No products in the cart.
Celebrex, capsules 100 mg 10 pcs
€19.60 €16.33
Description
Pharmacodynamics
celecoxib has anti-inflammatory, analgesic and antipyretic effects by blocking the formation of inflammatory prostaglandins (Pg) mainly by inhibiting cyclooxygenase-2 (COX-2). Induction of COX-2 occurs in response to inflammation and leads to the synthesis and accumulation of prostaglandins, especially prostaglandin E2, with increased manifestations of inflammation (swelling and pain). In human therapeutic doses, celecoxib does not significantly inhibit cyclooxygenase-1 (COX-1) and has no effect on prostaglandins synthesized as a result of COX-1 activation, and does not affect normal physiological processes connected with COX-1 and running in tissues, especially in stomach, intestine and platelet tissues.
The effect on renal function. Celecoxib reduces urinary excretion of PgE2 and 6-keto-PgF1 (a prostacyclin metabolite), but has no effect on serum thromboxane B2 and urinary excretion of 11-dehydro-thromboxane B2, a thromboxane metabolite (both COX-1 products). Celecoxib does not cause decrease in glomerular filtration rate in elderly patients and persons with chronic renal failure, transiently reduces sodium excretion. In patients with arthritis the observed incidence of peripheral edema, arterial hypertension and heart failure is comparable to that of non-selective COX inhibitors with inhibitory activity against COX-1 and COX-2.
Pharmacokinetics
Absorption. When taken on an empty stomach, celecoxib is well absorbed, reaching maximum concentration (Cmax) in plasma after about 2-3 hours. Cmax in plasma after administration of 200 mg is 705 ng/ml. Absolute bioavailability of the drug has not been studied. Cmax, and area under pharmacokinetic curve “concentration-time” (AUC) are approximately proportional to the dose taken in dose range up to 200 mg twice daily; when using the drug in higher doses the degree of increase in Cmax and AUC is less proportional.
The effect of ingestion. Administration of celecoxib with a fatty meal prolongs the time to reach Cmax by about 1-2 hours and increases total absorption by about 20%. Distribution. Binding with plasma proteins is independent of the concentration and is about 97%, celecoxib does not bind with red blood cells. The drug penetrates through the blood-brain barrier.
Metabolism. celecoxib is metabolized in the liver by hydroxylation, oxidation and partially by glucuronidation. Metabolism mainly occurs with the participation of cytochrome P450 CYP2C9. (See “Interaction with other medicinal products”). The metabolites found in blood are not pharmacologically active against COX-1 and COX-2. Activity of cytochrome P450 CYP2C9 is decreased in persons with genetic polymorphism, such as homozygous for CYP2C9*3 polymorphism, which leads to decreased efficiency of enzymes.
Elimation. Celecoxib is metabolized in liver, excreted with the feces and urine as metabolites (57% and 27%, respectively), less than 3% of the administered dose – unchanged. When repeated use, the elimination half-life is 8-12 hours, and clearance is about 500 ml/min. With repeated use, equilibrium plasma concentrations are reached by day 5. The variability of the main pharmacokinetic parameters (AUC, Cmax, elimination half-life) is about 30%. The average volume of distribution in the equilibrium state is about 400 l.
Special groups
Elderly patients. In patients older than 65 years old there is a 1.5-2-fold increase of the mean values of Cmax, AUC of celecoxib, which is more caused by changes in body weight than by age (elderly patients usually have lower mean body weight than younger patients, due to which they achieve higher celecoxib concentrations, all other conditions being equal). For the same reason, older women usually have higher plasma concentrations than older men. These features of pharmacokinetics usually do not require dose adjustments. However, in elderly patients with body weight below 50 kg, treatment should be started with the lowest recommended dose.
Race. The representative Negro race has an AUC of celecoxib approximately 40% higher than that of Europeans. The reasons and clinical significance of this fact are not known, so it is recommended that their treatment be started with the lowest recommended dose.
Liver function impairment. Plasma concentrations of celecoxib in patients with mild hepatic impairment (Child-Pugh class A) are insignificantly altered. In patients with moderate hepatic impairment (Child-Pugh class B) plasma concentrations of celecoxib may increase by almost 2-fold.
