No products in the cart.
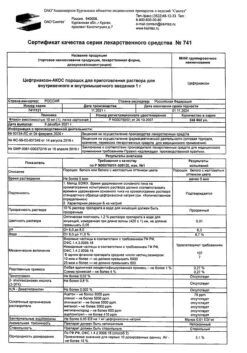
Ceftriaxone
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group:
Antibiotic – cephalosporin
ATX code:
J01DD04
Pharmacological properties
Pharmacodynamics.
Ceftriaxone is a parenteral cephalosporin antibiotic of III generation. Bactericidal activity of ceftriaxone is due to inhibition of cell wall synthesis. In vitro ceftriaxone has a broad spectrum against Gram-negative and Gram-positive microorganisms. It is highly resistant to most β – lactamases (both penicillinases and cephalosporinases) produced by Gram-positive and Gram-negative bacteria.
Ceftriaxone is generally active against the following microorganisms:
Gram-positive aerobes
Staphylococcus aureus (methicillin-sensitive), coagulase-negative staphylococci, Streptococcus pyogenes (β-hemolytic, group A), Streptococcus agalactiae (p-hemolytic, group B), p-hemolytic streptococci (groups neither A nor B), Streptococcus viridans, Streptococcus pneumoniae.
Note. Methicillin-resistant Staphylococcus spp. are resistant to cephalosporins, including ceftriaxone. Enterococcus faecalis, Enterococcus faecium and Listeria monocytogenes are also generally resistant.
Gram-negative aerobes
Acinetobacter lwoffii, Acinetobacter anitratus (mainly A. baumanni)*, Aeromonas hydrophila, Alcaligenes faecalis, Alcaligenes odorans, alkaligenes-like bacteria, Borrelia burgdorferi, Capnocytophaga spp, Citrobacter diversus (including C. amalonaticus), Citrobacter freundii*, Escherichia coli, Enterobacter aerogenes*, Enterobacter cloacae*, Enterobacter spp. (others)*, Haemophilus ducreyi, Haemophilus influenzae, Haemophilus parainfluenzae, Hafnia alvei, Klebsiella oxytoca, Klebsiella pneumonia**, Moraxella catarrhalis (previously called Branhamella catarrhalis), Moraxella osloensis, Moraxella spp. (others), Morganella morganii, Neisseria gonorrhoeae, Neisseria meningitidis, Pasteurella multocida, Plesiomonas shigelloides, Proteus mirabilis, Proteus penneri*, Proteus vulgaris*, Pseudomonas fluorescens*, Pseudomonas spp. (other), Providencia rettgeri*, Providencia spp. (other), Salmonella typhi, Salmonella spp. (nontyphoid), Serratia marcescens*, Serratia spp. (other)*, Shigella spp, Vibrio spp., Yersinia enterocolitica, Yersinia spp. (other).
*Some isolates of these species are resistant to ceftriaxone, mainly due to the formation of chromosome-encoded p-lactamases.
**Some isolates of these species are resistant due to the formation of a variety of plasmid-mediated p-lactamases.
Note. Many strains of the above microorganisms that are multiresistant to other antibiotics, such as aminopenicillins and ureidopenicillins, first and second generation cephalosporins and aminoglycosides, are sensitive to ceftriaxone. Treponema pallidum is sensitive to ceftriaxone in vitro and in animal experiments. Clinical trials show that ceftriaxone has good efficacy against primary and secondary syphilis. With very few exceptions, clinical isolates of P. aeruginosa are resistant to ceftriaxone.
The anaerobes
Bacteroides spp. (bile-sensitive)*, Clostridium spp. (except C. difficile), Fusobacterium nucleatum, Fusobacterium spp. (other), Gaffkya anaerobica (previously called Peptococcus), Peptostreptococcus.
*Some isolates of these species are resistant to ceftriaxone due to the formation of P-lactamases. Note. Many strains of p-lactamase-producing Bacteroides spp. (particularly B. fragilis) are resistant. Clostridium difficile is also resistant.
