No products in the cart.
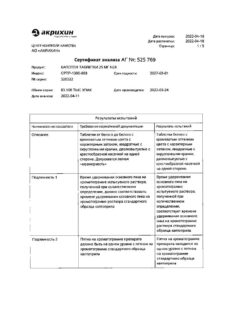
Captopril Welfarm, tablets 50 mg 40 pcs
€6.49 €5.68
Description
Pharmacotherapeutic group: angiotensin-converting enzyme inhibitor (ACE inhibitor)
ATX code: C09AA01
Pharmacological properties Pharmacodynamics
First generation angiotensin-converting enzyme (ACE) inhibitor containing a sulfhydryl group (SH-group). It has an antihypertensive effect.
Inhibiting ACE reduces the conversion of angiotensin I to angiotensin II and eliminates its vasoconstrictor effect on arterial and venous vessels. As a result of decreased concentration of angiotensin II, there is a secondary increase in plasma renin activity (due to elimination of negative feedback of renin release), which leads to a direct reduction of aldosterone secretion by the adrenal cortex. This reduces total peripheral vascular resistance (PPR) and arterial pressure (BP), resistance in the pulmonary vessels, and decreases the post- and preload on the heart. Increases cardiac output and exercise tolerance.
Dilates arteries to a greater extent than veins. Causes a decrease in bradykinin degradation (one of the effects of ACE) and an increase in prostaglandin synthesis.
The antihypertensive effect does not depend on the activity of plasma renin; the decrease of BP is observed with normal and even reduced activity of the hormone due to the effect on tissue renin-angiotensin-aldosterone system (RAAS).
It enhances coronary and renal blood flow. With long-term use, it reduces the severity of myocardial hypertrophy and arterial wall resistance, prevents the progression of heart failure and slows the development of left ventricular dilatation.
It improves blood supply to ischemic myocardium. Reduces platelet aggregation. Helps reduce sodium ions in patients with heart failure.
Decreases the tone of the renal tubular arterioles, thus improving intra-column hemodynamics and prevents the development of diabetic nephropathy. In doses of 50 mg/day it shows angioprotective properties against the vessels of the microcirculatory bed and allows to slow the progression of chronic renal failure in diabetic nephroangiopathy.
The decrease of BP in contrast to direct vasodilators (hydralazine, minoxidil, etc.) is not accompanied by reflex tachycardia and leads to reduction of myocardial oxygen demand. In heart failure, an adequate dose has no effect on BP. Maximum BP reduction is observed 60-90 minutes after oral administration. The duration of antihypertensive effect depends on the dose of the drug taken and reaches optimal values within a few weeks of therapy.
Discontinuation of captopril should not be abrupt, as this may cause a significant increase in BP.
Pharmacokinetics
Absorption is fast and is about 75% of the administered dose (absorption of the drug is reduced by 30-40% if it is taken with food simultaneously), bioavailability is 35-40% (effect of “primary passage” through the liver). Binding with plasma proteins (mainly with albumin) is 25-30%. Time to reach maximum plasma concentration (Cmax = 114 ng/ml) when administered orally is 30-90 min. Less than 0.002% of the administered dose of captopril is secreted with breast milk. Across the blood-brain barrier and placental barrier penetration is insignificant (less than 1%).
Metabolized in the liver with the formation of captopril disulfide dimer and captopril-cysteine sulfide. Metabolites are pharmacologically inactive.
Half-life of captopril is about 2-3 hours. About 95% is excreted by kidneys during the first day, 40-50% of them are unchanged, the rest – as metabolites. In daily urine 38 % of unchanged captopril and 62 % as metabolites are determined.
Cumulates in chronic renal failure. The half-life in renal failure is 3.5-32 hours, so patients with impaired renal function should reduce the dose of the drug and/or increase the interval between doses.
Indications
Indications
– Arterial hypertension (including renovascular).
– Chronic heart failure (as part of complex therapy).
