No products in the cart.
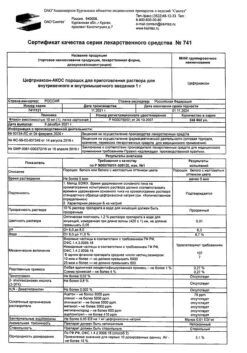
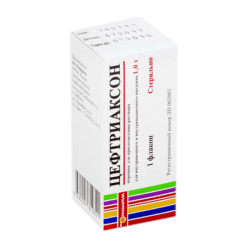
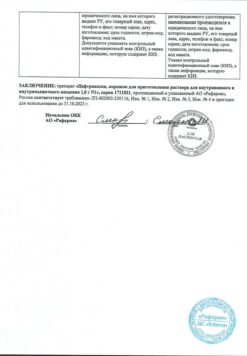
Ceftriaxone-ACOS, 2 g
€2.44 €2.22
Out of stock
(E-mail when Stock is available)
SKU: 501182
Categories: Antibiotics, Medicine
Description
Pharmacotherapeutic group
Cephalosporin antibiotic
ATX code: J01DD04
Pharmacodynamics:
Ceftriaxone is a parenteral cephalosporin III generation antibiotic.
The bactericidal activity of ceftriaxone is due to suppression of cell wall synthesis.
In vitro ceftriaxone has a broad spectrum of action against Gram-negative and Gram-positive micro-granisms. It is highly resistant to most β-lactamases (both penicillinases and cephalosporinases) produced by Gram-positive and Gram-negative bacteria.
Ceftriaxone is generally active against the following microorganisms.
Gram-positive aurebes
Staphylococcus aureus (mticillin-sensitive) coagulase-negative staphylococci Streptococcus pyogenes (β-hemolytic group A) Streptococcus agalactiae (β-hemolytic group B) β-hemolytic streptococci (neither A nor B groups) Streptococcus viridans Streptococcus pneumoniae.
Note. Methicillin-resistant Staphylococcusspp. are resistant to cephalosporins including ceftriaxone. EnterococcusfaecalisEnterococcusfaecium and Listeriamonocytogenes are also generally resistant.
Gram-negative aerobes
AcinetobacterIwoffiiAcinetobacteranitratus (mainly A. baumannii)* AeromonashydrophilaAlcaligenesfaecalisAlcaligenesodorans alkaligen-like bacteria BorreliaburgdorferiCapnocytophagaspp. Citrobacterdiversus (including C. amalonaticus) Citrobacterfreundii* EscherichiacoliEnterobacteraerogenes* Enterobactercloacae* Enterobacterspp. (others)* HaemophilusducreyiHaemophilusinfluenzaeHaemophilusparainfluenzaeHafniaalveiKlebsiellaoxytocaKlebsiellapneumoniae** Moraxellacatarrhalis (previously called Branhamellacatarrhalis) MoraxellaosloensisMoraxellaspp. (others) Morganella morganii Neisseria gonorrhoeae. Neisseria meningitidis Pasteurella multocida Plesiomonas shigelloides Proteus mirabilis Proteus penneri* Proteus vulgaris* Pseudomonas fluorescens* Pseudomonas spp. (other) Providencia rettgeri* Providencia spp. (other) Salmonella typhi Salmonella spp. (nontyphoid) Serratia marcescens* Serratia spp. (other)* Shigella spp. Vibrio spp. Yersinia enterocolitica Yersinia spp. (others).
* Some isolates of these species are resistant to ceftriaxone mainly due to the formation of β-lactamases encoded by chromosomes.
** Some isolates of these species are resistant due to the formation of a variety of plasmid-mediated β -lactamases.
Note. Many strains of the above microorganisms are multiresistant to other antibiotics such as aminopenicillins and ureidonecillins first and second generation cephalosporins and aminoglycosides are sensitive to ceftriaxone. Treponoma pallidum is sensitive to ceftriaxone in vitro and in animal experiments. Clinical trials show that ceftriaxone has good efficacy against primary and secondary syphilis. With very few exceptions, clinical isolates of P.aeruginosa are resistant to ceftriaxone.
The anaerobes
Bacteroidesspp. (bile-sensitive)* Clostridiumspp. (except C. difficile) Fusobacterium nucleatum Fusobacterium spp. (other) Gaffkya anaerobica (formerly called Peptococcus) Peptostreptococcus spp.
* Some isolates of these species are resistant to ceftriaxone because of the formation of β-lactamases. Note. Many strains of β-lactamase-producing Bacteroidesspp. (particularly B. fragilis) are resistant. Clostridiumdifficile is also resistant.
Sensitivity to ceftriaxone can be determined by disc-diffusion or serial dilution on agar or broth using a standard methodology similar to that recommended by the Institute of Clinical and Laboratory Standards (ICLS).
