developing serotonin syndrome.
In rare cases, patients taking escitalopram and other selective serotonin reuptake inhibitors concomitantly with serotonergic drugs may develop serotonin syndrome.
Escitalopram should be used with caution concomitantly with drugs that have serotonergic effects. A combination of symptoms such as agitation, tremor, myoclonus, and hyperthermia may indicate the development of serotonin syndrome. If this occurs, selective serotonin reuptake inhibitors and serotonergic drugs should be immediately discontinued and symptomatic therapy prescribed.
The simultaneous use of escitalopram and alcohol is not recommended.
Impact on the ability to drive vehicles and operate machinery
Although escitalopram does not affect psychomotor activity, it is not recommended to drive a car or operate machinery during the treatment period.
Active ingredient
Active ingredient
Escitalopram
Composition
Composition
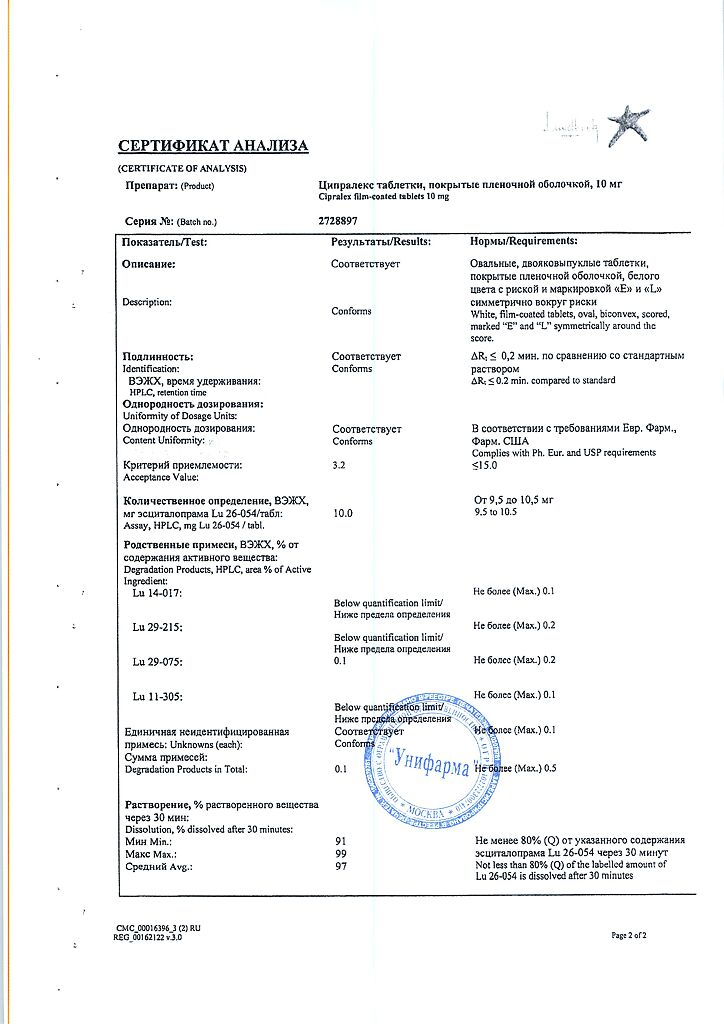
1 tablet contains escitalopram (in oxalate form) 10 mg
Pregnancy
Pregnancy
Cipralex is contraindicated for use during pregnancy and lactation (breastfeeding).
Contraindications
Contraindications
Concomitant use of MAO inhibitors;
Pregnancy;
Lactation period (breastfeeding);
Children under 15 years of age;
Hypersensitivity to escitalopram and other components of the drug.
Side Effects
Side Effects
From the digestive system:
Most often – nausea, loss of appetite, diarrhea, constipation
Rarely – taste disturbances; possible – vomiting, dry mouth, changes in laboratory parameters of liver function.
From the central nervous system and peripheral nervous system:
Most often – insomnia or drowsiness, dizziness, weakness
Possible: visual disturbances, seizures, tremors, movement disorders, serotonin syndrome, hallucinations, mania, confusion, agitation, anxiety, depersonalization, panic attacks, increased irritability
From the side of metabolism:
Most often – increased sweating, hyperthermia
Possibly hyponatremia
From the reproductive system: Most often – decreased libido, impotence, impaired ejaculation, anorgasmia (in women).
From the cardiovascular system: Possible orthostatic hypotension.
From the endocrine system: possible – insufficient secretion of ADH, galactorrhea.
Allergic reactions: possible – anaphylactic reactions, angioedema.
Dermatological reactions: possible – skin rash, itching, ecchymosis, purpura.
Others:
Most often – sinusitis
Possibly – arthralgia, myalgia, urinary retention
If the drug is abruptly discontinued after long-term use, withdrawal reactions are possible – dizziness, headaches and nausea. The severity of these reactions is insignificant, and the duration is limited.
Side effects most often develop at 1 or 2 weeks of treatment and then usually become less intense and occur less frequently as therapy is continued.
Interaction
Interaction
Pharmacodynamic interaction
With the simultaneous use of Cipralex with MAO inhibitors, as well as when starting to take MAO inhibitors in patients who recently stopped taking Cipralex, serious adverse reactions may occur. In such cases, serotonin syndrome may develop.
Concomitant use of Cipralex with serotonergic drugs (for example, tramadol, sumatriptan and other triptans) may lead to the development of serotonin syndrome.
Cipralex may lower the seizure threshold. Caution is required when prescribing Cipralex and other drugs that lower the seizure threshold at the same time.