– Impaired left ventricular function after myocardial infarction in a clinically stable condition.
– Diabetic nephropathy due to type 1 diabetes mellitus (with albuminuria more than 30 mg/day).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: angiotensin-converting enzyme inhibitor (ACE inhibitor)
ATX code: C09AA01
Pharmacological properties Pharmacodynamics
A first-generation angiotensin-converting enzyme (ACE) inhibitor containing a sulfhydryl group (SH group). Has an antihypertensive effect.
By inhibiting ACE, it reduces the conversion of angiotensin I to angiotensin II and eliminates its vasoconstrictor effect on arterial and venous vessels. As a result of a decrease in the concentration of angiotensin II, a secondary increase in plasma renin activity occurs (due to the elimination of negative feedback during the release of renin), which leads to a direct decrease in the secretion of aldosterone by the adrenal cortex. At the same time, total peripheral vascular resistance (TPVR) and blood pressure (BP), resistance in the pulmonary vessels decrease, and post- and preload on the heart decreases. Increases cardiac output and exercise tolerance.
Dilates arteries more than veins. Causes a decrease in the degradation of bradykinin (one of the effects of ACE) and an increase in the synthesis of prostaglandin.
The antihypertensive effect does not depend on the activity of plasma renin; a decrease in blood pressure is observed with normal and even reduced hormone activity, which is due to the effect on the tissue renin-angiotensin-aldosterone system (RAAS).
Strengthens coronary and renal blood flow. With long-term use, it reduces the severity of myocardial hypertrophy and the walls of resistive arteries, prevents the progression of heart failure and slows down the development of left ventricular dilatation.
Improves blood supply to ischemic myocardium. Reduces platelet aggregation. Helps reduce sodium ion levels in patients with heart failure.
Reduces the tone of the efferent arterioles of the glomeruli of the kidneys, thereby improving intraglomerular hemodynamics, and prevents the development of diabetic nephropathy. At doses of 50 mg/day, it exhibits angioprotective properties against microcirculatory vessels and helps slow the progression of chronic renal failure in diabetic nephroangiopathy.
A decrease in blood pressure, unlike direct vasodilators (hydralazine, minoxidil, etc.), is not accompanied by reflex tachycardia and leads to a decrease in myocardial oxygen demand. In case of heart failure in an adequate dose, it does not affect blood pressure. The maximum reduction in blood pressure is observed 60-90 minutes after oral administration. The duration of the antihypertensive effect depends on the dose of the drug taken and reaches optimal values within several weeks of therapy.
Captopril should not be discontinued abruptly, as this may cause a significant increase in blood pressure.
Pharmacokinetics
Absorption is rapid, accounting for about 75% of the dose taken (when taken simultaneously with food, absorption of the drug is reduced by 30-40%), bioavailability is 35-40% (the “first pass” effect through the liver). Communication with blood plasma proteins (mainly albumin) – 25-30%. The time to reach maximum concentration in blood plasma (Cmax = 114 ng/ml) when taken orally is 30-90 minutes. Less than 0.002% of the administered dose of captopril is secreted into breast milk. It penetrates slightly through the blood-brain barrier and placental barrier (less than 1%).
Metabolized in the liver to form the disulfide dimer of captopril and captopril-cysteine sulfide. Metabolites are pharmacologically inactive.
The half-life of captopril is approximately 2-3 hours. About 95% is excreted by the kidneys during the first day, of which 40-50% is unchanged, the rest is in the form of metabolites. In daily urine, 38% of unchanged captopril and 62% are determined in the form of metabolites.
Cumulates in chronic renal failure. The half-life for renal failure is 3.5-32 hours, so patients with impaired renal function should reduce the dose of the drug and/or increase the interval between doses.
Special instructions
Special instructions
Before starting, as well as regularly during treatment with Captopril Welfarm, blood pressure and kidney function should be regularly monitored. In patients with chronic heart failure, the drug is used under close medical supervision.
