No products in the cart.
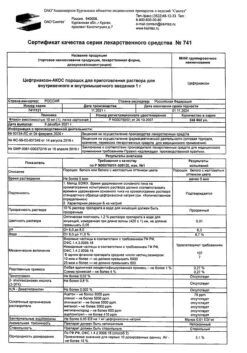
Ceftriaxone, 1 g
€1.88 €1.71
Out of stock
(E-mail when Stock is available)
Description
Infections caused by pathogens sensitive to ceftriaxone: sepsis; meningitis; disseminated Lyme disease (stage II and III disease); abdominal organ infections (peritonitis, biliary tract and gastrointestinal tract infections); infections of bones, joints, soft tissue, skin, and wound infections; infections in immunocompromised patients; kidney and urinary tract infections; respiratory tract infections, especially pneumonia, and ENT infections; genital infections, including gonorrhea.
Perioperative prevention of infections.
Active ingredient
Active ingredient
Composition
Composition
One vial contains:
The active ingredient
Ceftriaxone – 1.0 g, in the form of ceftriaxone sodium salt – 1.0790 g.
How to take, the dosage
How to take, the dosage
Standard dosing regimen
Intravenously, intramuscularly.
Adults and children over 12 years of age â¥50 kg: 1-2 g once daily (every 24 hours). In severe cases or in infections whose pathogens have only moderate sensitivity to ceftriaxone, the daily dose may be increased to 4 g.
The duration of treatment depends on the course of the disease. As always with antibiotic therapy, administration of ceftriaxone should be continued in patients for at least 48-72 hours after normalization of temperature and confirmation of eradication of the pathogen.
The course of treatment is usually 4-14 days; longer injections may be necessary for complicated infections.
The course of treatment for infections caused by Streptococcus pyogenes should be at least 10 days.
Injection
Only freshly prepared solutions should be used.
For intramuscular administration: 0.5 g of the drug is dissolved in 2 ml and 1 g in 3.5 ml of water for injection. The drug should be injected deeply intramuscularly into a large enough muscle (buttock). Do not inject more than 1 g into the same muscle.
For intravenous bolus administration: 0.5 g of the drug is dissolved in 5 ml and 1 g in 10 ml of water for injection. The solution is administered intravenously slowly over 5 minutes, preferably in a large vein.
For intravenous infusion: the solution is administered for at least 30 minutes.
2 g of the drug is dissolved in 40 ml of water for injection or one of the solutions which do not contain calcium (e.g. 0.9% sodium chloride solution, 5% or 10% dextrose solution, water for injection). Ceftriaxone solutions should not be mixed or added to solutions containing other antimicrobial agents or other solvents, except for those listed above, because of possible incompatibility.
Calcium-containing solvents such as Ringer’s or Hartmann’s solution should not be used to prepare ceftriaxone solutions for intravenous administration and their subsequent dilution because of the possibility of precipitate formation.
The formation of precipitates of calcium salts of ceftriaxone can also occur when Ceftriaxone and calcium-containing solutions are mixed using the same venous access. Ceftriaxone should not be used simultaneously with calcium-containing solutions for intravenous administration, including prolonged infusions of calcium-containing solutions, such as parenteral nutrition using a Ò® connector. For all groups of patients, except infants, sequential administration of ceftriaxone and calcium-containing solutions is possible with careful flushing of infusion systems between infusions with compatible fluid (see section “Interaction with other medicinal products”).
There have been no reports of interactions between ceftriaxone and oral calcium-containing drugs or interactions between ceftriaxone for intramuscular administration and calcium-containing drugs (for intravenous or oral administration).
Dosage in special cases
Patients with impaired liver function
In patients with impaired liver function there is no need to reduce the dose if there is no renal impairment.