Ceftriaxone discs should be used for determination because in vitro studies have shown that ceftriaxone is active against specific strains that show resistance when discs for the entire group of cephalosporins are used.
In place of the ICLS standards, other well-standardized guidelines can be used to recommend the sensitivity of microorganisms, for example DIN (Deutsches Institut für Normung) and ICS (International Collaborative Study) guidelines that allow an adequate interpretation of the sensitivity status.
Pharmacokinetics:
The pharmacokinetics of ceftritaxone are non-linear. All major pharmacokinetic parameters based on total drug concentrations with the exception of the elimination half-life are dose-dependent and increase in less than proportional proportion to its increase. Nonlinearity is characteristic for pharmacokinetic parameters depending on the total concentration of ceftriaxone in blood plasma (not only free ceftriaxone) and is explained by saturation of binding of the drug to blood plasma proteins.
Intake
The maximum plasma concentration after a single intramuscular administration of 1 g of the drug is about 81 mg/l and is reached within 2-3 hours after administration. The areas under the curve “plasma concentration – time” after intravenous and intramuscular administration are the same. This means that bioavailability of ceftriaxone after intramuscular administration is 100%.
After intravenous bolus administration of 500 mg and 1 g of ceftriaxone average maximum plasma concentrations were 120 mg/l and 200 mg/l, respectively. After intravenous infusion of 500 mg of 1 g and 2 g of ceftriaxone, the plasma concentrations of the drug were approximately 80,150 and 250 mg/L, respectively. After intramuscular injection, mean maximum plasma ceftriaxone concentrations were approximately twice as low as after intravenous administration of an equivalent dose of the drug.
Distribution
The volume of distribution of ceftriaxone is 7-12 liters. After administration in a dose of 1-2 g ceftriaxone penetrates well into tissues and body fluids. For more than 24 hours, its concentrations far exceed the minimal suppressive concentrations for most infectious agents in more than 60 tissues and fluids (including lungs, heart, biliary tracts, liver, tonsils, middle ear and nasal mucosa, bones, and cerebrospinal pleural and synovial fluid and prostate secretion).
After intravenous administration ceftriaxone rapidly penetrates into the cerebrospinal fluid where bactericidal concentrations against susceptible microorganisms persist for 24 hours.
Protein binding
Ceftriaxone binds reversibly to albumin. The degree of binding is approximately 95% with values of ceftriaxone concentration in plasma of at least 100 mg/l.
For ceftriaxone bound to plasma protein increases with increasing concentration as the binding is saturable and is about 85% at plasma concentration values of 300 mg/l.
Perfusion to selected tissues
Ceftriaxone penetrates the brain membranes to the greatest extent when they are inflamed. The average maximum concentration of ceftriaxone in the cerebrospinal fluid reaches 25% of the plasma concentration of ceftriaxone in patients with bacterial meningitis and only 2% of the plasma concentration in patients with non-inflamed cerebral membranes. The maximum concentration of ceftriaxone in the cerebrospinal fluid is reached 4-6 hours after its intravenous administration. Ceftriaxone passes through the placental barrier and passes in low concentrations into breast milk.
Metabolism
Ceftriaxone does not undergo systemic metabolism but is converted into inactive metabolites by the intestinal microflora.
The total plasma clearance of ceftriaxone is 10-22 ml/min. Renal clearance is 5-12 ml/min. 50-60% of ceftriaxone is excreted unchanged by the kidneys and 40-50% is excreted unchanged by the intestine. The half-life of ceftriaxone in adults is about 8 hours.
Pharmacokinetics in special clinical cases
Newborn infants and children younger than 12 years
In newborn children the half-life of ceftriaxone is longer compared to other age groups. During the first 14 days of life, plasma concentrations of free ceftriaxone may be further increased due to low glomerular filtration and features of the drug binding to blood plasma proteins. In pediatric patients the half-life is shorter than in newborns and adults.
The values of plasma clearance and volume of distribution of total ceftriaxone are higher in newborn infants and children younger than 12 years compared to those in adults.
Patients with impaired renal or hepatic function have little change in the pharmacokinetics of ceftriaxone with only a slight increase in the half-life (less than 2-fold), even in patients with severe renal impairment.
The slight increase of ceftriaxone half-life in renal failure can be explained by compensatory increase of nonrenal clearance as a result of decrease of plasma protein binding and corresponding increase of total ceftriaxone nonrenal clearance.
In patients with hepatic insufficiency the half-life is not increased. In these patients there is a compensatory increase in renal clearance. This is also due to the increased plasma concentration of free ceftriaxone which contributes to a paradoxical increase of total drug clearance against the background of increased volume of distribution.