Sensitivity to ceftriaxone can be determined by disk-diffusion or serial dilutions on agar or broth, using a standard technique similar to that recommended by the Institute of Clinical and Laboratory Standards (ICLS). The ICLS has established the following criteria for evaluating assay results for ceftriaxone:


Pharmacokinetics
Pharmacokinetics of ceftriaxone is non-linear. All major pharmacokinetic parameters based on total drug concentrations, with the exception of the elimination half-life, are dose-dependent and increase in less than proportional proportion to its increase. Nonlinearity is typical for pharmacokinetic parameters that depend on the total concentration of ceftriaxone in blood plasma (not only free ceftriaxone), and is explained by saturation of the drug binding to blood plasma proteins.
Intake
Maximum plasma concentration after a single intramuscular injection of 1 g of the drug is about 81 mg/l and is reached within 2-3 hours after administration. Areas under the curve “plasma concentration – time” after intravenous and intramuscular administration are the same. This means that bioavailability of ceftriaxone after intramuscular administration is 100%.
After intravenous bolus administration of 500 mg and 1 g of ceftriaxone average maximum plasma concentrations were 120 mg/l and 200 mg/l, respectively. After intravenous infusion of 500 mg, 1 g, and 2 g of ceftriaxone, plasma concentrations of the drug were approximately 80, 150, and 250 mg/L, respectively. After intramuscular injection, mean maximum plasma ceftriaxone concentrations were approximately half as high as after intravenous administration of an equivalent dose of the drug.
Distribution
The volume of distribution of ceftriaxone is 7 – 12 liters. After administration in a dose of 1 – 2 g ceftriaxone penetrates well into tissues and body fluids. For more than 24 hours its concentrations far exceed the minimum suppressive concentrations for most infectious agents in more than 60 tissues and fluids (including lungs, heart, biliary tract, liver, tonsils, middle ear and nasal mucosa, bones, as well as cerebrospinal, pleural and synovial fluids and prostate secretion).
After intravenous administration ceftriaxone rapidly penetrates into the cerebrospinal fluid, where bactericidal concentrations against susceptible microorganisms persist for 24 hours.
Protein binding
Ceftriaxone reversibly binds to albumin. The degree of binding is approximately 95% when values of ceftriaxone concentration in blood plasma are less than 100 mg/l. The proportion of ceftriaxone bound to plasma protein decreases with increasing concentration, as the binding is saturable and is about 85% at values of 300 mg/l.
Permeasurement in selected tissues
Ceftriaxone penetrates through the cerebral membranes, the greatest extent in their inflammation. The average maximum concentration of ceftriaxone in the cerebrospinal fluid reaches 25% of the plasma ceftriaxone concentration in patients with bacterial meningitis, and only 2% of the plasma concentration in patients with non-inflamed cerebral membranes. Maximum concentration of ceftriaxone in the cerebrospinal fluid is reached 4-6 hours after its intravenous administration.
Ceftriaxone passes through the placental barrier and in low concentrations passes into breast milk.
Metabolism
Ceftriaxone does not undergo systemic metabolism but is converted into inactive metabolites by the intestinal microflora.
Elimation
Total plasma clearance of ceftriaxone is 10-22 ml/min. Renal clearance is 5-12 ml/min. 50-60% of ceftriaxone is excreted unchanged by the kidneys, and 40-50% – unchanged by the intestine. The half-life of ceftriaxone in adults is about 8 hours.
Pharmacokinetics in special clinical cases
Newborns, infants and children younger than 12 years
In newborn children the half-life of ceftriaxone is longer compared to other age groups. During the first 14 days of life, the plasma concentration of free ceftriaxone may be further increased due to low glomerular filtration and peculiarities of the drug binding to blood plasma proteins. In pediatric patients the half-life is shorter than in newborns and adults.
The values of plasma clearance and volume of distribution of total ceftriaxone are higher in neonates, infants and children younger than 12 years compared to those in adults.
