No products in the cart.
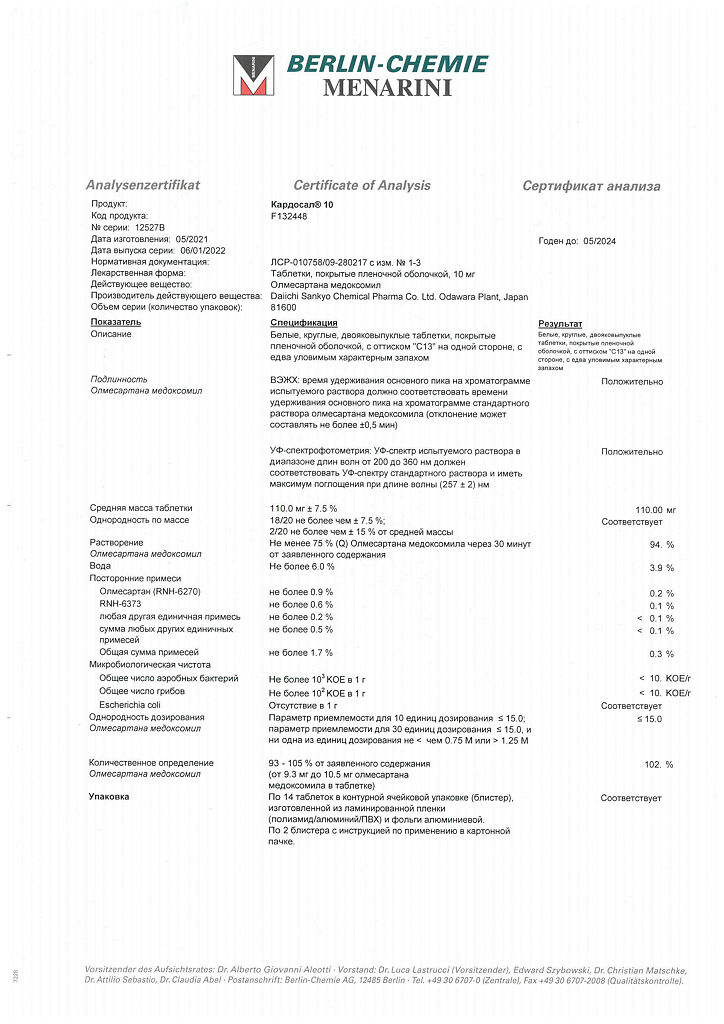
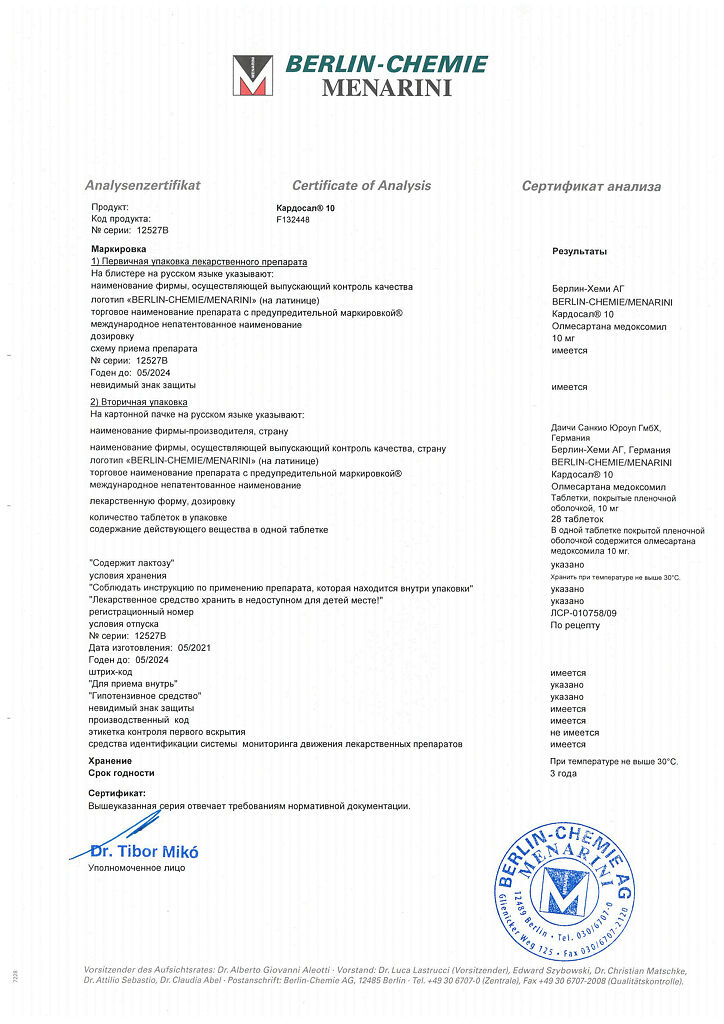
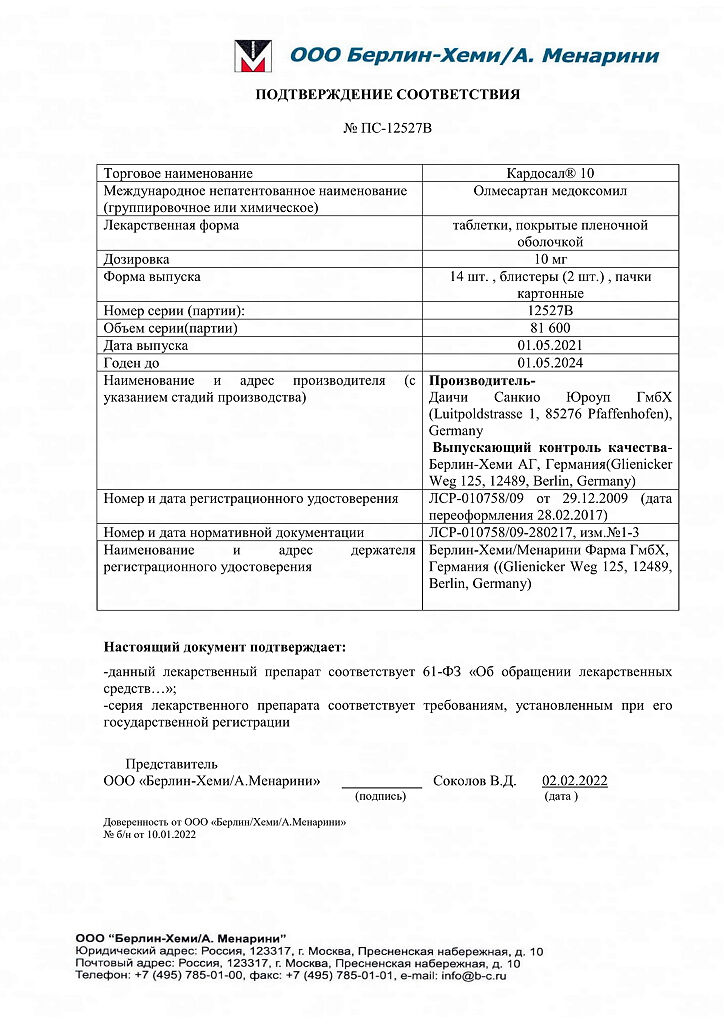
Cardosal 10,10 mg 28 pcs
€25.36 €21.13
Description
An angiotensin II receptor antagonist (AT1 type). Angiotensin II is the primary vasoactive hormone of the RAAS and plays a significant role in the pathophysiology of arterial hypertension via AT1 receptors. Olmesartan is thought to block all angiotensin II effects mediated by AT1 receptors regardless of the source and pathway of angiotensin II synthesis.
In arterial hypertension, olmesartan causes a dose-dependent prolonged decrease in BP. There is no evidence of arterial hypotension after the first dose, of tachycardia during long-term treatment (for Cardosal® 20 and Cardosal® 40) and of abstinence syndrome (rapid increase of BP after drug withdrawal).
Medoxomil olmesartan once daily effectively and gently reduces BP over 24 hours, and the effect after a single dose is similar to that of twice daily administration at the same daily dose.
The hypotensive effects of olmesartan generally develop as early as 2 weeks, with maximal effect after approximately 8 weeks of therapy.
Pharmacokinetics
Absorption and distribution
Olmesartan medoxomil is a prodrug. It is rapidly converted to the pharmacologically active metabolite olmesartan by enzymes in the intestinal mucosa and in the portal blood during absorption from the GI tract. Olmesartan medoxomil was not detected in unchanged form in plasma. The bioavailability of olmesartan averages 25.6%. Cmax of olmesartan in plasma is reached on average 2 hours after oral administration of olmesartan medoxomil and increases approximately linearly with increasing single dose up to 80 mg.