Patients of advanced age
The elimination half-life is, on average, two to three times longer in patients over 75 years of age than in adult patients.
Indications
Indications
Infections caused by pathogens sensitive to ceftriaxone: sepsis; meningitis; disseminated Lyme disease (stages II and III of the disease); infections of the abdominal organs (peritonitis, infections of the biliary tract and gastrointestinal tract); infections of bones, joints, soft tissues of the skin, as well as wound infections; infections in immunocompromised patients; kidney and urinary tract infections; respiratory tract infections especially pneumonia and ENT infections; genital infections including gonorrhea.
Perioperative prevention of infections.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Antibiotic-cephalosporin
ATX code: J01DD04
Pharmacodynamics:
Ceftriaxone is a parenteral cephalosporin antibiotic of the third generation.
The bactericidal activity of ceftriaxone is due to the suppression of cell wall synthesis.
In vitro, ceftriaxone has a broad spectrum of action against gram-negative and gram-positive microorganisms. It is highly resistant to most β-lactamases (both penicillinases and cephalosporinases) produced by gram-positive and gram-negative bacteria.
Ceftriaxone is usually active against the following microorganisms.
Gram-positive aerobes
Staphylococcus aureus (msticillin-sensitive) coagulase-negative staphylococci Streptococcus pyogenes (β-hemolytic group A) Streptococcus agalactiae (β-hemolytic group B) β-hemolytic streptococci (group neither A nor B) Streptococcus viridans Streptococcus pneumoniae.
Note. Methicillin-resistant Staphylococcus spp. resistant to cephalosporins, including ceftriaxone. As a rule, Enterococcus faecalis Enterococcus faecium and Listeria monocytogenes are also resistant.
Gram-negative aerobes
AcinetobacterIwoffiiAcinetobacteranitratus (mainly A. baumannii)* AeromonashydrophilaAlcaligenesfaecalisAlcaligenesodorans alkaligen-like bacteria BorreliaburgdorferiCapnocytophagaspp. Citrobacterdiversus (including C. amalonaticus) Citrobacterfreundii* Escherichia coliEnterobacteraerogenes* Enterobactercloacae* Enterobacterspp. (others)* HaemophilusducreyiHaemophilusinfluenzaeHaemophilusparainfluenzaeHafniaalveiKlebsiellaoxytocaKlebsiellapneumoniae** Moraxellacatarrhalis (formerly called Branhamellacatarrhalis) MoraxellaosloensisMoraxellaspp. (other) Morganella morganii Neisseria gonorrhoeae. Neisseria meningitidis Pasteurella multocida Plesiomonas shigelloides Proteus mirabilis Proteus penneri* Proteus vulgaris* Pseudomonas fluorescens* Pseudomonas spp. (other) Providencia rettgeri* Providencia spp. (other) Salmonella typhi Salmonella spp. (non-typhoid) Serratia marcescens* Serratia spp. (other)* Shigella spp. Vibrio spp. Yersinia enterocolitica Yersinia spp. (others).
* Some isolates of these species are resistant to ceftriaxone, mainly due to the production of chromosomally encoded β-lactamases.
** Some isolates of these species are resistant due to the formation of a number of plasmid-mediated β-lactamases.
Note. Many strains of the above microorganisms are multiresistant to other antibiotics such as aminopenicillins and ureidonenicillins, first and second generation cephalosporins and aminoglycosides and are sensitive to ceftriaxone. Treponoma pallidum is sensitive to ceftriaxone in vitro and in animal experiments. Clinical trials show that ceftriaxone has good efficacy against primary and secondary syphilis. With very few exceptions, clinical isolates of P. aeruginosa are resistant to ceftriaxone.
Anaerobes
Bacteroidessp. (bile sensitive)* Clostridium spp. (except C. difficile) Fusobacterium nucleatum Fusobacterium spp. (others) Gaffkya anaerobica (formerly called Peptococcus) Peptostreptococcus spp.
* Some isolates of these species are resistant to ceftriaxone due to the formation of β-lactamases. Note. Many strains of β-lactamase-forming Bacteroidesspp. (in particular B. fragilis) are resistant. Clostridium difficile is also resistant.
Susceptibility to ceftriaxone can be determined by the disk diffusion method or by the serial dilution method on agar or broth using a standard technique similar to that recommended by the Clinical and Laboratory Standards Institute (CLSI).
For determination, you should take disks with ceftriaxone, since in vitro studies have shown that ceftriaxone is active against certain strains that show resistance when using disks intended for the entire group of cephalosporins.
Instead of ICLS standards, to recommend determining the sensitivity of microorganisms, you can use other well-standardized standards, for example, the German Institute for Standardization DIN (Deutsches Institut fur Normung) and international recommendations ICS (International Collaborative Study) that allow you to adequately interpret the state of sensitivity.
