No products in the cart.
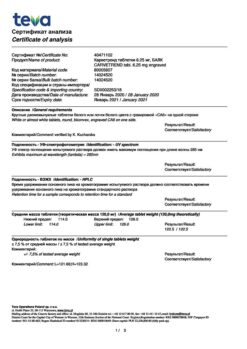
Carvedilol, tablets 12.5mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacodynamics
Carvedilol blocks alpha-1-, beta-1- and beta-2-adrenoreceptors. It has vasodilatory, antianginal and antiarrhythmic effects. The vasodilatory effect is mainly due to blockade of alpha 1-receptors. Due to vasodilatation, it reduces total peripheral vascular resistance (TPRR). It has no sympathomimetic activity of its own and has membrane stabilizing properties. The combination of vasodilation and beta-adrenoreceptor blockade leads to the following effects: in patients with arterial hypertension, the decrease in arterial pressure (BP) is not accompanied by an increase in PPS, peripheral blood flow is not reduced (unlike beta-adrenoblockers). HR decreases insignificantly. In patients with coronary artery disease it has antianginal action. Reduces pre- and post-load on the heart. It has no pronounced effect on lipid metabolism and blood plasma levels of potassium, sodium and magnesium. In patients with left ventricular dysfunction or circulatory insufficiency, it has a favorable effect on hemodynamic parameters and improves the ejection fraction and left ventricular size. It has an antioxidant effect by eliminating free oxygen radicals.
Pharmacokinetics
Carvedilol is rapidly and almost completely absorbed after oral administration from the gastrointestinal tract. It is almost completely bound to blood plasma proteins (98-99%). The plasma concentration is proportional to the dose taken. Bioavailability is about 25% due to high metabolism in the liver. Metabolites with high ability to block beta-adrenoreceptors are formed.
The maximum concentration in plasma is reached after 1 hour. Half-life period is 6-10 hours.
In elderly patients, the plasma concentration of carvedilol is approximately 50% higher than in younger patients. It is excreted mainly with bile. In patients with impaired liver function the bioavailability may increase to 80%. It penetrates through the placental barrier and is excreted with breast milk. Food slows absorption of the drug, but does not affect its bioavailability.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
Orally, regardless of meals.
Strictly follow the instructions of your physician. You should not stop the treatment with Carvedilol or change its dosage without first consulting your doctor. If it is necessary to cancel the drug, the dose should be reduced gradually over a period of 1 to 2 weeks.
If there is no therapeutic effect of treatment or a worsening of your condition is noted, consult your doctor.
Arterial hypertension.
The dose is adjusted individually. For the first 7-14 days, the recommended dose of Carvedilol is 12.5 mg (1 tablet of 12.5 mg) taken in the morning after breakfast. The dose may be divided into two doses of 6, 25 mg of Carvedilol (1/2 tablet of 12.5 mg). Further treatment should be carried out with Carvedilol in a dose of 25 mg (1 tablet of 25 mg) in the morning or divided into two doses of 12.5 mg of the drug (1 tablet of 12.5 mg). If necessary, after 14 days, the doctor may increase the dose again.
Take the drug after meals with a small amount of liquid.
Stable angina pectoris. The initial dose of Carvedilol is 12.5 mg (1 tablet of 12.5 mg) twice a day. After 7-14 days, under medical control, the dose of Carvedilol can be increased to 25 mg (1 tablet of 25 mg) twice a day. After 14 days, in case of insufficient effectiveness and good tolerability, the dose of Carvedilol can be further increased.
The total daily dose of Carvedilol for angina should not exceed 50 mg of the drug (2 tablets of 25 mg) administered twice a day. If your age exceeds 70 years, the daily dose of Carvedilol should not exceed 25 mg (1 tablet of 25 mg) twice a day.
If you have missed your next dose, you should take the drug as soon as possible.
However, if the time for the next dose is approaching, you should take only that dose, without doubling it.
You must take the medication regularly. If you have not taken the drug for more than 2 weeks, you should resume treatment with the lowest dose.
Chronic heart failure. The dose is adjusted individually, under the close supervision of a physician. The recommended starting dose is 3.125 mg 2 times a day for 2 weeks. If tolerated well, the dose is increased at intervals of at least 2 weeks to 6.25 mg 2 times a day, then to l2.5 mg 2 times a day, then to 25 mg 2 times a day. The dose should be increased to the maximum that is well tolerated by the patient. In patients with body weight less than 85 kg the target dose is 50 mg per day; in patients with body weight over 85 kg the target dose is 75-100 mg per day.
If treatment is interrupted for more than 2 weeks, treatment is restarted with a dose of 3.125 mg twice daily, with subsequent dose increases.
Interaction
Interaction
Carvedilol may potentiate the effect of other simultaneously taken antihypertensive agents or drugs that have a hypotensive effect (nitrates).
Concomitant use of carvedilol and diltiazem may lead to cardiac conduction abnormalities and hemodynamic disorders.
Concomitant administration of carvedilol and digoxin increases the concentration of the latter and may increase atrioventricular conduction time.
Carvedilol may potentiate the effects of insulin and oral hypoglycemic agents, and the symptoms of hypoglycemia (especially tachycardia) may mask, therefore regular monitoring of blood sugar levels is recommended in diabetic patients.
Microsomal oxidation inhibitors (cimetidine) enhance and inducers (phenobarbital, rifampicin) weaken the hypotensive effect of carvedilol.
Drugs that reduce catecholamines (reserpine, monoamine oxidase inhibitors) increase the risk of arterial hypotension and marked bradycardia.
Concomitant use of cyclosporine increases the concentration of the latter (correction of daily dose of cyclosporine is recommended).