Kidney function impairment. In patients with chronic renal failure with glomerular filtration rate (GFR)>65 ml/min/1.73 m2 and in patients with GFR equal to 35-60 ml/min/1.73 m2 the pharmacokinetics of celecoxib is not changed. No significant relationship is found between serum creatinine (or creatinine clearance) and celecoxib clearance. It is assumed that the presence of severe renal failure does not affect the clearance of celecoxib, since its main route of excretion is transformation in the liver into inactive metabolites.
Indications
Indications
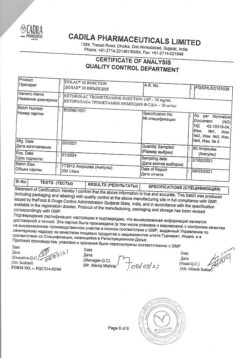
Active ingredient
Active ingredient
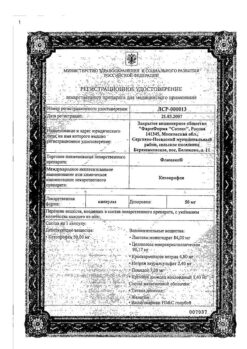
Composition
Composition
1 capsule contains:
the active ingredient:
celecoxib – 100 mg.
excipients:
Lactose monohydrate,
sodium lauryl sulfate,
povidone K30,
croscarmellose sodium and magnesium stearate;
coating:
titanium dioxide, gelatin.
The 100 mg capsule ink (SB-6018 blue ink) contains:
shellac, ethanol, isopropanol, butanol, propylene glycol, ammonia aqueous, FD&C Blue #2 aluminum blue varnish based on indigo-tin dye (E132).
How to take, the dosage
How to take, the dosage
Since the risk of possible cardiovascular complications may increase with increasing dose and duration of Cellebrex administration, it should be prescribed in the shortest possible courses and at the lowest recommended doses. The maximum recommended daily dose for long-term use is 400 mg.
Symptomatic treatment of osteoarthritis: The recommended dose is 200 mg daily in 1 or 2 doses. Doses of up to 400 mg 2 times daily have been observed to be safe. Symptomatic treatment of rheumatoid arthritis: Recommended dose is 100 or 200 mg 2 times daily. The safety of doses up to 400 mg 2 times a day has been noted. Symptomatic treatment of ankylosing spondylitis: The recommended dose is 200 mg daily in 1 or 2 doses. The dose may be increased to 400 mg per day as prescribed by the physician.
Treatment of pain syndrome and primary dysmenorrhea: The recommended initial dose is 400 mg, followed, if necessary, by an additional dose of 200 mg, on the first day. On subsequent days, the recommended dose is 200 mg 2 times daily, as needed.
Elderly patients: No dose adjustment is usually required. However, in patients with body weight less than 50 kg, it is better to start treatment with the lowest recommended dose.
Hepatic impairment: In patients with mild hepatic impairment (Child-Pugh class A), no dose adjustment is required; in patients with moderate hepatic impairment (Child-Pugh class A), treatment should be started with the lowest recommended dose.
Renal dysfunction: In patients with mild to moderate renal insufficiency, no dose adjustment is required. There is no experience of using the drug in patients with severe renal failure.
Simultaneous use with fluconazole: In patients taking fluconazole (CYP2C9 inhibitor), Celebrex should be prescribed in the minimum recommended dose.
Interaction
Interaction
“In vitro” studies have shown that celecoxib, although not a substrate of CYP2D6, but inhibits its activity. Therefore there is a possibility of drug interaction “in vivo” with drugs whose metabolism is associated with cytochrome CYP2D6.
Warfarin and other anticoagulants: simultaneous use may increase prothrombin time.
Fluconazole, ketoconazole: patients taking fluconazole (CYP2C9 inhibitor) celecoxib should be prescribed in the lowest recommended dose, ketoconazole (CYP3A4 inhibitor) has no clinically significant effect on the metabolism of celecoxib.
ACE inhibitors/angiotensin II antagonists: Inhibition of prostaglandin synthesis may reduce the antihypertensive effect of angiotensin converting enzyme inhibitors (ACE)/angiotensin II antagonists. This interaction should be taken into account when prescribing celecoxib together with ACE inhibitors/angiotensin II antagonists. However, no significant pharmacodynamic interaction with lisinopril has been noted with regard to the effect on blood pressure.