Pharmacokinetics:
The pharmacokinetics of ceftritaxone is nonlinear. All major pharmacokinetic parameters based on total drug concentrations, with the exception of the half-life, are dose dependent and increase less than proportionally with dose. Nonlinearity is characteristic of pharmacokinetic parameters that depend on the total concentration of ceftriaxone in the blood plasma (not only free ceftriaxone) and is explained by the saturation of the binding of the drug to plasma proteins.
Suction
The maximum concentration in plasma after a single intramuscular injection of 1 g of the drug is about 81 mg/l and is achieved within 2-3 hours after administration. The areas under the plasma concentration-time curve after intravenous and intramuscular administration are the same. This means that the bioavailability of ceftriaxone after intramuscular administration is 100%.
After intravenous bolus administration of 500 mg and 1 g of ceftriaxone, the mean maximum plasma concentration was 120 mg/L and 200 mg/L, respectively. After intravenous infusion of 500 mg of ceftriaxone 1 g and 2 g, the drug concentration in the blood plasma was approximately 80,150 and 250 mg/L, respectively. After intramuscular injection, the average maximum concentration of ceftriaxone in the blood plasma is approximately two times lower than after intravenous administration of an equivalent dose of the drug.
Distribution
The volume of distribution of ceftriaxone is 7-12 liters. After administration in a dose of 1-2 g, ceftriaxone penetrates well into tissues and body fluids. Over a period of more than 24 hours, its concentrations far exceed the minimum inhibitory concentrations for most infectious agents in more than 60 tissues and fluids (including the lungs, heart, bile ducts, liver, tonsils, middle ear and nasal mucosa, bones, as well as cerebrospinal pleural and synovial fluids and prostate secretions).
After intravenous administration, ceftriaxone quickly penetrates into the cerebrospinal fluid where bactericidal concentrations against sensitive microorganisms are maintained for 24 hours.
Protein binding
Ceftriaxone binds reversibly to albumin. The degree of binding is approximately 95% at ceftriaxone plasma concentrations of at least 100 mg/l.
For protein-bound blood plasma, ceftriaxone decreases with increasing concentration since binding is saturable and is about 85% at concentration values of 300 mg/l.
Penetration into individual tissues
Ceftriaxone penetrates the meninges to the greatest extent when they are inflamed. The mean maximum concentration of ceftriaxone in the cerebrospinal fluid reaches 25% of the plasma concentration of ceftriaxone in patients with bacterial meningitis and only 2% of the plasma concentration in patients with non-inflamed meninges. The maximum concentration of ceftriaxone in the cerebrospinal fluid is achieved 4-6 hours after its intravenous administration. Ceftriaxone passes through the placental barrier and enters breast milk in low concentrations.
Metabolism
Ceftriaxone does not undergo systemic metabolism and is converted into inactive metabolites under the influence of intestinal microflora.
Removal
The total plasma clearance of ceftriaxone is 10-22 ml/min. Renal clearance is 5-12 ml/min. 50-60% of ceftriaxone is excreted unchanged by the kidneys and 40-50% is excreted unchanged by the intestines. The half-life of ceftriaxone is approximately 8 hours in adults.
Pharmacokinetics in special clinical situations
Newborn infants and children under 12 years of age
In newborns, the half-life of ceftriaxone is increased compared to other age groups. In the first 14 days of life, the concentration of free ceftriaxone in the blood plasma can be further increased due to low glomerular filtration and the peculiarities of the drug binding to plasma proteins. In pediatric patients, the half-life is shorter than in neonates and adults.
The values of plasma clearance and volume of distribution of total ceftriaxone are higher in newborn infants and children under 12 years of age compared to those in adults.
Impaired kidney or liver function
In patients with impaired renal or hepatic function, the pharmacokinetics of ceftriaxone changes slightly, with only a slight increase in the half-life (less than 2 times) even in patients with severe renal impairment.
The slight increase in the half-life of ceftriaxone in renal failure may be explained by a compensatory increase in non-renal clearance as a result of a decrease in the degree of binding to plasma proteins and a corresponding increase in non-renal clearance of total ceftriaxone.
In patients with hepatic impairment, the half-life does not increase. In such patients, a compensatory increase in renal clearance occurs. The reason is also an increase in the concentration of free ceftriaxone in the blood plasma, which contributes to a paradoxical increase in the overall clearance of the drug against the background of an increase in the volume of distribution.
Elderly patients
In patients over 75 years of age, the half-life is on average two or three times longer than in adult patients.