Eating has no significant effect on the bioavailability of olmesartan, so olmesartan medoxomil can be taken regardless of meals.
There are no clinically significant differences in the pharmacokinetic parameters of olmesartan according to gender.
Olmesartan binds to plasma proteins (99.7%), but the potential for clinically significant shifts in protein binding magnitude when interacting olmesartan with other highly bindable and concomitantly used drugs is low (this is confirmed by the absence of clinically significant interaction between olmesartan and warfarin). Binding of olmesartan to blood cells is insignificant.
Metabolism and excretion
Total plasma clearance is typically 1.3 L/h (coefficient of variation is 19%) and is relatively low compared to hepatic blood flow (approximately 90 L/h). Renal excretion is approximately 40%, with bile about 60%. Intrahepatic circulation of olmesartan is minimal. Since most of olmesartan is excreted through the liver, its use in patients with biliary obstruction is contraindicated.
The T1/2 of olmesartan is 10-15 h after multiple oral administration. Meaningful effect of therapy is achieved after the first few doses of the drug, and no further cumulation is observed after 14 days of repeated use. Renal clearance is approximately 0.5-0.7 l/h and is independent of the drug dose.
Pharmacokinetics in Special Clinical Cases
In patients with impaired renal function, the AUC at steady state (steady state) was increased by approximately 62%, 82% and 179% for mild, moderate and severe renal impairment, respectively, compared to healthy volunteers.
After a single oral dose, AUC values for olmesartan were 6% and 65% higher in patients with mild and moderate hepatic impairment, respectively, compared to healthy volunteers. The unbound fraction of olmesartan 2 hours after a dose of the drug in healthy volunteers and in patients with mild and moderate hepatic impairment was 0.26%, 0.34% and 0.41%, respectively.
Indications
Indications
Essential arterial hypertension.
Pharmacological effect
Pharmacological effect
Angiotensin II receptor antagonist (type AT1). Angiotensin II is the primary vasoactive hormone of the RAAS and plays a significant role in the pathophysiology of arterial hypertension through AT1 receptors. It is assumed that olmesartan blocks all effects of angiotensin II mediated by AT1 receptors, regardless of the source and pathway of angiotensin II synthesis.
In arterial hypertension, olmesartan causes a dose-dependent, long-term decrease in blood pressure. There is no evidence of the development of arterial hypotension after taking the first dose of the drug, of tachycardia during long-term treatment (for the drugs Cardosal® 20 and Cardosal® 40) and of the development of withdrawal syndrome (a sharp increase in blood pressure after discontinuation of the drug).
Taking olmesartan medoxomil 1 time/day provides an effective and mild reduction in blood pressure within 24 hours, and the effect after a single dose is similar to the effect of taking the drug 2 times/day at the same daily dose.
The hypotensive effect of olmesartan usually develops within 2 weeks, and the maximum effect develops approximately 8 weeks after the start of therapy.
Pharmacokinetics
Suction and distribution
Olmesartan medoxomil is a prodrug. It is rapidly converted to the pharmacologically active metabolite olmesartan by enzymes in the intestinal mucosa and in portal blood during absorption from the gastrointestinal tract. Olmesartan medoxomil was not detected unchanged in blood plasma. The bioavailability of olmesartan averages 25.6%. Cmax of olmesartan in blood plasma is achieved on average 2 hours after oral administration of olmesartan medoxomil and increases approximately linearly with increasing single dose to 80 mg.
Food intake does not have a significant effect on the bioavailability of olmesartan, therefore olmesartan medoxomil can be taken regardless of meals.
There were no clinically significant differences in the pharmacokinetic parameters of olmesartan depending on gender.
Olmesartan is bound to plasma proteins (99.7%), but the potential for a clinically significant shift in the magnitude of protein binding when olmesartan interacts with other highly binding and concomitantly used drugs is low (this is confirmed by the lack of clinically significant interaction between olmesartan and warfarin). The association of olmesartan with blood cells is insignificant.
Metabolism and excretion
Total plasma clearance is typically 1.3 L/h (coefficient of variation – 19%) and is relatively low compared with hepatic blood flow (approximately 90 L/h). Renal excretion is approximately 40%, bile excretion is about 60%. Intrahepatic circulation of olmesartan is minimal. Since most of olmesartan is eliminated through the liver, its use in patients with biliary obstruction is contraindicated.