Concomitant administration of clonidine may potentiate antihypertensive and heart rate-lowering effects of carvedilol.
General anesthetics enhance the negative inotropic and hypotensive effects of carvedilol.
Special Instructions
Special Instructions
The therapy should be prolonged and should not be stopped abruptly, especially in patients with coronary heart disease, as this may worsen the course of the underlying disease. If necessary, reduction of the drug dose should be gradual, over 1-2 weeks.
At the beginning of therapy with carvedilol or when increasing the drug dose, patients, especially elderly patients, may have an excessive decrease in blood pressure, predominantly when standing up. Correction of the drug dose is necessary. Patients with chronic heart failure may experience an increase in symptoms of heart failure and edema when adjusting the dose. In this case the dose of carvedilol should not be increased, it is recommended to prescribe high doses of diuretics until the patient’s condition stabilizes.
Continuous monitoring of electrocardiogram and blood pressure is recommended with simultaneous administration of carvedilol and slow calcium channel blockers, phenylalkylamine derivatives (verapamil) and benzodiazepine (diltiazem), and also with class I antiarrhythmic agents.
It is recommended to monitor renal function in patients with chronic renal failure, arterial hypotension and chronic heart failure.
If surgery is performed using general anesthesia, the anesthesiologist should be advised of prior therapy with Carvedilol.
Carvedilol does not affect blood glucose concentration and does not cause changes in glucose tolerance test in patients with insulin-independent diabetes mellitus.
At the time of treatment avoid the use of ethanol.
Patients with pheochromocytoma should be prescribed alpha-adrenoblockers before therapy.
Patients who wear contact lenses should note that the drug may cause decreased tear production.
It is not recommended to drive at the beginning of therapy and when increasing the dose of carvedilol. Other activities requiring high concentration and rapid psychomotor reactions should be refrained from.
Contraindications
Contraindications
With caution
Bronchospastic syndrome, chronic bronchitis, pulmonary emphysema, Prinz-metal angina, thyrotoxicosis, peripheral vascular occlusive disease, pheochromocytoma, psoriasis, renal failure, 1st degree atrioventricular block, extensive surgery and general anesthesia, diabetes, hypoglycemia, depression, myasthenia.
Side effects
Side effects
Immune system disorders: very rare – hypersensitivity.
Hematopoietic system: frequent – anemia; rare – thrombocytopenia; very rare – leukopenia.
Nervous system disorders: very frequent – dizziness, headache; infrequent – fainting state, syncope, paresthesias.
An organ of vision: frequent – visual disturbances, decreased lacrimation (dry eyes), eye irritation.
Cardiovascular system disorders: very frequent – heart failure during dose escalation, marked BP reduction; frequent – bradycardia, edema, hypervolemia, fluid retention, orthostatic hypotension, peripheral circulatory disorders (limb coldness, peripheral vascular disease, worsening of intermittent claudication and Raynaud syndrome); infrequent – AV blockade of degree II-III, angina pectoris.
Respiratory system disorders: frequent – shortness of breath, pulmonary edema, asthma in susceptible patients, bronchitis, pneumonia, upper respiratory tract infections; rare – nasal congestion.
Digestive system disorders: frequent – nausea, diarrhea, vomiting, dyspepsia, abdominal pain; infrequent – constipation, dry mouth.
Hepatic and biliary tract disorders: very rare – increased ALT, AST and GGT activity.
Skin and subcutaneous tissue disorders: infrequent – skin reactions (e.g., allergic exanthema, dermatitis, urticaria, pruritus, psoriasis-like and scaly-like skin lesions, alopecia); very rare – erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrolysis.
Muscular system disorders: frequent – pain in the extremities.
Perior urinary system disorders: frequent – urinary tract infections, urinary disorders, renal failure and renal dysfunction in patients with diffuse vasculitis and/or impaired renal function; very rare – urinary incontinence in women (reversible after drug withdrawal).
Gender and mammary gland disorders: infrequent – erectile dysfunction.
Metabolism and nutrition: frequent – hypercholesterolemia, hyperglycemia or hypoglycemia in patients with diabetes.
General disorders: very frequent – asthenia, increased fatigue; frequent – weight gain.
Dizziness, fainting, headache, and asthenia of usually mild degree occur more frequently at the beginning of therapy with Carvedilol Zentiva.
In patients with chronic heart failure and low BP (systolic BP)
The beta adreno-blocker properties of the drug do not exclude the possibility of manifestation of latent diabetes mellitus, decompensation of existing diabetes mellitus, or suppression of the counterinsulatory system.
Overdose
Overdose
Similarities
Similarities
Additional information
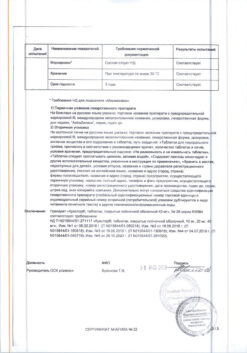
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | Store in a dry place, protected from light, at a temperature not exceeding 25 ° C. |
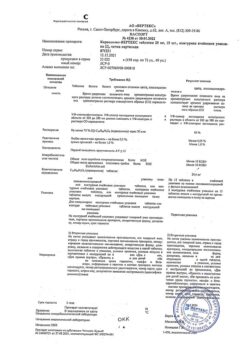
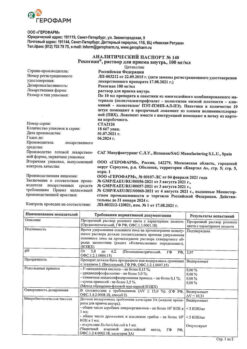
| Manufacturer | Pranapharm, Russia |
| Medication form | pills |
| Brand | Pranapharm |
Other forms…
Related products
Buy Carvedilol, tablets 12.5mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.