Hepatic or renal impairment
In patients with impaired renal or hepatic function the pharmacokinetics of ceftriaxone changes slightly, only a slight increase in the elimination half-life (less than 2-fold) is noted even in patients with severe renal impairment.
The slight increase in the half-life of ceftriaxone in renal failure may be explained by a compensatory increase in nonrenal clearance as a result of decreased binding to plasma proteins and a corresponding increase in nonrenal clearance of total ceftriaxone.
In patients with hepatic insufficiency, the half-life is not increased. In these patients there is a compensatory increase in renal clearance. This is also due to an increase in the plasma concentration of free ceftriaxone, which contributes to a paradoxical increase in total drug clearance against an increase in the volume of distribution.
Patients of advanced age
Patients over 75 years of age have, on average, a half-life two or three times longer than that of adult patients.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
Standard dosing regimen
Intravenously, infusion.
Adults and children over 12 years of age ⥠50 kg: 1 to 2 g once daily (every 24 hours). In severe cases or in infections whose pathogens are only moderately sensitive to ceftriaxone, the daily dose may be increased to 4 g.
The duration of treatment depends on the course of the disease. As always with antibiotic therapy, administration of ceftriaxone should be continued for at least 48 to 72 hours after normalization of temperature and confirmation of eradication of the pathogen. Usually the course of treatment is 4-14 days; for complicated infections a longer course may be needed.
The course of treatment of infections caused by Streptococcus pyogenes should be at least 10 days.
Injection
The general rule should be to use solutions immediately after preparation.
The intravenous infusion should last at least 30 minutes. For solution preparation 2 g of ceftriaxone is diluted in 40 ml of one of the following infusion solutions, not containing calcium ions: 0.9% sodium chloride solution, 0.45% sodium chloride solution + 2.5% dextrose solution, 5% dextrose solution, 10% dextrose solution, 6% dextran solution in 5% dextrose solution, 6 – 10% hydroxyethyl starch solution, water for injection. Ceftriaxone solutions must not be mixed or added to solutions containing other antimicrobial agents or other solvents, except for those listed above, due to possible incompatibility.
Calcium-containing solvents such as Ringer’s solution or Hartmann’s solution should not be used to prepare ceftriaxone solutions for intravenous administration and their subsequent dilution because of possible precipitate formation.
The formation of precipitates of calcium salts of ceftriaxone can also occur when ceftriaxone and calcium-containing solutions are mixed using the same venous access. Ceftriaxone should not be used simultaneously with calcium-containing solutions for intravenous administration, including prolonged infusions of calcium-containing solutions, for example, during parenteral nutrition using a Y-connector. For all groups of patients, except infants, sequential administration of ceftriaxone and calcium-containing solutions is possible with careful flushing of the infusion systems between infusions with compatible fluid (see section “Interaction with other medicinal products”).
There have been no reports of interactions between ceftriaxone and oral calcium-containing drugs or interactions between ceftriaxone for intramuscular administration and calcium-containing solutions (for intravenous or oral administration).
Dosage in special cases
Patients with impaired liver function
In patients with impaired liver function there is no need to reduce the dose if there is no renal impairment.
Patients with impaired renal function
In patients with impaired renal function, there is no need to decrease the dose in the absence of hepatic impairment. The daily dose of ceftriaxone should not exceed 2 g only in cases of renal failure with creatinine clearance less than 10 ml/min. Ceftriaxone is not excreted in hemodialysis or peritoneal dialysis, so no additional dose of ceftriaxone is required after dialysis.
If severe renal and hepatic impairment are combined, the efficacy and safety of the drug should be closely monitored.
Elderly and elderly patients
Normal doses for adults without adjustment for age provided there is no severe renal or hepatic impairment.
Children
Newborns, infants and children younger than 12 years
The following dosing regimens are recommended when administering ceftriaxone once daily:
Preterm infants under 41 weeks of age inclusive (total gestational and chronological age) are contraindicated for use of ceftriaxone.