Patients with impaired renal function
In patients with impaired renal function, there is no need to decrease the dose in the absence of hepatic impairment. The daily dose of ceftriaxone should not exceed 2 g only in cases of renal failure with creatinine clearance less than 10 ml/min. Ceftriaxone is not excreted in hemodialysis or peritoneal dialysis, therefore an additional dose of Ceftriaxone is not required after completion of dialysis.
If severe renal and hepatic impairment are combined, the efficacy and safety of the drug should be closely monitored.
Elderly and elderly patients
The usual doses for adults without adjustment for age provided there is no severe renal or hepatic impairment.
Children
Newborns, infants and children less than 12 years of age
The following dosing regimens are recommended when Ceftriaxone is prescribed once daily:
– Newborns (up to 14 days): 20-50 mg/kg body weight once daily; the daily dose should not exceed 50 mg/kg body weight;
– Newborns, infants and young children (from 15 days to 12 years): 20-80 mg/kg body weight once daily;
– Children with a body weight greater than 50 kg are prescribed adult doses.
In premature children under 41 weeks of age inclusive (cumulative gestational and chronological age) the use of ceftriaxone is contraindicated.
Ceftriaxone is contraindicated in newborns (â¤28 days) who are already receiving or anticipate intravenous treatment with calcium-containing solutions, including prolonged calcium-containing infusions such as parenteral nutrition due to the risk of precipitation of calcium salts of ceftriaxone (see “Contraindications”).
Infants and children less than 12 years of age should be given intravenous doses of 50 mg/kg or more by drip for at least 30 minutes. In newborns, intravenous doses should be given within 60 minutes to reduce the potential risk of bilirubin encephalopathy.
Meningitis
In bacterial meningitis in infants and young children, treatment begins with a dose of 100 mg/kg (but no more than 4 g) once daily. After identifying the pathogen and determining its sensitivity, the dose can be reduced accordingly. The best results with meningococcal meningitis were achieved with a treatment duration of 4 days, with meningitis caused by Haemophilus influenzae – 6 days, Streptococcus pneumoniae – 7 days.
Lyme disease
50 mg/kg (highest daily dose – 2 g) to adults and children once a day for 14 days.
Gonorrhea (caused by penicillin- and penicillin-negative strains)
A single intramuscular infusion of 250 mg of Ceftriaxone in adult patients and children over 12 years of age â¥50 kg.
Acute otitis media
In the treatment of acute otitis media in children, a single intramuscular dose of 50 mg/kg (but no more than 1 g) is recommended.
In adults, a single intramuscular dose of 1-2 g is recommended. According to limited data, in severe cases or in case of ineffectiveness of previous therapy, Ceftriaxone may be effective with intramuscular administration in a dose of 1-2 g per day for 3 days.
Prevention of postoperative infections
Depending on the degree of infection risk, 1-2 g of Ceftriaxone is administered once 30-90 minutes before surgery. In operations on the colon and rectum, simultaneous (but separate, see section “Dosage and administration”) administration of Ceftriaxone and one of the 5-nitroimidazoles, such as ornidazole, has proven well.
Interaction
Interaction
When concomitant use of high doses of ceftriaxone and “loop” diuretics (e.g., furosemide) renal dysfunction was not observed. There are conflicting data on the likelihood of increased nephrotoxicity of aminoglycosides when using them with cephalosporins, so it is necessary to monitor renal function and blood concentrations of aminoglycosides. Alcohol consumption after administration of Ceftriaxone was not accompanied by disulfiram-like reaction. Ceftriaxone does not contain N-methylthiotetrazole group, which could cause ethanol intolerance and bleeding, which is inherent in some other cephalosporins. Probenecid does not affect the excretion of Ceftriaxone.
Bacteriostatic antibiotics reduce the bactericidal effect of ceftriaxone.
In vitro antagonism between chloramphenicol and ceftriaxone has been found. Calcium-containing solvents such as Ringer’s solution or Hartmann’s solution should not be used when preparing ceftriaxone solutions for intravenous administration and subsequent dilution because of possible precipitate formation.