Arterial hypotension
In patients with arterial hypertension, when using the drug Captopril Velpharm, severe arterial hypotension is observed only in rare cases; the likelihood of developing this condition increases with a decrease in circulating blood volume and an imbalance in water and electrolyte balance (for example, after intensive treatment with diuretics), in patients with chronic heart failure or on hemodialysis. The possibility of a sharp decrease in blood pressure can be minimized by first withdrawing (4-7 days before) the diuretic or replenishing the volume of circulating blood (about a week before starting treatment), or by using the drug Captopril Velpharm in small doses at the beginning of treatment (6.25-12.5 mg/day).
A marked decrease in blood pressure when using antihypertensive drugs in patients with cerebrovascular accidents and cardiovascular diseases may increase the risk of myocardial infarction or stroke. If arterial hypotension develops, the patient should take a horizontal position with legs elevated. Sometimes it may be necessary to replenish the volume of circulating blood.
Renovascular hypertension
There is an increased risk of developing hypertension and renal failure in patients with bilateral renal artery stenosis of a solitary kidney when using ACE inhibitors. Impaired renal function can occur with moderate changes in serum creatinine concentrations. In such patients, therapy should be initiated under close medical supervision with low doses, carefully titrated and with monitoring of renal function.
The simultaneous use of ACE inhibitors (including Captopril Velpharm) with drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal failure (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
Concomitant use of ACE inhibitors with angiotensin II receptor antagonists is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Renal dysfunction
In patients with renal failure or when taking high doses of ACE inhibitors (including Captopril Welfarm), proteinuria may occur. In most cases, proteinuria decreased or disappeared within 6 weeks, regardless of whether treatment with Captopril Welfarm was continued or not. Parameters of renal function, such as residual blood nitrogen and creatinine, rarely changed in patients with proteinuria. In patients with kidney disease, the protein content in the urine should be determined before starting therapy and periodically throughout the course of therapy.
Hyperkalemia
In some cases, when using the drug Captopril Velpharm, an increase in potassium levels in the blood serum is observed. The risk of developing hyperkalemia when using ACE inhibitors is increased in patients with renal failure and diabetes mellitus, as well as those taking potassium-sparing diuretics, potassium supplements and other drugs that cause an increase in potassium levels in the blood (for example, heparin). The simultaneous use of potassium-sparing diuretics and potassium supplements should be avoided. Use with caution in patients on a low-salt or salt-free diet (increased risk of hypotension and hyperkalemia).
Neutropenia/agranulocytosis
In the first 3 months of therapy, the number of leukocytes in the blood is monitored monthly, then once every 3 months. Neutropenia/agranulocytosis, anemia and thrombocytopenia have been reported in patients taking ACE inhibitors, including Captopril Welfarm. In patients with normal renal function and no other complicating factors, neutropenia rarely occurs. Captopril should be used with great caution in patients with connective tissue diseases who are simultaneously receiving immunosuppressive therapy (allopurinol or procainamide), especially with existing renal impairment. In such patients, a clinical blood test is monitored every 2 weeks in the first 3 months, then every 2 months. If the number of leukocytes is below 4.0 × 109 / L, a general blood test is indicated; below 1.0 × 109 / L, the drug is stopped. These patients may develop severe infections that do not respond to intensive antibiotic therapy. During treatment, all patients should be instructed that if signs of infection occur (eg, sore throat, fever), they should notify the physician and have a complete blood count performed. In most patients, the white blood cell count quickly returns to normal when treatment with Captopril is stopped.
Anaphylactoid reactions
Patients taking Captopril Welfarm against the background of desensitizing therapy with hymenoptera venom, etc., have an increased risk of developing anaphylactoid reactions. This can be avoided if you first temporarily stop taking the drug.