Special instructions
Special instructions
Hypersensitivity reactions
As with other β-lactam antibiotics, severe hypersensitivity reactions, including fatal ones, have been reported. If a severe hypersensitivity reaction develops, therapy with Ceftriaxone-AKOS should be immediately discontinued and appropriate emergency treatment measures taken. Before starting therapy with Ceftriaxone-AKOS, it is necessary to determine whether the patient has had hypersensitivity reactions to ceftriaxone, cephalosporins or severe hypersensitivity reactions to other β-lactam antibiotics (penicillin monobactams and carbapenems).
Caution should be exercised when using ceftriaxone in patients with a history of mild hypersensitivity reactions to other β-lactam antibiotics (penicillin monobactams and carbapenems).
Severe life-threatening or fatal skin hypersensitivity reactions (Stevens-Johnson syndrome or Lyell’s syndrome/toxic epidermal necrolysis) and drug reaction with eosinophilia and systemic symptoms (DRESS syndrome) have been reported. The frequency of such reactions is unknown.
Shortly after treatment with ceftriaxone, some patients with spirochete infection may experience a Jarisch-Herxheimer reaction (JHR). The reaction usually goes away on its own or can be managed with symptomatic treatment.
If a reaction occurs, antibiotic treatment should not be stopped.
Sodium content
1 g of Ceftriaxone-AKOS contains 36 mmol of sodium. This should be taken into account by patients on a sodium controlled diet.
Hemolytic anemia
As with the use of other cephalosporins, the development of autoimmune hemolytic anemia during treatment with Ceftriaxone-AKOS is possible. Cases of severe hemolytic anemia have been reported in adults and children, including deaths. If anemia develops in a patient being treated with ceftriaxone, the diagnosis of cephalosporin-associated anemia cannot be excluded and treatment must be discontinued until the cause is determined.
Diarrhea caused by Clostridium difficile
As with the use of most other antibacterial drugs, cases of diarrhea caused by Clostridium difficile (C. difficile) of varying severity have been reported during treatment with ceftriaxone: from mild diarrhea to fatal colitis. Treatment with antibacterial drugs suppresses the normal microflora of the colon and provokes the growth of C. difficile. In turn, C. difficile produces toxins A and B, which are factors in the pathogenesis of diarrhea caused by C. difficile. Toxin-overproducing strains of C. difficile are infectious agents with a high risk of morbidity and mortality due to possible resistance to antimicrobial therapy and treatment may require colectomy. It is necessary to remember the possibility of developing diarrhea caused by C. difficile in all patients with diarrhea after antibiotic therapy. A thorough history taking is necessary because There have been cases of diarrhea caused by C. difficile occurring more than 2 months after antibiotic therapy. If diarrhea due to C. difficile is suspected or confirmed, current non-C. difficile antibiotic therapy may need to be discontinued. In accordance with clinical indications, appropriate treatment should be prescribed with the introduction of fluids and electrolytes, proteins, antibiotic therapy for C. difficile, surgical treatment. You cannot use drugs that inhibit intestinal perilstatitis.
Superinfections
As with treatment with other antibacterial drugs, superinfections may develop.
Changes in prothrombin time
Rare cases of changes in prothrombin time have been described in patients receiving Ceftriaxone-AKOS. Patients with vitamin K deficiency (impaired synthesis and nutritional disorder) may require monitoring of prothrombin time during therapy and administration of vitamin K (10 mg/week) if prothrombin time increases before or during therapy.
Formation of precipitates of ceftriaxone calcium salt
Cases of fatal reactions resulting from the deposition of ceftriaxone-calcium precipitates in the lungs and kidneys of newborns have been described. Theoretically, there is a possibility of interaction of ceftriaxone with calcium-containing solutions for intravenous administration in other age groups of patients; therefore, ceftriaxone should not be mixed with calcium-containing solutions (including for parenteral nutrition) and should not be administered simultaneously, including through separate accesses for infusions at different sites. Theoretically, based on the calculation of the 5 half-lives of ceftriaxone, the interval between the administration of ceftriaxone and calcium-containing solutions should be at least 48 hours.
There are no data on the possible interaction of ceftriaxone with calcium-containing drugs for oral administration, as well as ceftriaxone for intramuscular administration with calcium-containing drugs (intravenously or orally). After using ceftriaxone, usually in doses exceeding the standard recommended (1 g per day or more), ultrasound examination of the gallbladder revealed precipitates of the calcium salt of ceftriaxone, the formation of which is most likely in pediatric patients. Precipitates rarely cause any symptoms and disappear after completion or cessation of therapy with Ceftriaxone-AKOS. If these phenomena are accompanied by clinical symptoms, conservative non-surgical treatment is recommended, and the decision to discontinue the drug is left to the discretion of the attending physician and should be based on an individual assessment of the benefits and risks.
