No products in the cart.
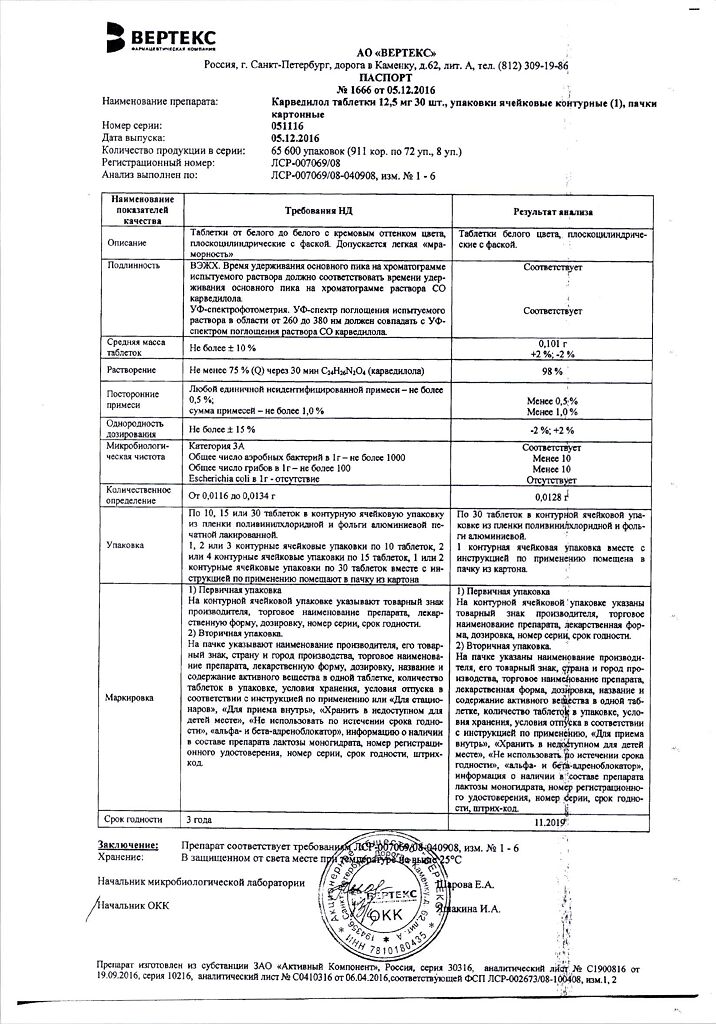
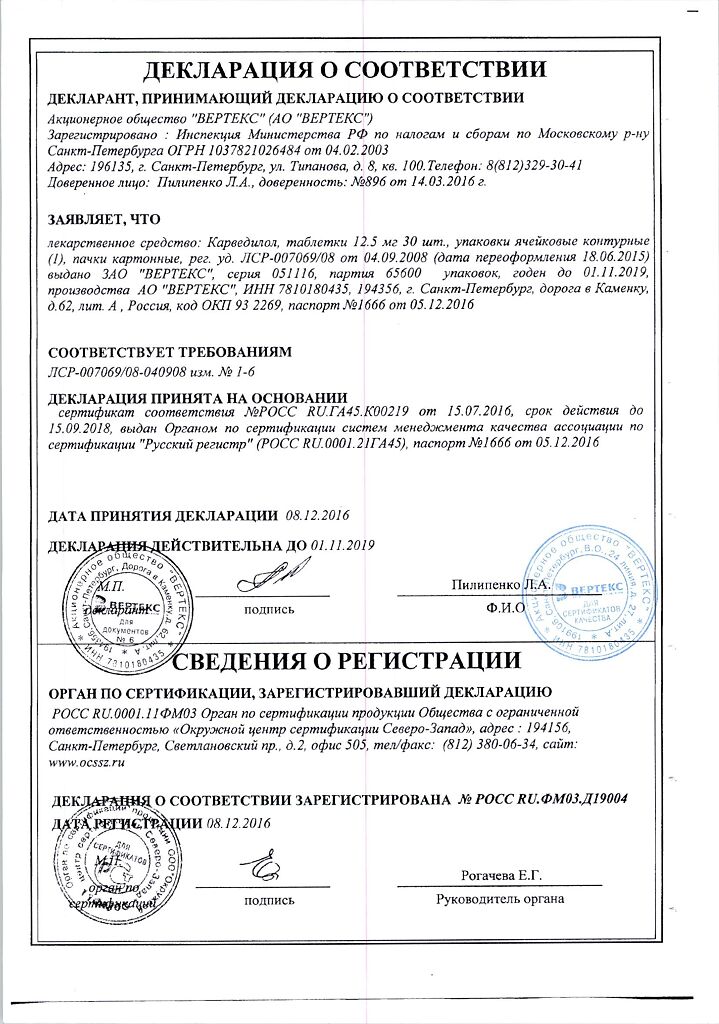
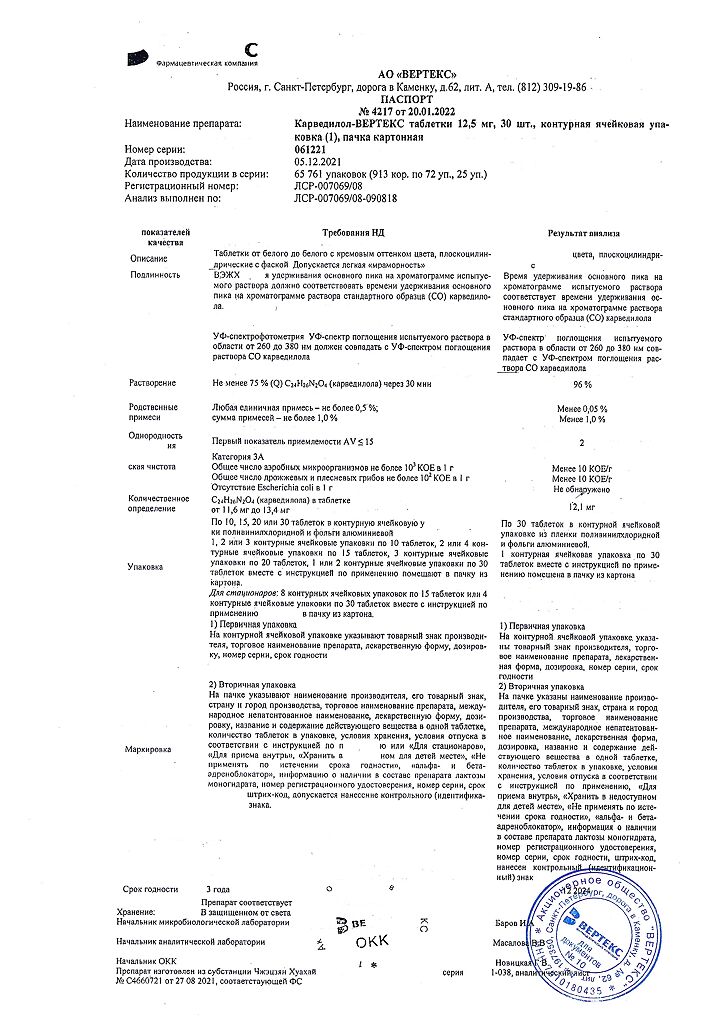
Carvedilol-Vertex, tablets 12.5mg 30 pcs
€7.71 €6.43
Description
- Arterial hypertension (in monotherapy and in combination with diuretics)
- Cronic heart failure (in combination therapy)
- Ischemic heart disease: stable angina.
.
Indications
Indications
Arterial hypertension (in monotherapy and combination with diuretics)
Chronic heart failure (as part of combination therapy)
Coronary heart disease: stable angina.
Pharmacological effect
Pharmacological effect
Alpha and beta blocker
Special instructions
Special instructions
Therapy should be carried out over a long period of time and should not be stopped abruptly, especially in patients with coronary heart disease, as this can lead to a worsening of the underlying disease. If necessary, the dose reduction should be gradual over 1-2 weeks.
At the beginning of therapy with carvedilol or when the dose of the drug is increased in patients, especially elderly patients, an excessive decrease in blood pressure may be observed, mainly when standing up. A dose adjustment of the drug is necessary. In patients with chronic heart failure, when selecting a dose, an increase in symptoms of heart failure and the appearance of edema is possible. In this case, the dose of carvedilol should not be increased; it is recommended to prescribe large doses of diuretics until the patient’s condition is stabilized.
Continuous monitoring of the electrocardiogram and blood pressure is recommended while prescribing carvedilol and slow calcium channel blockers, phenylalkylamine derivatives (verapamil) and benzodiazepine (diltiazem), as well as with class I antiarrhythmic drugs.