When performing hemodialysis in patients receiving Captopril Welfarm, the use of high permeability dialysis membranes (for example, AN69®) should be avoided, since in such cases the risk of developing anaphylactoid reactions increases. In rare cases, life-threatening anaphylactoid reactions may occur in patients receiving ACE inhibitors during low-density lipoprotein (LDL) apheresis using dextran sulfate. To prevent anaphylactoid reactions, ACE inhibitor therapy should be discontinued before each LDL apheresis procedure using high-flux membranes.
Angioedema
In patients taking Captopril Velpharm, the appearance of abdominal pain must be differentiated from intestinal angioedema.
If angioedema develops, the drug is discontinued and careful medical observation and symptomatic therapy are provided. If the swelling is localized on the face, special treatment is usually not required (antihistamines can be used to reduce the severity of symptoms); if the swelling spreads to the tongue, pharynx or larynx and there is a threat of developing airway obstruction and a threat to the patient’s life, epinephrine (adrenaline) should be immediately administered subcutaneously (0.5 ml in a dilution of 1:1000), and also make sure that the airways are clear.
It is recommended to stop taking ACE inhibitors, including Captopril Welfarm, 12 hours before surgery, warning the surgeon-anesthesiologist about the use of ACE inhibitors.
Cough
The development of a non-productive, prolonged cough when taking ACE inhibitors is reversible and resolves after discontinuation of treatment.
Diabetes mellitus
In patients with diabetes mellitus taking oral hypoglycemic agents or insulin, blood glucose concentrations should be regularly monitored during the first month of treatment with Captopril Welfarm.
Liver dysfunction
During therapy with ACE inhibitors, several cases of liver dysfunction with cholestatic jaundice, fulminant liver necrosis, sometimes fatal, have been reported.
If, during therapy with Captopril Velpharm, jaundice develops or the activity of “liver” transaminases increases, the drug should be discontinued immediately; the patient should be closely monitored and, if necessary, receive appropriate therapy.
Hypokalemia
The simultaneous use of an ACE inhibitor and a thiazide diuretic does not exclude the possibility of hypokalemia. It is recommended to regularly monitor potassium levels in the blood.
Surgery/anesthesia
Hypotension may occur in patients undergoing major surgery or during the use of anesthetics known to lower blood pressure. If arterial hypotension occurs, it is recommended to replenish the volume of circulating blood.
Ethnic differences
ACE inhibitors, including Captopril Welfarm, have a less pronounced antihypertensive effect in patients of the Black race, which is apparently due to the frequent occurrence of low renin activity in this group of patients.
Laboratory data
Captopril may cause a false-positive urine acetone test.
Impact on the ability to drive vehicles and machinery
During the treatment period, it is necessary to refrain from driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions, as dizziness is possible, especially after taking the initial dose.
Active ingredient
Active ingredient
Captopril
Composition
Composition
For one tablet:
Active ingredient: captopril (in terms of dry matter) – 50.0 mg,
Excipients: lactose monohydrate (milk sugar), microcrystalline cellulose, magnesium stearate, talc, colloidal silicon dioxide (Aerosil), crospovidone (Kollidon CL-M, Kollidon CL).
Pregnancy
Pregnancy
The use of Captopril Welfarm during pregnancy is contraindicated.
The drug Captopril Velpharm should not be used in the first trimester of pregnancy. There have been no adequate controlled studies of the use of ACE inhibitors in pregnant women. The limited available data on the effects of the drug in the first trimester of pregnancy indicate that the use of ACE inhibitors does not lead to fetal malformations associated with fetotoxicity. Epidemiological data demonstrating a risk of teratogenicity following first trimester exposure to ACE inhibitors have not been convincing, but some increased risk cannot be excluded.
The use of ACE inhibitors during pregnancy can lead to morbidity and death of the fetus and/or newborn. Long-term use of captopril in the second and third trimesters is toxic to the fetus (decreased renal function, oligohydramnios, delayed ossification of the skull bones) and newborns (neonatal renal failure, arterial hypotension, hyperkalemia).