The formation of precipitates of calcium salts of ceftriaxone can also occur when Ceftriaxone and calcium-containing solutions are mixed using the same venous access. Ceftriaxone should not be used simultaneously with calcium-containing solutions for intravenous administration, including prolonged infusions of calcium-containing solutions, such as parenteral nutrition using a Ò® connector.
For all patient groups except infants, sequential administration of ceftriaxone and calcium-containing solutions is possible with careful flushing of infusion systems between infusions with compatible fluid. To evaluate the interaction of ceftriaxone and calcium, two in vitro studies were conducted: one using adult blood plasma and the other using neonatal cord blood plasma. Various combinations of ceftriaxone with an initial concentration of up to 1 mM (the maximum concentration that ceftriaxone reaches in vivo when 2 g of the drug is infused for at least 30 minutes) and calcium with an initial concentration of up to 12 mM (48 mg/dL) were analyzed.
Decreased plasma ceftriaxone concentrations have been observed with calcium concentrations of 6 mM (24 mg/dL) or higher for adult plasma and 4 mM (16 mg/dL) or higher for neonatal plasma, indicating an increased risk of calcium salts of ceftriaxone in neonates (see “Administration and Doses” and “Contraindications” sections).
Ceftriaxone is pharmaceutically incompatible with amsacrine, vancomycin, fluconazole and aminoglycosides.
The use of vitamin K antagonists during therapy with ceftriaxone increases the risk of bleeding. Blood clotting parameters should be constantly monitored and if necessary, the dose of anticoagulant should be adjusted both during and after therapy with ceftriaxone.
Synergism between ceftriaxone and aminoglycosides has been shown against many Gram-negative bacteria. Although the increased efficacy of such combinations is not always predictable, it should be kept in mind in severe, life-threatening infections such as those caused by Pseudomonas aeruginosa.
Special Instructions
Special Instructions
Hypersensitivity reactions
As with other β-lactam antibiotics, severe hypersensitivity reactions, including death, have been reported. In case of severe hypersensitivity reactions, therapy with Ceftriaxone should be immediately cancelled and appropriate emergency treatment measures should be taken. Before initiating therapy with Ceftriaxone it is necessary to determine whether the patient has had hypersensitivity reactions to ceftriaxone, cephalosporins or severe hypersensitivity reactions to other β-lactam antibiotics (penicillins, monobactams and carbapenems).
Caution should be exercised when using ceftriaxone in patients with a history of non-serious hypersensitivity reactions to other β-lactam antibiotics (penicillins, monobactams and carbapenems).
Sodium content
The drug ceftriaxone contains 3.6 mmol of sodium in 1 g. This should be taken into account in patients on a sodium-controlled diet.
Hemolytic anemia
As with the use of other cephalosporins, autoimmune hemolytic anemia may develop when treated with Ceftriaxone. Cases of severe hemolytic anemia in adults and children have been reported, including cases with fatal outcome.
If a patient treated with ceftriaxone develops anemia, the diagnosis of cephalosporin-associated anemia cannot be excluded and treatment must be withdrawn until the cause is determined.
Diarrhea caused by Clostridium difficile
As with most other antibacterials, cases of diarrhea caused by Clostridium difficile (C. difficile) of varying severity, from mild to fatal colitis, have been reported with Ceftriaxone treatment. Treatment with antibiotics suppresses normal colon microflora and induces the growth of C. difficile. In turn, C. difficile produces toxins A and B, which are factors in the pathogenesis of C. difficile-induced diarrhea. Toxin-producing strains of C. difficile are pathogens with a high risk of complications and mortality due to their possible resistance to antimicrobial therapy, and treatment may require colectomy.