It is recommended to monitor renal function in patients with chronic renal failure, arterial hypotension and chronic heart failure.
In case of surgery using general anesthesia, the anesthesiologist should be warned about previous therapy with carvedilol.
Carvedilol does not affect the concentration of glucose in the blood and does not cause changes in the glucose tolerance test in patients with non-insulin-dependent diabetes mellitus.
Avoid drinking ethanol during treatment.
Patients with pheochromocytoma should be prescribed alpha-blockers before starting therapy.
Patients wearing contact lenses should be aware that the drug may cause a decrease in tear production.
It is not recommended to drive a car at the beginning of therapy and when increasing the dose of carvedilol. You should refrain from other activities that require high concentration of attention and rapid psychomotor reactions.
Active ingredient
Active ingredient
Carvedilol
Composition
Composition
1 tablet contains:
active ingredient:
carvedilol 12.5 mg
Contraindications
Contraindications
Hypersensitivity to carvedilol or other components of the drug,
acute and decompensated chronic heart failure,
requiring intravenous administration of inotropic agents,
severe liver failure,
atrioventricular block stage II-III,
severe bradycardia (less than 50 beats/min),
sick sinus syndrome,
arterial hypotension (systolic blood pressure less than 85 mm Hg),
cardiogenic shock,
bronchial asthma,
chronic obstructive pulmonary disease,
age under 18 years (efficacy and safety have not been established).