In addition, the use of ACE inhibitors in the first trimester of pregnancy is associated with a potentially increased risk of developing congenital defects in the fetus.
Women planning pregnancy should not use ACE inhibitors (including Captopril Welfarm). Women of childbearing age should be aware of the potential dangers of using ACE inhibitors (including Captopril Welfarm). If pregnancy occurs while using Captopril Velpharm, the drug should be stopped as soon as possible and fetal development should be monitored regularly.
If the patient received the drug during the second and third trimesters of pregnancy, it is recommended to conduct an ultrasound examination to assess the condition of the skull bones and fetal kidney function.
If the use of an ACE inhibitor is considered necessary, patients planning pregnancy should be switched to alternative antihypertensive therapy that has an established safety profile for use during pregnancy. Approximately 1% of the administered dose of Captopril Welfarm is found in breast milk. Due to the risk of serious adverse reactions in the child, breastfeeding should be stopped or drug therapy should be discontinued in the mother during the period of breastfeeding.
Contraindications
Contraindications
– hypersensitivity to captopril, other components of the drug or other ACE inhibitors (including a history);
– hereditary and/or idiopathic angioedema, a history of angioedema (against the background of previous therapy with other ACE inhibitors);
– severe renal dysfunction, refractory hyperkalemia, bilateral renal artery stenosis, stenosis of a solitary kidney with progressive azotemia, condition after kidney transplantation, primary hyperaldosteronism;
– severe liver dysfunction;
– pregnancy;
– period of breastfeeding;
– age under 18 years (efficacy and safety have not been established);
– lactose intolerance, lactase deficiency or glucose-galactose malabsorption;
– simultaneous use of ACE inhibitors (including captopril) with aliskiren and aliskiren-containing drugs in patients with type 2 diabetes mellitus or impaired renal function (glomerular filtration rate (GFR) less than 60 ml/min/1.73 m2 body surface area) (see section “Interaction with other drugs”);
– simultaneous use with angiotensin II receptor antagonists (APA II) in patients with diabetic nephropathy.
With caution
Hypertrophic obstructive cardiomyopathy, connective tissue diseases (especially systemic lupus erythematosus or scleroderma), inhibition of bone marrow hematopoiesis (risk of developing neutropenia and agranulocytosis), cerebrovascular diseases, coronary heart disease, diabetes mellitus (increased risk of developing hyperkalemia), diet with limited salt, conditions accompanied by a decrease in circulating blood volume (including diarrhea, vomiting, in hemodialysis patients), mitral stenosis, aortic stenosis and similar changes obstructing the outflow of blood from the left ventricle of the heart, liver dysfunction, chronic renal failure, surgery/general anesthesia, hemodialysis using high-flux membranes (eg, AN69®), desensitization therapy, low-density lipoprotein (LDL) apheresis, administration potassium-sparing diuretics, potassium preparations, potassium-containing salt and lithium substitutes, hyperkalemia, renovascular hypertension, when used in black patients, in elderly patients (dose adjustment required).
Side Effects
Side Effects
According to the World Health Organization (WHO), adverse reactions are classified according to their frequency of development as follows: very often (≥ 1/10); often (≥ 1/100, < 1/10); uncommon (≥ 1/1000, < 1/100); rare (≥ 1/10000, < 1/1000); very rare (<1/10000), including isolated reports; unspecified frequency (frequency cannot be calculated from available data).
From the central nervous system: often – taste disorder, sleep disturbances, dizziness, drowsiness; rarely – headache, paresthesia, asthenia; very rarely – depression, cerebrovascular disorders, including stroke, fainting, impaired consciousness.
From the skin: often – skin itching with and without rashes, skin rash (maculopapular, less often – vesicular or bullous), baldness; very rarely – urticaria, Stevens-Johnson syndrome, erythema multiforme, photosensitivity, erythroderma, exfoliative dermatitis, pemphigoid reactions.