It is important to remember the possibility of C. difficile-induced diarrhea in all patients with diarrhea after antibiotic therapy. A careful history must be taken, as there are cases of C. difficile diarrhea more than 2 months after antibiotic therapy. If diarrhea caused by C. Difficile, it may be necessary to discontinue current non-C. difficile, it may be necessary to discontinue current antibiotic therapy. Appropriate treatment with administration of fluids and electrolytes, proteins, antibiotic therapy against C. difficile, and surgical treatment should be prescribed according to clinical indications. Do not use drugs that inhibit intestinal peristalsis.
Superinfections
As with treatment with other antibacterial drugs, superinfections may develop.
Changes in prothrombin time
Rare cases of changes in prothrombin time have been described in patients treated with ceftriaxone. Patients with vitamin K insufficiency (impaired synthesis, malnutrition) may require control of prothrombin time during therapy and administration of vitamin K (10 mg/week) if prothrombin time increases before or during therapy.
The formation of ceftriaxone calcium salt precipitates
Fatal reactions have been described as a result of deposits of ceftriaxone-calcium precipitates in the lungs and kidneys of newborns. Theoretically there is a possibility of interaction of ceftriaxone with calcium-containing solutions for intravenous administration and in other age groups of patients, so ceftriaxone should not be mixed with calcium-containing solutions (including for parenteral nutrition) and also administered simultaneously, including through separate accesses for infusion at different sites. Theoretically, based on the calculation of 5 half-lives of ceftriaxone, the interval between the administration of ceftriaxone and calcium-containing solutions should be at least 48 hours.
There are no data on possible interaction of ceftriaxone with calcium-containing drugs for oral administration, as well as ceftriaxone for intramuscular administration with calcium-containing drugs (intravenous or for oral administration). After administration of ceftriaxone, usually in doses higher than the standard recommended (1 g per day or more), an ultrasound examination of the gallbladder reveals precipitates of the calcium salt of ceftriaxone, the formation of which is most likely in pediatric patients. Precipitates rarely give any symptoms and disappear after completion or discontinuation of Ceftriaxone therapy. If these phenomena are accompanied by clinical symptoms, conservative nonsurgical treatment is recommended, and the decision to discontinue the drug is left to the discretion of the treating physician and should be based on an individual benefit-risk assessment.
While there is evidence of intravascular precipitate formation only in neonates when using ceftriaxone and calcium-containing infusion solutions or any other calcium-containing drugs, Ceftriaxone should not be mixed or administered simultaneously in children and adult patients with calcium-containing infusion solutions, even using different venous accesses (see See “Contraindications” and “Interaction with other medicinal products”).
Pancreatitis
Rare cases of pancreatitis have been described in patients treated with Ceftriaxone, possibly due to biliary obstruction. Most of these patients had previous risk factors for biliary obstruction, such as previous therapy, severe illness, and complete parenteral nutrition. However, a trigger role in the development of pancreatitis cannot be excluded for precipitates formed under the influence of ceftriaxone in the biliary tract.
The use in children
The safety and efficacy of Ceftriaxone in neonates, infants and young children have been determined for the dosages described in the Administration and Dosages section. Studies have shown that, like other cephalosporins, ceftriaxone can displace bilirubin from binding to serum albumin. Ceftriaxone should not be used in newborns, especially premature infants with the risk of bilirubin encephalopathy (see section “Contraindications”).
Long-term treatment
In long-term treatment it is necessary to monitor the peripheral blood count, liver and kidney function parameters regularly.
Blood count monitoring
In long-term treatment, regular complete blood counts should be performed.
Serologic studies
False-positive results of Coombs test, galactosemia test, in determining glucose in the urine may be noted during treatment with ceftriaxone (glucosuria is recommended to be determined by enzymatic method only).
Impact on the ability to drive vehicles, machinery
There are no data on the effect of the drug on driving vehicles and working with machines and mechanisms. However, during the therapy with Ceftriaxone, caution should be exercised when driving vehicles and operating machinery due to the possibility of dizziness and other adverse reactions which may affect the ability to operate vehicles and mechanisms.
Synopsis
Synopsis
Contraindications
Contraindications
Hypersensitivity
Hypersensitivity to ceftriaxone and any other component of the drug.