Despite the presence of data on the formation of intravascular precipitates only in newborns when using Ceftriaxone and calcium-containing infusion solutions of any other calcium-containing drugs. The drug Ceftriaxone-AKOS should not be mixed or prescribed to children and adult patients simultaneously with calcium-containing infusion solutions, even using different venous accesses (see sections “Contraindications”, “Interaction with other drugs”, subsection “Post-registration surveillance”).
Pancreatitis
In patients receiving the drug Ceftriaxone-AKOS, rare cases of pencreatitis that developed, possibly due to obstruction of the biliary tract, have been described. Most of these patients already had risk factors for bile duct congestion, such as previous therapy, severe illness and complete parenteral nutrition. At the same time, it is impossible to exclude the triggering role in the development of pancreatitis of precipitates formed under the influence of the drug Ceftriaxone-AKOS in the biliary tract.
Use in children
The safety and effectiveness of Ceftriaxone-AKOS in newborn infants and young children have been determined for the dosages described in the section “Dosage and Administration”. Studies have shown that, like other cephalosporins, ceftriaxone can displace bilirubin from binding to serum albumin.
The drug Ceftriaxone-AKOS should not be used in newborns, especially premature ones, who are at risk of developing bilirubin encephalopathy (see section “Contraindications”)
Long-term treatment
With long-term treatment, it is necessary to regularly monitor the peripheral blood picture and indicators of the functional state of the liver and kidneys.
Blood test monitoring
During long-term treatment, a complete blood count should be performed regularly.
Serological studies
When treated with ceftriaxone, false-positive results of the Coombs test for galactosemia may be observed when determining glucose in the urine (glucosuria is recommended to be determined only by the enzyme method).
Impact on the ability to drive vehicles. Wed and fur.:
There is no data indicating the effect of the drug on driving vehicles and working with machines and mechanisms. However, during therapy with Ceftriaxone-AKOS, caution should be exercised when driving vehicles and operating machinery due to the possibility of dizziness and other undesirable reactions that may affect the ability to operate vehicles with machinery.
Active ingredient
Active ingredient
Ceftriaxone
Composition
Composition
One bottle of powder for preparing a solution for intravenous and intramuscular administration contains:
Active ingredient: ceftriaxone sodium – 2.142 g (in terms of ceftriaxone – 2 g).
Pregnancy
Pregnancy
Pregnancy
Ceftriaxone penetrates the placental barrier. Safety of use during pregnancy in women has not been established. Preclinical studies of reproduction did not reveal embryotoxic fetotoxic teratogenic effects or other adverse effects of the drug on the fertility of males and females, the process of childbirth, perinatal and postnatal development of the fetus. During pregnancy, especially in the first trimester, it should be prescribed only according to strict indications, provided that the expected benefit to the mother outweighs the potential risk to the fetus.
Breastfeeding period
Ceftriaxone passes into breast milk in low concentrations. The effect of ceftriaxone on a breastfed child is unlikely when it is used by the mother in therapeutic doses; however, the risk of developing diarrhea, fungal infections of the mucous membranes and hypersensitivity reactions in the child cannot be excluded.
It is necessary to stop breastfeeding or discontinue/abstain from ceftriaxone therapy, taking into account the benefits of breastfeeding for the child and the benefit of therapy for the mother.
Contraindications
Contraindications
Hypersensitivity
Hypersensitivity to ceftriaxone and any other component of the drug.
Hypersensitivity to cephalosporins.
History of severe hypersensitivity reactions (eg anaphylactic reactions) to other β-lactam antibiotics (penicillin monobactams and carbapenems).
Premature babies
For premature infants up to 41 weeks of age inclusive (combined gestational and chronological age), the use of ceftriaxone is contraindicated.
Term newborns (<28 days of age)
Hyperbilirubinemia jaundice or acidosis hypoalbuminemia in newborns (in vitro studies have shown that ceftriaxone may displace bilirubin from binding to serum albumin, increasing the risk of developing bilirubin encephalopathy in these patients).
Intravenous administration of potassium-containing solutions to newborns.
Newborns (≤28 days) who are already prescribed or are expected to be treated intravenously with calcium-containing solutions, including continuous calcium-containing infusions, such as with parenteral nutrition, due to the risk of the formation of precipitates of ceftriaxone calcium salts (see sections “Dosage and Administration” and “Interaction with other medicinal products”).
Isolated fatal cases of the formation of precipitates in the lungs and kidneys in newborns receiving ceftriaxone and calcium-containing solutions have been described. Moreover, in some cases, one venous access was used and the formation of precipitates was observed directly in the intravenous system; at least one case with a fatal outcome was described with different venous accesses and at different times of administration of ceftriaxone and calcium-containing solutions. Similar cases were observed only in newborns (see subsection “Post-registration surveillance”).