Diuretics: Previously known NSAIDs in some patients may decrease the natriuretic effect of furosemide and thiazides by reducing renal prostaglandin synthesis; this should be considered when prescribing celecoxib.
Peroral contraceptives: no clinically significant effect on the pharmacokinetics of the contraceptive combination (1 mg norethisterone/35 mcg ethinylestradiol) has been observed.
Lithium: an increase in plasma lithium concentrations of approximately 17% has been observed when lithium and celecoxib are coadministered. Patients receiving lithium therapy should be closely monitored when prescribing or withdrawing celecoxib.
Other NSAIDs: Concomitant use of celecoxib and other NSAIDs (not containing acetylsalicylic acid) should be avoided.
Other drugs: There were no clinically significant interactions between celecoxib and angacids (aluminum- and magnesium-containing drugs), omeprazole, methotrexate, glibenclamide, phenygoin or tolbutamide.
The celecoxib does not affect the antiplatelet effect of acetylsalicylic acid, so it should not be considered as a substitute for acetylsalicylic acid prescribed to prevent cardiovascular disease.
Special Instructions
Special Instructions
Impacts on the cardiovascular system. celecoxib, like all coxibs, may increase the risk of serious cardiovascular complications such as thrombosis, myocardial infarction, and stroke, which can lead to death. The risk of these reactions may increase with the length of time you take the drug and in patients with cardiovascular disease. To reduce the risk of these reactions in patients taking Celebrex, it should be prescribed in the lowest recommended doses and for the shortest possible periods (at the discretion of the treating physician). The treating physician and the patient should be aware of the possibility of these complications even in the absence of previously known cardiovascular symptoms.
Patients should be informed about the signs and symptoms of adverse cardiovascular events and the steps to take when they occur.
All NSAIDs, including celecoxib, should be used with caution in patients with arterial hypertension. Monitoring of blood pressure should be performed at the beginning of therapy with celecoxib, as well as during the course of treatment.
The effect on the gastrointestinal tract. Very rare cases of gastrointestinal perforation, ulceration and bleeding from the gastrointestinal tract have been observed in patients receiving celecoxib. The risk of developing these complications when treated with NSAIDs is highest in the elderly, patients with cardiovascular disease, patients receiving acetylsalicylic acid at the same time, and patients with such gastrointestinal diseases as ulceration, bleeding in the acute stage and in the history. Most spontaneous reports of serious gastrointestinal side effects have been in elderly and debilitated patients.
Co-use with warfarin and other anti-coagulants. Serious (some of them fatal) bleeding has been reported in patients who received concomitant treatment with warfarin or similar agents. Since an increase in prothrombin time has been reported, anticoagulant activity should be monitored after starting treatment with Celebrex or changing its dose.
Fluid retention and edema. As with other drugs that inhibit prostaglandin synthesis, fluid retention and edema may occur in some patients taking Celebrex, so caution should be exercised when prescribing this drug in patients with conditions that predispose to or are worsened by fluid retention. Patients with a history of heart failure or arterial hypertension should be closely monitored.
The effect on renal function. Celebrex should be used with caution in patients with impaired renal function. Renal function in such patients should be closely monitored.
Caution should be exercised when prescribing therapy with Celebrex in patients with dehydration. In these cases, it is advisable to rehydrate first and then start therapy with Celebrex.
The effect on liver function. Celebrex should be used with caution when treating patients with moderate hepatic impairment and should be administered at the lowest recommended dose.
In some cases, severe liver reactions have been observed, including fulminant hepatitis (sometimes fatal), liver necrosis (sometimes fatal or requiring liver transplantation). Most of these reactions developed 1 month after starting celecoxib.
Patients with symptoms and/or signs of impaired liver function, or those patients in whom impaired liver function is detected by laboratory methods, should be closely monitored for the development of more severe liver reactions during treatment with celecoxib.
Anaphylactic reactions. Cases of anaphylactic reactions have been reported while taking Celebrex.
Celebrex, given its antipyretic effect, may reduce the diagnostic value of a symptom such as fever and affect the diagnosis of infection.