Hypersensitivity to cephalosporins.
He has a history of severe hypersensitivity reactions (e.g., anaphylactic reactions) to other β-lactam antibiotics (penicillins, monobactams and carbapenems).
Perinatally born children
Perinatally born children under 41 weeks of age inclusive (cumulative gestational and chronological age) are contraindicated for the use of ceftriaxone.
Preterm infants (â¤28 days of gestational age)
– Hyperbilirubinemia, jaundice or acidosis, hypoalbuminemia in neonates (in vitro studies have shown that ceftriaxone can displace bilirubin from binding to serum albumin, increasing the risk of bilirubin encephalopathy in such patients).
Intravenous administration of calcium-containing solutions to newborns.
Newborns (â¤28 days) who are already prescribed or expected to receive intravenous treatment with calcium-containing solutions, including prolonged calcium-containing infusions such as parenteral nutrition, because of the risk of precipitate formation of calcium salts of ceftriaxone (see sections “Dosage and administration” and “Interaction with other medicinal products”).
In isolated fatal cases of precipitate formation in the lungs and kidneys in neonates receiving ceftriaxone and calcium-containing solutions have been described. In some cases a single venous access was used and precipitate formation was observed directly in the intravenous system; at least one fatal case has also been described with different venous accesses and at different times of administration of ceftriaxone and calcium-containing solutions. Such cases have been observed only in neonates (see subsection “Post-registration follow-up”).
With caution
The period of breastfeeding.
Severe hypersensitivity reactions to other β-lactam antibiotics (penicillins, monobactams and carbapenems) in history.
Side effects
Side effects
The most frequent adverse reactions reported with ceftriaxone therapy in clinical trials are eosinophilia, leukopenia, thrombocytopenia, diarrhea, rash and increased liver enzyme activity.
The following classification is used to describe the frequency of adverse reactions: very frequent (â¥1/10); frequent (â¥1/100, < 1/10); infrequent (â¥1/1000, < 1/100); rare (â¥1/10000, < 1/1000); very rare (< 1/10000) including single cases.
The adverse reactions are grouped according to the classes of medical dictionary organ systems for MedDRA regulatory activity.
Infectious and parasitic diseases: infrequent – genital mycoses; rare – pseudomembranous colitis.
Disorders of blood and lymphatic system: frequently – eosinophilia, leukopenia, thrombocytopenia; rarely – granulocytopenia, anemia, coagulopathy.
Nervous system disorders: infrequent headache and dizziness.
Respiratory system disorders, thoracic and mediastinal organs: rarely – bronchospasm.
Gastro-intestinal disorders: frequently – diarrhea, loose stools; infrequently – nausea, vomiting.
Hepatic and biliary tract disorders: often – increased activity of liver enzymes (aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP)).
Skin and subcutaneous tissue disorders: common – rash; infrequent – itching; rare – urticaria.
Renal and urinary tract disorders: rarely – hematuria, glucosuria.
General disorders and disorders at the injection site: infrequent – phlebitis, pain at the injection site, fever; rarely – edema, chills.
Impact on the results of laboratory and instrumental studies: infrequent – increase in blood creatinine concentration.
Post-registration follow-up
The side effects observed with ceftriaxone during the post-registration period are described below. It is not always possible to determine the frequencies of adverse events observed and their relationship to ceftriaxone use because the exact size of the patient population cannot be determined.
Gastrointestinal disorders: pancreatitis, stomatitis, glossitis, taste disorders.
Blood and lymphatic system disorders: thrombocytosis, increased thromboplastin and prothrombin time, decreased prothrombin time, hemolytic anemia. Individual cases of agranulocytosis (< 500 cells/μl) have been described, with most developing after 10 days of treatment and using a cumulative dose of 20 g or more.
Immune system disorders: anaphylactic shock, hypersensitivity.