Lidocaine
Before performing an intramuscular injection of ceftriaxone using lidocaine, it is necessary to exclude the presence of contraindications to lidocaine. Contraindications to the use of lidocaine are given in the instructions for medical use of lidocaine. Ceftriaxone solutions containing lidocaine should not be administered intravenously.
With caution:
Breastfeeding period.
History of mild hypersensitivity reactions to other β-lactam antibiotics (penicillin monobactams and carbapenems).
Side Effects
Side Effects
The most common adverse reactions reported during ceftriaxone therapy in clinical trials are eosinophilia, leukopenia, thrombocytopenia, diarrhea, rash, and increased liver enzymes.
The following classification is used to describe the frequency of adverse reactions: very common (≥1/10) common (≥1/100 and <1/10) uncommon (≥1/1000 and <1/100) rare (≥1/10000 and <1/1000) and very rare (<1/10000) including isolated cases.
Adverse reactions are grouped according to MedDRA Medical Dictionary of Regulatory Organ System classes.
Infectious and parasitic diseases: infrequently – mycoses of the genital organs; rarely – pseudomembranous colitis.
Disorders of the blood and lymphatic system: often – eosinophilia, leukopenia, thrombocytopenia; uncommon – granulocytopenia, anemia, coagulopathy.
Nervous system disorders: uncommon – headache and dizziness.
Disorders of the respiratory system of the chest and mediastinum: rarely – bronchospasm.
Gastrointestinal disorders: often – diarrhea, unformed stools; infrequently nausea vomiting.
Disorders of the liver and biliary tract: often – increased activity of liver enzymes (aspartate aminotransferase (ATS), alanine aminotransferase (ALT), alkaline phosphatase (ALP)).
Disorders of the skin and subcutaneous tissues: often – rash; infrequently – itching; rarely – urticaria.
Renal and urinary tract disorders: rarely – hematuria, glucosuria.
General disorders and disorders at the injection site: infrequently – phlebitis, pain at the injection site, increased body temperature; rarely – swelling, chills.
Impact on the results of laboratory and instrumental studies: infrequently – an increase in the concentration of creatinine in the blood.
Post-registration surveillance
The following describes the side effects observed with the use of the drug Ceftriaxone-AKOS in the post-registration period. Determining the frequency of observed side effects and their relationship with the use of the drug Ceftriaxone-AKOS is not always possible since it is impossible to establish the exact size of the patient population.
Gastrointestinal disorders: pancreatitis, stomatitis, glossitis, taste disturbance.
Blood disorders of the lymphatic system: thrombocytosis, increased thromboplastin and prothrombin time, decreased prothrombin time, hemolytic anemia. Isolated cases of agranulocytosis (<500 cells/µl) have been described, most of them developing after 10 days of treatment and the use of a cumulative dose of 20 g or more.
Immune system disorders: anaphylactic shock, hypersensitivity reaction, Jarisch-Herxheimer reaction.
Skin and subcutaneous tissue disorders: acute generalized exanthematous pustulosis, isolated cases of severe adverse reactions (exudative erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis (Lyell’s syndrome), drug reaction with eosinophilia and systemic symptoms (DRESS syndrome).
Nervous system disorders: seizures.
Hearing and labyrinthine disorders: vertigo.
Infectious and parasitic diseases: superinfections.
The following undesirable reactions are also known: the formation of precipitates of calcium salts of cefritaxone in the gallbladder with corresponding symptoms; bilirubin encephalopathy hyperbilirubinemia oliguria vaginitis increased sweating “hot flashes” allergic pneumonitis nosebleeds jaundice palpitations serum sickness as well as anaphaylactic or anaphylactoid reactions.
Isolated fatal cases of the formation of precipitates in the lungs and kidneys have been described based on the results of an autopsy study in newborns receiving cefritaxone and potassium-containing solutions. In some cases, a single venous access was used and the formation of precipitates was observed directly in the intravenous system. At least one case of death has also been described using different venous approaches and at different times of administration of ceftriaxone and calcium-containing solutions. However, according to the results of the autopsy study, no precipitates were found in this newborn. Similar cases were observed only in newborns (see section “Special instructions”).
Cases of the formation of ceftriaxone precipitates in the urinary tract have been reported, mainly in children who received either large daily doses of the drug (≥80 mg/kg per day) or cumulative doses of more than 10 g, as well as those who had additional risk factors (dehydration, bed rest). The formation of precipitates in the kidneys may be asymptomatic or clinically manifest and can lead to ureteral obstruction and postrenal acute renal failure. This adverse event is reversible and disappears after discontinuation of therapy with Ceftriaxone-AKOS.
General disorders and disorders at the injection site: phlebitis after intravenous administration. This can be avoided by injecting the drug slowly over 5 minutes, preferably into a large vein.