From the genitourinary system: rarely – impaired renal function, acute renal failure, polyuria, oliguria, increased frequency of urination; very rarely – nephrotic syndrome, sexual dysfunction, gynecomastia.
Metabolic disorders: rarely – anorexia; very rarely – hyperkalemia, hypoglycemia.
From the musculoskeletal system: very rarely – myalgia, arthralgia.
From the digestive system: often – dryness of the oral mucosa, nausea, vomiting, abdominal pain, diarrhea, constipation; rarely – stomatitis, aphthous ulcers of the inner surface of the mucous membrane of the cheeks and tongue, gum hyperplasia; very rarely – glossitis, peptic ulcer, pancreatitis, liver dysfunction, cholestasis, jaundice, hepatitis (including rare cases of hepatonecrosis), increased activity of liver transaminases, increased bilirubin concentration in the blood serum, angioedema of the intestinal mucosa.
From the hematopoietic organs: very rarely – neutropenia, agranulocytosis, pancytopenia, especially in patients with impaired renal function, anemia (including aplastic, hemolytic), thrombocytopenia, lymphadenopathy, eosinophilia, autoimmune diseases and/or increased titer for antinuclear antibodies.
From the respiratory system: often – dry, irritating (non-productive) cough, shortness of breath; very rarely – bronchospasm, rhinitis, allergic alveolitis, eosinophilic pneumonia, pulmonary edema.
From the senses: very rarely – impaired visual acuity.
From the cardiovascular system: infrequently – tachycardia or tachyarrhythmia, palpitations, angina pectoris, orthostatic hypotension, Raynaud’s syndrome, flushing of the face, pallor, peripheral edema; very rarely – cardiogenic shock, cardiac arrest.
Laboratory indicators: very rarely – proteinuria, eosinophilia, hyperkalemia, hyponatremia, hypoglycemia, increased concentrations of urea nitrogen and creatinine in the blood plasma, acidosis, decreased hemoglobin and hematocrit, decreased number of leukocytes, platelets, increased erythrocyte sedimentation rate (ESR).
Other: infrequently – chest pain, increased fatigue, weakness; very rarely – fever; frequency unknown – a complex of symptoms including facial flushing, nausea, vomiting and decreased blood pressure.
Interaction
Interaction
The simultaneous use of ACE inhibitors with other drugs that affect the RAAS, including angiotensin II receptor antagonists (ARA II) and aliskiren, leads to an increased incidence of cases of pronounced decrease in blood pressure, hyperkalemia, and renal dysfunction (including acute renal failure). It is necessary to monitor blood pressure, renal function, and plasma electrolyte levels when using captopril with other drugs that affect the RAAS.
The simultaneous use of ACE inhibitors with drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
Concomitant use of ACE inhibitors with angiotensin II receptor antagonists is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Combined use with potassium-sparing diuretics (triamterene, amiloride, spironolactone and its derivative eplerenone), potassium supplements, potassium supplements, salt substitutes (contain significant amounts of potassium ions) increases the risk of developing hyperkalemia. If it is necessary to use them simultaneously with captopril, plasma potassium levels should be monitored.
When using high doses of diuretics (thiazide diuretics, loop diuretics) simultaneously with captopril due to a reduced circulating blood volume, the risk of arterial hypotension increases, especially at the beginning of captopril therapy.
The antihypertensive effect of captopril is potentiated when used simultaneously with aldesleukin, alprostadil, beta-blockers, alpha1-blockers, central alpha2-adrenergic agonists, diuretics, cardiotonics, blockers of “slow” calcium channels, minoxidil, muscle relaxants, nitrates and vasodilators. Antidepressants, antipsychotics, anxiolytics and hypnotics can also enhance the antihypertensive effect of captopril.
With long-term use, the antihypertensive effect of captopril is weakened by indomethacin and other nonsteroidal anti-inflammatory drugs (NSAIDs), incl. selective cyclooxygenase-2 inhibitors (sodium ion retention, decreased prostaglandin synthesis, especially against the background of low renin activity) and estrogens.