Ceftriaxone is contraindicated in newborns (⤠28 days) who are already receiving or anticipate intravenous treatment with calcium-containing solutions, including prolonged calcium-containing infusions such as parenteral nutrition due to the risk of precipitation of calcium salts of ceftriaxone (see section “Contraindications”).
Infants and children less than 12 years of age should be given intravenous doses of 50 mg/kg or more by drip for at least 30 minutes. Newborns should be given intravenously for 60 minutes to reduce the potential risk of bilirubin encephalopathy.
Meningitis
In bacterial meningitis in infants and young children, treatment begins with a dose of 100 mg/kg (but no more than 4 g) once daily. After identifying the pathogen and determining its sensitivity, the dose can be reduced accordingly. The best results with meningococcal meningitis were achieved with a treatment duration of 4 days, with meningitis caused by Haemophilus influenzae – 6 days, Streptococcus pneumoniae – 7 days.
Lyme disease
50 mg/kg (highest daily dose – 2 g) to adults and children once a day for 14 days.
Prevention of postoperative infections
Depending on the degree of infection risk 1 – 2 g ceftriaxone is administered once 30 to 90 minutes before surgery. In operations on the colon and rectum, simultaneous (but separate, see section “Dosage and administration”) administration of ceftriaxone and one of the 5-nitroimidazoles, such as ornidazole, has proven well.
Interaction
Interaction
When concomitant use of high doses of ceftriaxone and “loop” diuretics (e.g., furosemide) renal dysfunction was not observed. There are conflicting data on the likelihood of increased nephrotoxicity of aminoglycosides when using them with cephalosporins, so it is necessary to monitor renal function and blood concentrations of aminoglycosides. Alcohol consumption after administration of ceftriaxone was not accompanied by disulfiram-like reaction. Ceftriaxone does not contain N-methylthiotetrazole group, which could cause ethanol intolerance and bleeding, which is inherent in some other cephalosporins.
Probenecid does not affect the excretion of ceftriaxone.
Bacteriostatic antibiotics reduce the bactericidal effect of ceftriaxone.
In vitro antagonism has been found between chloramphenicol and ceftriaxone.
Calcium-containing solvents such as Ringer’s solution or Hartmann’s solution should not be used when preparing ceftriaxone solutions for intravenous administration and subsequent dilution because of the possibility of precipitate formation.
The formation of precipitates of calcium salts of ceftriaxone can also occur when ceftriaxone and calcium-containing solutions are mixed using the same venous access. Ceftriaxone should not be used simultaneously with calcium-containing solutions for intravenous administration, including prolonged infusions of calcium-containing solutions, such as parenteral nutrition using a Y-connector. For all patient groups except neonates, sequential administration of ceftriaxone and calcium-containing solutions is possible with careful flushing of the infusion systems between infusions with compatible fluid. To evaluate the interaction of ceftriaxone and calcium, two in vitro studies were conducted: one using adult blood plasma and the other using neonatal cord blood plasma. Various combinations of ceftriaxone with an initial concentration of up to 1 mM (the maximum concentration that ceftriaxone reaches in vivo when infused with 2 g of the drug for at least 30 min) and calcium with an initial concentration of up to 12 mM (48 mg/dL) were analyzed. A decrease in plasma ceftriaxone concentration was observed when calcium was used at a concentration of 6 mM (24 mg/dL) or higher for adult plasma and at a concentration of 4 mM (16 mg/dL) or higher for neonatal plasma, indicating an increased risk of calcium salts of ceftriaxone in neonates (see “Administration and Doses” and “Contraindications” sections).
Ceftriaxone is pharmaceutically incompatible with amsacrine, vancomycin, fluconazole and aminoglycosides.
The use of vitamin K antagonists during ceftriaxone therapy increases the risk of bleeding. Blood clotting parameters should be constantly monitored and, if necessary, the anticoagulant dose should be adjusted both during and after ceftriaxone therapy.