T1/2 of olmesartan is 10-15 hours after repeated oral administration. A significant effect of therapy is achieved after taking the first few doses of the drug, and after 14 days of repeated use, no further accumulation is observed. Renal clearance is approximately 0.5-0.7 l/h and is independent of the dose of the drug.
Pharmacokinetics in special clinical situations
In patients with renal impairment, steady-state AUC was increased by approximately 62%, 82%, and 179% for mild, moderate, and severe renal impairment, respectively, compared with healthy volunteers.
After a single oral dose, the AUC values for olmesartan were 6% and 65% higher in patients with mild and moderate hepatic impairment, respectively, compared to healthy volunteers. The unbound fraction of olmesartan 2 hours after dosing in healthy volunteers and in patients with mild and moderate hepatic impairment was 0.26%, 0.34% and 0.41%, respectively.
Special instructions
Special instructions
Symptomatic arterial hypotension, especially after taking the first dose of the drug, may occur in patients with reduced blood volume and/or reduced sodium levels due to intensive diuretic therapy, restriction of dietary salt intake during dietary nutrition, and also due to diarrhea or vomiting. Relevant factors should be eliminated before using Cardosal®.
In patients whose vascular tone and renal function depend largely on the activity of the RAAS (for example, in patients with severe chronic heart failure or impaired renal function, including renal artery stenosis), treatment with other drugs acting on this system is associated with the possibility of developing acute arterial hypotension, azotemia, oliguria or, in rare cases, acute renal failure. The possibility of a similar effect cannot be excluded when using angiotensin II receptor antagonists.
There is an increased risk of severe hypotension and renal failure if a patient with bilateral renal artery stenosis or arterial stenosis of a single functioning kidney is treated with drugs that affect the RAAS.
When using the drug Cardosal® in patients with impaired renal function, it is recommended to periodically monitor the level of potassium and creatinine in the blood serum. There is no experience with the use of Cardosal® in patients with recent kidney transplantation or in patients with late-stage renal impairment (for example, creatinine clearance less than 12 ml/min).
As with other angiotensin II receptor antagonists and ACE inhibitors, hyperkalemia may develop during treatment with Cardosal if the patient suffers from impaired renal function and/or chronic heart failure. In patients at this risk group, monitoring serum potassium levels is recommended.
As with other angiotensin II receptor antagonists, the combination of lithium and Cardosal® is not recommended.
As with other angiotensin II receptor antagonists, in black patients suffering from arterial hypertension, the effectiveness of therapy with Cardosal® is slightly lower than in patients of other races.
As with any antihypertensive drug, excessive reduction of blood pressure in patients with coronary artery disease or cerebrovascular insufficiency can lead to myocardial infarction or stroke.
Impact on the ability to drive vehicles and other mechanisms that require increased concentration of attention
The effect of the drug Cardosal® on the ability to drive vehicles and operate machinery has not been studied, therefore, during treatment with the drug Cardosal®, caution should be exercised when driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions (dizziness and weakness are possible).
Active ingredient
Active ingredient
Olmesartan medoxomil
Composition
Composition
Active ingredients:
olmesartan medoxomil 10 mg.
Excipients:
microcrystalline cellulose – 10 mg,
low-substituted hyprolose – 20 mg,
lactose monohydrate – 61.6 mg,
hyprolose 6-10 mPa×s – 2.5 mg,
magnesium stearate – 0.9 mg.
Film shell composition:
hypromellose 5 mPa×s – 3.6 mg,
talc – 0.7 mg,
titanium dioxide (E171) – 0.7 mg.
Pregnancy
Pregnancy
There is no experience with the use of olmesartan medoxomil in pregnant women. However, due to existing reports of severe teratogenic effects of drugs acting directly on the renin-angiotensin system, like any drug of this class, olmesartan is contraindicated during pregnancy. If pregnancy occurs during therapy with Cardosal®, the drug must be discontinued.
There is no data on whether olmesartan is excreted in breast milk, therefore, if it is necessary to use the drug Cardosal® during lactation, breastfeeding should be discontinued while taking the drug.
Contraindications
Contraindications
Hypersensitivity to the active substance or to any of the excipients included in the drug;
obstruction of the biliary tract;
renal failure (creatinine clearance less than 20 ml/min), condition after kidney transplantation (no experience of clinical use);
lactase deficiency, galactosemia or malabsorption syndrome;
pregnancy and lactation;
age under 18 years (efficacy and safety have not been established).