Since cases of increased effects have been reported when Cipralex is co-administered with lithium or tryptophan, it is recommended to exercise caution when prescribing these drugs simultaneously.
The simultaneous administration of Cipralex and drugs containing St. John’s wort (Hypericum perforatum) may lead to an increase in the number of side effects.
When escitalopram is co-administered with oral anticoagulants and drugs that affect blood clotting (for example, atypical antipsycholeptics and phenothiazines, most tricyclic antidepressants, acetylsalicylic acid and NSAIDs, ticlopidine and dipyridamole), a blood clotting disorder may occur. In such cases, careful monitoring of blood clotting is necessary at the beginning or at the end of therapy with escitalopram.
When taken concomitantly with alcohol, escitalopram does not interact pharmacodynamically or pharmacokinetically. However, as with other psychotropic drugs, the simultaneous use of escitalopram and alcohol is not recommended.
Pharmacokinetic interaction
Concomitant use with drugs that inhibit the CYP2C19 isoenzyme may increase the concentration of escitalopram in the blood plasma. Escitalopram should be used with caution simultaneously with similar drugs (including omeprazole); A dose reduction of escitalopram may be required.
Caution should be exercised when Cipralex is administered in high doses concomitantly with high doses of cimetidine, which is a strong inhibitor of the CYP2D6, CYP3A4 and CYP1A2 isoenzymes.
Escitalopram is an inhibitor of the CYP2D6 isoenzyme. Caution should be exercised when co-prescribing escitalopram and drugs metabolized by this isoenzyme and having a low therapeutic index, for example, flecainide, propafenone and metoprolol (in cases of use in heart failure) or drugs mainly metabolized through the CYP2D6 isoenzyme and acting on the central nervous system, for example the antidepressants desipramine, clomipramine, nortriptyline or antipsychotics risperidone, thioridazine, haloperidol. In these cases, dose adjustment may be required.
The simultaneous administration of escitalopram and desipramine or metoprolol leads to a twofold increase in the concentration of the latter two drugs.
Escitalopram may slightly inhibit the CYP2C19 isoenzyme. Therefore, it is recommended to exercise caution when using escitalopram simultaneously with drugs metabolized by this isoenzyme.
Overdose
Overdose
Symptoms: dizziness, tremor, agitation, drowsiness, confusion, seizures, tachycardia, ECG changes (changes in the ST segment and T wave, widening of the QRS complex, prolongation of the QT interval), arrhythmias, respiratory depression, vomiting, rhabdomyolysis, metabolic acidosis, hypokalemia.
Treatment: There is no specific antidote. Treatment is symptomatic and supportive: gastric lavage, adequate oxygenation. Monitoring the function of the cardiovascular and respiratory systems.
Storage conditions
Storage conditions
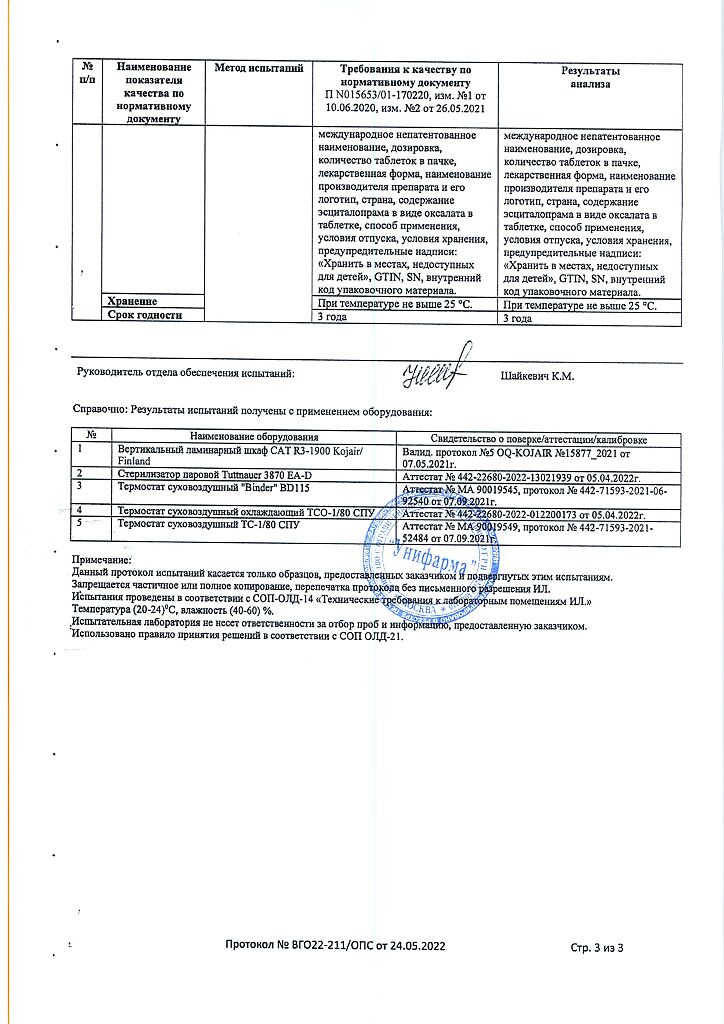
At a temperature not exceeding 25 °C
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
H. Lundbeck A/O, Denmark
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | Х. Lundbeck A/O, Denmark |
| Medication form | pills |
| Brand | Х. Lundbeck A/O |
Other forms…
Related products
Buy Cipralex, 10 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.