Synergism between ceftriaxone and aminoglycosides against many Gram-negative bacteria has been shown. Although the increased efficacy of such combinations is not always predictable, it should be kept in mind in severe, life-threatening infections such as those caused by Pseudomonas aeruginosa.
Special Instructions
Special Instructions
Hypersensitivity reactions
As with other β-lactam antibiotics, severe hypersensitivity reactions, including death, have been reported. In case of severe hypersensitivity reactions, ceftriaxone therapy should be immediately withdrawn and appropriate emergency treatment measures should be taken. Before starting therapy with ceftriaxone it is necessary to establish whether the patient has had hypersensitivity reactions to ceftriaxone, cephalosporins or severe hypersensitivity reactions to other β-lactam antibiotics (penicillins, monobactams and carbapenems).
Caution should be exercised when using ceftriaxone in patients with a history of non-serious hypersensitivity reactions to other P-lactam antibiotics (penicillins, monobactams and carbapenems).
The sodium content
1 g of ceftriaxone contains 3.6 mmol of sodium. This should be taken into account in patients on a sodium-controlled diet.
Hemolytic anemia
As with other cephalosporins, autoimmune hemolytic anemia may develop during treatment with ceftriaxone. Cases of severe hemolytic anemia in adults and children, including fatalities, have been reported.
If a patient treated with ceftriaxone develops anemia, the diagnosis of cephalosporin-associated anemia cannot be excluded and treatment should be withdrawn until the cause is determined.
Diarrhea caused by Clostridium difficile
As with most other antibacterials, cases of diarrhea caused by Clostridium difficile (C. difficile) of varying severity, from mild diarrhea to fatal colitis, have been reported with ceftriaxone treatment. Treatment with antibiotics suppresses normal colon microflora and induces the growth of C. difficile. In turn, C. difficile produces toxins A and B, which are factors in the pathogenesis of diarrhea caused by C. difficile. Toxin-producing strains of C. difficile cause infections with a high risk of complications and mortality due to their possible resistance to antimicrobial therapy, and treatment may require colectomy. The possibility of C. difficile-induced diarrhea in all patients with diarrhea after antibiotic therapy must be kept in mind. A careful history must be taken, as there are cases of C. difficile diarrhea more than 2 months after antibiotic therapy. If diarrhea caused by C. difficile is suspected or confirmed, current non-C. difficile antibiotic therapy may need to be withdrawn. Appropriate treatment with administration of fluids and electrolytes, proteins, antibiotic therapy against C. difficile, and surgical treatment should be prescribed according to clinical indications. Do not use drugs that inhibit intestinal peristalsis.
Superinfections
As with treatment with other antibacterial drugs, superinfections may develop.
Prothrombin time changes
Rare cases of changes in prothrombin time have been described in patients receiving ceftriaxone. Patients with vitamin K insufficiency (synthesis disorders, nutritional disorders) may require control of prothrombin time during therapy and administration of vitamin K (10 mg/week) if prothrombin time increases before or during therapy.
The formation of calcium salt precipitates of ceftriaxone
Cases of fatal reactions have been described due to deposition of ceftriaxone-calcium precipitates in the lungs and kidneys of newborns. Theoretically there is a possibility of interaction of ceftriaxone with calcium-containing solutions for intravenous administration and in other age groups of patients, so ceftriaxone should not be mixed with calcium-containing solutions (including for parenteral nutrition), and also administered simultaneously, including through separate accesses for infusion at different sites. Theoretically, based on the calculation of 5 half-lives of ceftriaxone, the interval between the administration of ceftriaxone and calcium-containing solutions should be at least 48 hours. There are no data on possible interaction of ceftriaxone with calcium-containing drugs for oral administration, as well as ceftriaxone for intramuscular administration with calcium-containing drugs (intravenously or for oral administration). After administration of ceftriaxone, usually in doses higher than the standard recommended (1 g per day or more), an ultrasound examination of the gallbladder has revealed precipitates of the calcium salt of ceftriaxone, the formation of which is most likely in pediatric patients. The precipitates rarely produce any symptoms and disappear after completion or discontinuation of ceftriaxone therapy. If these phenomena are accompanied by clinical symptoms, conservative nonsurgical treatment is recommended, and the decision to withdraw the drug is left to the discretion of the treating physician and should be based on an individual benefit-risk assessment.