Serious skin reactions. Serious skin reactions such as exfoliative dermatitis, Stevens-Johnson syndrome, and toxic epidermal necrolysis have been extremely rare when taking celecoxib, some of which have been fatal. The risk of such reactions is higher in patients at the beginning of therapy; in most cases noted, such reactions began in the first month of therapy. Cellebrex should be discontinued if skin rash, changes on mucous membranes or other signs of hypersensitivity occur.
The effect of celecoxib on driving and operating machinery has not been studied.
However, based on the pharmacodynamic properties and overall safety profile, it seems unlikely that celebrex has this effect.
Contraindications
Contraindications
Cautions
Side effects
Side effects
Frequent
General: exacerbation of allergic diseases, flu-like syndrome, accidental injury.
Cardiovascular system: peripheral edema.
Gastrointestinal tract: abdominal pain, diarrhea, dyspepsia, flatulence, dental diseases (post-extraction lunate alveolitis).
Nervous system disorders: dizziness, increased muscle tone, insomnia.
Renal and urinary system disorders: urinary tract infection.
Respiratory system: bronchitis, cough, pharyngitis, rhinitis, sinusitis, upper respiratory tract infections.
Skin disorders: skin itching, skin rash.
Infrequent
Blood: anemia, ecchymosis, thrombocytopenia.
Cardiovascular system: worsening of the course of arterial hypertension, increased blood pressure, arrhythmia, “hot flashes”, palpitations, tachycardia.
Sensory organs: tinnitus, blurred vision.
Gastrointestinal tract: vomiting.
Mental status: restlessness, somnolence.
Skin: alopecia, urticaria.
Rarely
Cardiovascular system: manifestation of congestive heart failure, ischemic stroke and myocardial infarction.
Gastrointestinal tract: gastric and duodenal ulcer, esophageal ulceration, intestinal perforation, pancreatitis.
Immune system disorders: angioedema, bullous rash.
Hepatobiliary system: increased activity of “liver” enzymes.
Mental status: confusion.
Side effects identified in post-marketing observations:
Immune system: anaphylaxis.
Mental status: hallucinations.
Nervous system disorders: loss of taste, loss of smell, aseptic meningitis.
Vascular disorders: vasculitis.
Gastrointestinal tract: gastrointestinal bleeding.
Hepatobiliary system disorders: hepatitis, liver failure (see section “Special indications”, “effect on liver function”).
Renal and urinary system disorders: acute renal failure, interstitial nephritis.
Skin disorders: photosensitivity reactions, skin flaking (including erythema multiforme and Stevens-Johnson syndrome), toxic epidermal necrolysis, acute generalized exanthematous pustulosis.
Reproductive system disorders: menstrual cycle disorders.
Overdose
Overdose
Clinical experience with overdose is limited.
Single doses up to 1200 mg and multiple doses up to 1200 mg in 2 doses per day have been used without clinically significant side effects.
If an overdose is suspected, appropriate maintenance therapy should be provided.
Presumably, dialysis is not an effective method of eliminating the drug from the blood because of the high degree of binding of the drug to protein.
Pregnancy use
Pregnancy use
There are insufficient data on the use of celecoxib in pregnant women.
The potential risk of using celecoxib during pregnancy has not been established, but cannot be excluded.
Celecoxib, which belongs to the group of prostaglandin synthesis inhibitors, when taken during pregnancy, especially in the third trimester, may cause weak uterine contractions and premature closure of the arterial duct.
There is limited evidence that celecoxib is excreted with breast milk.
Given the potential for side effects of celecoxib in a breastfed infant, the advisability of continuing breastfeeding should be evaluated, given the importance of taking celebrex to the mother.
Similarities
Similarities
Additional information
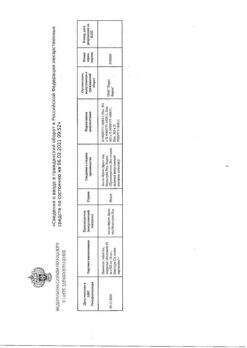
| Weight | 0.017 kg |
|---|---|
| Shelf life | 3 years |
| Conditions of storage | In a dry place, at 15-30 °C |
| Manufacturer | Pfizer, Puerto Rico |
| Medication form | capsules |
| Brand | Pfizer |
Related products
Buy Celebrex, capsules 100 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.