The drug should be used with caution in the following conditions or diseases: stenosis of the aortic or mitral valves; hypertrophic obstructive cardiomyopathy; primary aldosteronism; hyperkalemia, hyponatremia (risk of dehydration, arterial hypotension, renal failure); renal failure (creatinine clearance more than 20 ml/min); chronic heart failure; bilateral renal artery stenosis or stenosis of the artery of a single kidney; IHD; cerebrovascular diseases; old age (over 65 years); liver dysfunction; conditions accompanied by a decrease in blood volume (including diarrhea, vomiting), as well as when following a sodium-restricted diet; simultaneous use with diuretics.
Side Effects
Side Effects
Possible side effects are listed below in descending order of frequency:
very often (> 1/10);
often (> 1/100 < 1/10);
sometimes (> 1/1000, < 1/100);
rare (> 1/10,000, < 1/1000);
very rare (<1/10,000), including isolated reports.
From the hematopoietic system: very rarely – thrombocytopenia.
From the side of the central nervous system: sometimes – dizziness; very rarely – headache.
From the respiratory system: often – pharyngitis, rhinitis; very rarely – cough, bronchitis.
From the digestive system: often – diarrhea, dyspepsia, gastroenteritis; very rarely – abdominal pain, nausea, vomiting.
From the skin: very rarely – itching, rash, angioedema, allergic dermatitis, urticaria.
From the musculoskeletal system: often – back pain, bone pain, arthralgia, arthritis; very rarely – muscle cramps, myalgia.
From the urinary system: often – hematuria, urinary tract infection; very rarely – acute renal failure.
From laboratory parameters: very rarely – increased levels of creatinine and urea in the blood serum, increased activity of liver enzymes.
From the cardiovascular system: sometimes – angina, tachycardia; rarely – a pronounced decrease in blood pressure.
Metabolism: often – increased CPK levels, hypertriglyceridemia, hyperuricemia; rarely – hyperkalemia.
From the body as a whole: often – chest pain, flu-like symptoms, peripheral edema; very rarely – asthenia, fatigue, malaise, drowsiness.
Interaction
Interaction
Concomitant use with potassium-sparing diuretics, potassium supplements, salt substitutes containing potassium, or other drugs that can increase serum potassium levels (for example, heparin) is not recommended; this may lead to an increase in serum potassium levels.
The antihypertensive effect of olmesartan therapy can be enhanced when used in combination with other antihypertensive drugs.
NSAIDs, including acetylsalicylic acid in doses greater than 3 g/day, as well as COX-2 inhibitors and angiotensin II receptor antagonists may act synergistically to reduce glomerular filtration. With the simultaneous use of NSAIDs and angiotensin II receptor antagonists, there may be a risk of developing acute renal failure, therefore monitoring of renal function at the beginning of treatment, as well as regular intake of sufficient fluids, is recommended. However, simultaneous treatment may reduce the antihypertensive effect of angiotensin II receptor antagonists, leading to a partial loss of their therapeutic effectiveness.
When used simultaneously with antacids (magnesium and aluminum hydroxide), a moderate decrease in the bioavailability of olmesartan is possible.
There are reports of a reversible increase in serum lithium concentrations and toxicity during simultaneous use of lithium preparations with ACE inhibitors and angiotensin II receptor antagonists, therefore the use of olmesartan medoxomil in combination with lithium preparations is not recommended. If appropriate combination therapy is necessary, regular monitoring of serum lithium levels is recommended.
Overdose
Overdose
Symptoms: marked decrease in blood pressure.
Treatment: with a pronounced decrease in blood pressure, it is recommended to place the patient on his back with his legs elevated.
Gastric lavage and/or intake of activated carbon, therapy aimed at correcting dehydration and disturbances in water-salt metabolism, and replenishing blood volume are recommended.
Storage conditions
Storage conditions
At a temperature not exceeding 30 °C
Shelf life
Shelf life
3 years
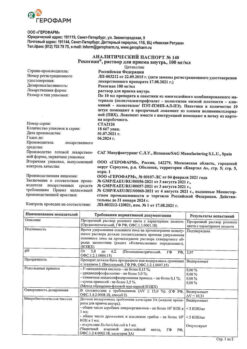
Manufacturer
Manufacturer
Berlin-Chemie AG/Daichi Sankyo Europe GmbH, Germany
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Daichi Sankio Europe GmbH, Germany |
| Medication form | pills |
| Brand | Daichi Sankio Europe GmbH |
Related products
Buy Cardosal 10,10 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.