Intramuscular injection without lidocaine is painful.
Impact on laboratory test results
When treated with Ceftriaxone-AKOS, patients may experience false-positive Coombs test results. Like other antibiotics, Ceftriaxone-AKOS can give a false-positive test result for galactosemia. False-positive results can also be obtained when determining glucose in urine using non-enzymatic methods; therefore, during therapy with Ceftriaxone-AKOS, glucosuria, if necessary, should be determined only by the enzymatic method.
Ceftriaxone may cause an unreliable decrease in blood glucose values measured using some blood glucose monitoring devices. See the instructions for use of the device you are using. If necessary, alternative methods for determining blood glucose should be used.
Interaction
Interaction
With the simultaneous use of large doses of Ceftriaxone-AKOS and “loop” diuretics (for example, furosemide), renal dysfunction was not observed. There is conflicting data on the likelihood of increased nephrotoxicity of aminoglycosides when used with cephalosporins; therefore, it is necessary to monitor renal function and the concentration of aminoglycosides in the blood. Drinking alcohol after administration of Ceftriaxone-AKOS was not accompanied by a disulfiram-like reaction. Ceftriaxone does not contain an N-methylthiotetrazole group, which could cause ethanol intolerance and bleeding, which is inherent in some other cephalosporins. Probenecid does not affect the elimination of Ceftriaxone-AKOS.
Bacteriostatic antibiotics reduce the bactericidal effect of ceftriaxone.
In vitro antagonism was found between chloramphenicol and ceftriaxone.
Solvents containing calcium such as Ringer’s solution or Hartmann’s solution should not be used when preparing solutions of Ceftriaxone-AKOS for intravenous administration and their subsequent dilution due to the possible formation of precipitates. The formation of precipitates of ceftriaxone calcium salts can also occur when mixing the drug Ceftriaxone-AKOS and calcium-containing solutions when using the same venous access. Ceftriaxone should not be used simultaneously with calcium-containing solutions for intravenous administration, including long-term infusions of calcium-containing solutions, such as parenteral nutrition using a Y-connector.
For all groups of patients except newborns, sequential administration of ceftriaxone and calcium-containing solutions is possible with thorough rinsing of the infusion systems between infusions with a compatible liquid. To evaluate the interaction of Ceftriaxone and calcium concentrations, two in vitro studies were conducted, one using adult blood plasma and the other using newborn umbilical cord blood plasma. Various combinations of ceftriaxone with an initial concentration of up to 1 mM (the maximum concentration that ceftriaxone reaches in vivo when 2 g of the drug is infused over at least 30 minutes) and calcium with an initial concentration of up to 12 mM (48 mg/dL) were analyzed.
A decrease in the concentration of ceftriaxone in plasma was observed when using calcium at a concentration of 6 mM (24 mg/dL) and higher for the plasma of an adult and at a concentration of 4 mM (16 mg/dL) and higher for the plasma of a newborn, indicating an increased risk of the formation of calcium salts of ceftriaxone in newborns (see sections “Dosage and Administration” and “Contraindications”).
Ceftriaxone is pharmaceutically incompatible with amsacrine, vancomycin, fluconazole and aminoglycosides.
When using vitamin K antagonists during therapy with Ceftriaxone-AKOS, the risk of bleeding increases. Blood coagulation parameters should be constantly monitored and, if necessary, the dose of the anticoagulant should be adjusted both during and after the end of therapy with Ceftriaxone-AKOS.
Synergism between ceftriaxone and aminoglycosides has been shown against many gram-negative bacteria. Although the increased effectiveness of such combinations is not always predictable, it should be kept in mind in severe life-threatening infections such as those caused by Pseudomonasaeruginosa.
Overdose
Overdose
Symptoms
Nausea, vomiting and diarrhea.
Treatment
In case of overdose, hemodialysis and peritoneal dialysis will not reduce drug concentrations. There is no specific antidote. Treatment of overdose is symptomatic.
Storage conditions
Storage conditions
In a place protected from light at a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years. Do not use after expiration date.
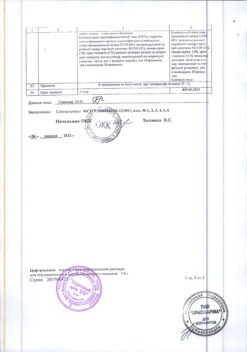
Manufacturer
Manufacturer
Sintez, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In the dark place at a temperature not exceeding 25 °C. Store out of the reach of children. |
| Manufacturer | Sintez OAO, Russia |
| Medication form | Powder for preparation of solution |
| Brand | Sintez OAO |
Other forms…
Related products
Buy Ceftriaxone-ACOS, 2 g with delivery to USA, UK, Europe and over 120 other countries.