Skin and subcutaneous tissue disorders: acute generalized exanthematous pustulosis, individual cases of severe adverse reactions (erythema multiforme exudative, Stevens-Johnson syndrome, toxic epidermal necrolysis (Lyell’s syndrome)).
Nervous system disorders: seizures.
Hearing and labyrinth disorders: vertigo.
Infectious and parasitic diseases: superinfections.
The following adverse reactions are also known: The formation of precipitates of calcium salts of ceftriaxone in the gallbladder with associated symptoms, bilirubin encephalopathy, hyperbilirubinemia, oliguria, vaginitis, increased sweating, “flushes,” allergic pneumonitis, nasal bleeding, jaundice, palpitations, serum sickness, and anaphylactic or anaphylactoid reactions.
He has described isolated fatal cases of precipitate formation in the lungs and kidneys from autopsy studies in neonates receiving Ceftriaxone and calcium-containing solutions. In some cases, a single venous access was used, and precipitate formation was observed directly in the intravenous system. At least one case with a fatal outcome was also described with different venous accesses and at different times of administration of Ceftriaxone and calcium-containing solutions. However, autopsy results showed no precipitates in this neonate. Similar cases have been observed only in newborns (see section “Special indications”).
The formation of ceftriaxone precipitates in the urinary tract has been reported mainly in children who received either high daily doses of the drug (â¥80 mg/kg per day) or cumulative doses greater than 10 g, and who had additional risk factors (dehydration, bed rest). The formation of precipitates in the kidneys may be asymptomatic or manifest clinically and may lead to ureteral obstruction and postrenal acute renal failure. This adverse event is reversible and resolves after discontinuation of Ceftriaxone therapy.
General disorders and disorders at the injection site: phlebitis after intravenous injection. It can be avoided by injecting the drug slowly for 5 minutes, preferably into a large vein.
Impact on laboratory test results
False positive Coombs test results may be observed in patients treated with Ceftriaxone. As with other antibiotics, ceftriaxone may give false-positive results for galactosemia. False-positive results may also be obtained when determining glucose in the urine by non-enzymatic methods, so during therapy with Ceftriaxone glucosuria should be determined by enzymatic method only, if necessary.
Ceftriaxone may cause unreliable decrease in glycemic values obtained with some blood glucose monitoring devices (see the instructions for use of the device used). If necessary, alternative methods of blood glucose determination should be used.
Overdose
Overdose
Symptoms: Nausea, vomiting and diarrhea.
Treatment: In case of overdose hemodialysis and peritoneal dialysis will not reduce drug concentrations. There is no specific antidote. Treatment of overdose is symptomatic.
Pregnancy use
Pregnancy use
Pregnancy
Ceftriaxone penetrates the placental barrier. The safety of use in pregnancy in women has not been established. Preclinical reproductive studies have shown no embryotoxic, fetotoxic, teratogenic effects or other adverse effects of the drug on fecundity of males and females, the process of childbirth, perinatal and postnatal development of the fetus. In pregnancy, especially in the first trimester, should be administered only under strict indications, provided that the expected benefits to the mother exceed the potential risk to the fetus.
Breastfeeding period
In low concentrations ceftriaxone passes into breast milk. The effect of ceftriaxone on the breastfed baby is unlikely when used by the mother in therapeutic doses; however, the risk of diarrhea, fungal mucous membrane infections and hypersensitivity reactions in the baby cannot be excluded. Breastfeeding should be discontinued or cease/abstain from ceftriaxone therapy, taking into account the benefits of breastfeeding for the baby and the benefits of therapy for the mother.
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In a light-protected place at a temperature not exceeding 25 °C. Keep out of reach of children. |
| Manufacturer | Borisov Medical Preparations Plant, Belarus |
| Medication form | Powder for preparation of solution |
| Brand | Borisov Medical Preparations Plant |
Other forms…
Related products
Buy Ceftriaxone, 1 g with delivery to USA, UK, Europe and over 120 other countries.