While there is evidence of intravascular precipitate formation only in neonates when using ceftriaxone and calcium-containing infusion solutions or any other calcium-containing drugs, ceftriaxone should not be mixed or administered simultaneously to children and adult patients with calcium-containing infusion solutions, even using different venous accesses (see See “Contraindications” and “Interaction with other medicinal products”, subsection “Post-registration monitoring”).
Pancreatitis
Rare cases of pancreatitis have been described in patients treated with ceftriaxone, possibly due to biliary obstruction. Most of these patients had previous risk factors for biliary obstruction, such as previous therapy, severe illness and complete parenteral nutrition. At the same time, a trigger role in the development of pancreatitis cannot be excluded for precipitates in the biliary tract formed under the influence of ceftriaxone.
Pediatric use
The safety and efficacy of ceftriaxone in neonates, infants and young children have been determined for the dosages described in the “Dosage and administration” section. Studies have shown that, like other cephalosporins, ceftriaxone can displace bilirubin from serum albumin binding.
Ceftriaxone should not be used in newborns, especially premature infants, who have a risk of bilirubin encephalopathy (see section “Contraindications”).
Long-term treatment
In long-term treatment it is necessary to monitor the peripheral blood count, liver and kidney function tests regularly.
Blood test monitoring
In long-term treatment, regular complete blood counts should be performed.
Serologic studies
False-positive results of Coombs test, galactosemia test, in determining glucose in urine may be observed during treatment with ceftriaxone (glucosuria is recommended to be determined by enzymatic method only).
There are no data indicating the effect of the drug on driving vehicles and working with machines and mechanisms. However, during therapy with ceftriaxone, caution should be exercised when driving vehicles and operating machinery due to the possibility of dizziness and other adverse reactions that may affect the ability to drive vehicles, mechanisms.
Contraindications
Contraindications
Hypersensitivity
Hypersensitivity to ceftriaxone and any other component of the drug. Hypersensitivity to cephalosporins.
Severe hypersensitivity reactions (e.g., anaphylactic reactions) to other β-lactam antibiotics (penicillins, monobactams and carbapenems) in the history.
Perinatally born children
Premature infants under 41 weeks of age inclusive (total gestational and chronological age) are contraindicated for the use of ceftriaxone.
Preterm infants (⤠28 days of age)
Breastfeeding period.
No history of hypersensitivity reactions to other β-lactam antibiotics (penicillins, monobactams and carbapenems).
Side effects
Side effects
The most frequent adverse reactions reported with ceftriaxone therapy in clinical trials are eosinophilia, leukopenia, thrombocytopenia, diarrhea, rash and increased hepatic enzyme activity.
The following classification is used to describe the frequency of adverse reactions: very frequent (â¥1/10), frequent (â¥1/100 and < 1/10), infrequent (â¥1/1000 and < 1/100), rare (â¥1/10000 and < 1/1000) and very rare (< 1/10000), including isolated cases.
The adverse reactions are grouped according to the classes of medical dictionary organ systems for MedDRA regulatory activity.
Infectious and parasitic diseases: infrequent – genital mycoses; rarely – pseudomembranous colitis.
Disorders of blood and lymphatic system: frequently – eosinophilia, leukopenia, thrombocytopenia; rarely – granulocytopenia, anemia, coagulopathy.
Nervous system disorders: infrequent – headache and dizziness.
Respiratory system disorders, thoracic and mediastinal organs: rarely – bronchospasm.
Gastro-intestinal disorders: frequently – diarrhea, loose stools; infrequently – nausea, vomiting.
Hepatic and biliary tract disorders: often – increased activity of liver enzymes (aspartate aminotransferase (ACT), alanine aminotransferase (ALT), alkaline phosphatase (ALP)).