NSAIDs and ACE inhibitors have been described to have an additive effect in increasing serum potassium while simultaneously decreasing renal function. These effects are reversible. Rarely, acute renal failure may occur, especially in patients with pre-existing renal impairment, in elderly patients or in patients with reduced circulating blood volume (dehydration).
The use of ACE inhibitors in patients undergoing surgery under general anesthesia can lead to a significant decrease in blood pressure, especially when using general anesthetic agents that have an antihypertensive effect.
Slows down the excretion of lithium drugs, increasing the concentration of lithium in the blood. If simultaneous use of captopril and lithium preparations is necessary, serum lithium concentrations should be carefully monitored.
When using captopril while taking allopurinol or procainamide, the risk of developing Stevens-Johnson syndrome and/or neutropenia increases.
With the simultaneous use of ACE inhibitors and gold preparations (iv sodium aurothiomalate), a symptom complex has been described, including facial flushing, nausea, vomiting and decreased blood pressure.
Sympathomimetics may reduce the antihypertensive effects of captopril.
Insulin and oral hypoglycemic agents increase the risk of hypoglycemia.
Concomitant use of captopril with food or antacids slows down the absorption of captopril in the gastrointestinal tract.
During therapy with captopril, the use of ethanol is not recommended, since ethanol enhances the antihypertensive effect of captopril.
The antihypertensive effect of captopril is weakened by epoetins, estrogens and combined oral contraceptives, carbenoxolone, glucocorticosteroids and naloxone.
Probenecid reduces the renal clearance of captopril and increases its serum concentrations in the blood.
The use of captopril in patients taking immunosuppressants (for example, azathioprine or cyclophosphamide) increases the risk of developing hematological disorders. Captopril increases the concentration of digoxin in the blood plasma by 15-20%.
Increases the bioavailability of propranolol.
Cimetidine, by slowing down metabolism in the liver, increases the concentration of captopril in the blood plasma.
Clonidine reduces the severity of the antihypertensive effect.
The interaction of ACE inhibitors with drugs containing co-trimoxazole [trimethoprim + sulfamethoxazole] causes an increased risk of developing hyperkalemia.
Interaction with dipeptidyl peptidase type IV (DPP-IV) inhibitors (gliptins), for example, sitagliptin, saxagliptin, vildagliptin, linagliptin increases the risk of developing angioedema.
Interaction with racecadotril increases the risk of developing angioedema. Interaction with estramustine increases the risk of developing angioedema.
Overdose
Overdose
Symptoms: pronounced decrease in blood pressure, up to collapse, shock, stupor, bradycardia, water and electrolyte imbalance, acute renal failure, myocardial infarction, acute cerebrovascular accident, thromboembolic complications.
Treatment: gastric lavage, administration of adsorbents and sodium sulfate no later than 30 minutes after taking the drug; transfer the patient to the “lying” position with elevated legs, take measures aimed at restoring blood pressure, replenishing the volume of circulating blood (for example, intravenous administration of 0.9% sodium chloride solution), symptomatic therapy – epinephrine (adrenaline) – subcutaneously or intravenously, antihistamines, hydrocortisone – intravenously. For bradycardia or severe vagal reactions, atropine should be used. Hemodialysis may be used; peritoneal hemodialysis is ineffective.
Storage conditions
Storage conditions
In a place protected from light at a temperature not exceeding 25 ° C. Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after expiration date.
Manufacturer
Manufacturer
Velfarm LLC, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In a light-protected place at a temperature not exceeding 25 oC. Keep out of the reach of children. |
| Manufacturer | Welfarm, Russia |
| Medication form | pills |
| Brand | Welfarm |
Other forms…
Related products
Buy Captopril Welfarm, tablets 50 mg 40 pcs with delivery to USA, UK, Europe and over 120 other countries.