With caution
Bronchospastic syndrome, chronic bronchitis, pulmonary emphysema, Prinzmetal angina, thyrotoxicosis, occlusive diseases of peripheral vessels, pheochromocytoma, psoriasis, renal failure, first degree atrioventricular block, extensive surgical interventions and general anesthesia, diabetes mellitus, hypoglycemia, depression, myasthenia gravis.
Side Effects
Side Effects
From the immune system: very rare – hypersensitivity.
From the hematopoietic system: frequent – anemia; rare – thrombocytopenia; very rare – leukopenia.
From the nervous system: very common – dizziness, headache; Uncommon – presyncope, fainting, paresthesia.
On the part of the organ of vision: frequent – visual disturbances, decreased tear production (dry eyes), eye irritation.
From the cardiovascular system: very common – heart failure during the period of increasing dose, marked decrease in blood pressure; common – bradycardia, edema, hypervolemia, fluid retention, orthostatic hypotension, peripheral circulatory disorders (cold extremities, peripheral vascular disease, exacerbation of intermittent claudication and Raynaud’s syndrome); uncommon – AV block II-III degree, angina pectoris.
From the respiratory system: frequent – shortness of breath, pulmonary edema, asthma in predisposed patients, bronchitis, pneumonia, upper respiratory tract infections; rare – nasal congestion.
From the digestive system: frequent – nausea, diarrhea, vomiting, dyspepsia, abdominal pain; Uncommon: constipation, dry mouth.
From the liver and biliary tract: very rare – increased activity of ALT, AST and GGT.
From the skin and subcutaneous tissues: uncommon – skin reactions (for example, allergic exanthema, dermatitis, urticaria, itching, psoriasis-like and lichen-like skin lesions, alopecia); very rare – erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrolysis.
From the musculoskeletal system: frequent – pain in the extremities.
From the urinary system: common – urinary tract infections, urinary disorders, renal failure and impaired renal function in patients with diffuse vasculitis and/or impaired renal function; very rarely – urinary incontinence in women (reversible after discontinuation of the drug).
From the genital organs and breast: uncommon – erectile dysfunction.
Metabolism and nutrition: common – hypercholesterolemia, hyperglycemia or hypoglycemia in patients with diabetes mellitus.
General disorders: very common – asthenia, increased fatigue; frequent – weight gain.
Dizziness, fainting, headache and usually mild asthenia occur more often at the beginning of therapy with Carvedilol Zentiva.
When using the drug in patients with chronic heart failure and low blood pressure (systolic blood pressure < 100 mm Hg), coronary artery disease and diffuse vascular changes and/or renal failure, reversible impairment of renal function was observed.
The presence of beta-adrenergic blocking properties of the drug does not exclude the possibility of manifestation of latent diabetes mellitus, decompensation of existing diabetes mellitus, or suppression of the contrainsular system.
Interaction
Interaction
Carvedilol may potentiate the effect of other concomitantly taken antihypertensive drugs or drugs that have a hypotensive effect (nitrates).
When carvedilol and diltiazem are used together, cardiac conduction disturbances and hemodynamic disturbances may develop.
When carvedilol and digoxin are taken simultaneously, the concentration of the latter increases and the atrioventricular conduction time may increase.
Carvedilol may potentiate the effect of insulin and oral hypoglycemic agents, and the symptoms of hypoglycemia (especially tachycardia) may be masked; therefore, regular monitoring of blood sugar levels is recommended in patients with diabetes mellitus.
Inhibitors of microsomal oxidation (cimetidine) enhance, and inducers (phenobarbital, rifampicin) weaken the hypotensive effect of carvedilol.
Drugs that reduce the content of catecholamines (reserpine, monoamine oxidase inhibitors) increase the risk of developing arterial hypotension and severe bradycardia.
With simultaneous use of cyclosporine, the concentration of the latter increases (adjustment of the daily dose of cyclosporine is recommended).
Concomitant administration of clonidine may potentiate the antihypertensive and heart rate-lowering effects of carvedilol.
General anesthetics enhance the negative inotropic and hypotensive effect of carvedilol.
Overdose
Overdose
Symptoms:
decreased blood pressure (accompanied by dizziness or fainting), bradycardia. Shortness of breath may occur due to bronchospasm and vomiting. In severe cases, cardiogenic shock, respiratory failure, confusion, and conduction disturbances are possible.
Treatment:
it is necessary to monitor and correct vital signs, if necessary, in the intensive care unit. Treatment is symptomatic. It is advisable to use intravenously m-anticholinergic agents (atropine), adrenergic agonists (epinephrine, norepinephrine).
Storage conditions
Storage conditions
Store in a dry place, protected from light, at a temperature not exceeding 25° C.
Manufacturer
Manufacturer
Vertex, Russia
Additional information
| Conditions of storage | Store in a dry place, protected from light, at a temperature not exceeding 25 ° C. |
|---|---|
| Manufacturer | Vertex, Russia |
| Medication form | pills |
| Brand | Vertex |
Other forms…
Related products
Buy Carvedilol-Vertex, tablets 12.5mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.