Skin and subcutaneous tissue disorders: common – rash; infrequent – itching; rare – urticaria.
Renal and urinary tract disorders: rarely – hematuria, glucosuria.
General disorders and disorders at the injection site: infrequent – phlebitis, pain at the injection site, increased body temperature; rarely – swelling, chills.
Impact on the results of laboratory and instrumental studies: infrequent – increase in blood creatinine concentration.
The side effects observed with ceftriaxone during the post-registration period are described below. It is not always possible to determine the frequencies of adverse events observed and their relationship to ceftriaxone use because the exact size of the patient population cannot be determined.
Gastrointestinal disorders: pancreatitis, stomatitis, glossitis, taste disorders.
Blood and lymphatic system disorders: thrombocytosis, increased thromboplastin and prothrombin time, decreased prothrombin time, hemolytic anemia. Individual cases of agranulocytosis (< 500 cells/μl) have been described, with most developing after 10 days of treatment and using a cumulative dose of 20 g or more.
Immune system disorders: anaphylactic shock, hypersensitivity.
Skin and subcutaneous tissue disorders: acute generalized exanthematous pustulosis, individual cases of severe adverse reactions (erythema multiforme exudative, Stevens-Johnson syndrome, toxic epidermal necrolysis (Lyell’s syndrome)).
Nervous system disorders: seizures.
Hearing and labyrinth disorders: vertigo.
Infectious and parasitic diseases: superinfections.
The following adverse reactions are also known: The formation of precipitates of calcium salts of ceftriaxone in the gallbladder with associated symptoms, bilirubin encephalopathy, hyperbilirubinemia, oliguria, vaginitis, increased sweating, “flushes,” allergic pneumonitis, nasal bleeding, jaundice, palpitations, serum sickness, and anaphylactic or anaphylactoid reactions.
He has described isolated fatal cases of precipitate formation in the lungs and kidneys from autopsy studies in newborns who received ceftriaxone and calcium-containing solutions. In some cases, a single venous access was used, and precipitate formation was observed directly in the intravenous system. At least one case with a fatal outcome was also described with different venous accesses and at different times of administration of ceftriaxone and calcium-containing solutions. However, on autopsy no precipitates were found in this newborn. Similar cases have been observed only in newborns (see section “Special indications”).
The formation of ceftriaxone precipitates in the urinary tract has been reported mainly in children who received either high daily doses of the drug (⥠80 mg/kg per day) or cumulative doses of more than 10 g, and who had additional risk factors (dehydration, bed rest). The formation of precipitates in the kidneys may be asymptomatic or manifest clinically and may lead to ureteral obstruction and postrenal acute renal failure. This adverse event is reversible and resolves after discontinuation of ceftriaxone therapy.
General disorders and disorders at the injection site: phlebitis after intravenous administration. It can be avoided by injecting the drug slowly for 5 minutes, preferably in a large vein.
Impact on laboratory test results
False positive Coombs test results may be observed in patients treated with ceftriaxone. Like other antibiotics, ceftriaxone may give false-positive results for galactosemia. False-positive results may also be obtained when determining glucose in the urine by non-enzymatic methods, so during therapy with ceftriaxone glucosuria should be determined by enzymatic method only, if necessary.
Ceftriaxone may cause unreliable decrease in glycemic values obtained with some blood glucose monitoring devices. See the instructions for use of the device used. If necessary, alternative methods of blood glucose determination should be used.
Overdose
Overdose
Pregnancy use
Pregnancy use
Additional information
| Shelf life | 2 years. Do not use after the expiration date |
|---|---|
| Conditions of storage | In a light-protected place at a temperature not exceeding 25 °C. Keep out of reach of children. |
| Manufacturer | PharmConcept, Russia |
| Medication form | solution for injection |
| Brand | PharmConcept |
Other forms…
Related products
Buy Ceftriaxone with delivery to USA, UK, Europe and over 120 other countries.