No products in the cart.
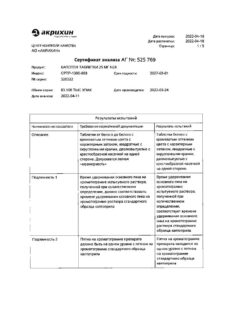
Captopril, tablets 50 mg 20 pcs
€1.68 €1.53
Description
Pharmacotherapeutic group: inhibitor of angiotensin-converting enzyme
ATX code: C09AA01
Pharmacological Properties
Pharmacodynamics
Captopril is an angiotensin-converting enzyme (ACE) inhibitor. It reduces the formation of angiotensin II from angiotensin I. Reduces the concentration of angiotensin II, which leads to a direct reduction in the release of aldosterone. It reduces total peripheral vascular resistance, blood pressure (BP), post- and preload on the heart. Dilates arteries to a greater extent than veins. Causes decreased bradykinin degradation (one of the effects of ACE) and increased prostaglandin synthesis. The antihypertensive effect does not depend on blood plasma renin activity, BP reduction is observed in normal and even reduced activity of the hormone, which is due to the effect on tissue renin-angiotensin-aldosterone system (RAAS). It enhances coronary and renal blood flow. With long-term use it reduces the severity of myocardial hypertrophy and resistive arterial walls. Improves blood supply to ischemic myocardium. Reduces platelet aggregation. Helps reduce sodium ions in patients with heart failure.
The decrease of BP in contrast to direct vasodilators (hydralazine, minoxidil, etc.) is not accompanied by reflex tachycardia and leads to a reduction of myocardial oxygen demand. In heart failure, an adequate dose has no effect on BP. Maximum BP decrease after oral administration is observed in 60-90 minutes. The duration of antihypertensive effect depends on the dose of the drug taken and reaches optimal values within several weeks.
The temporary withdrawal of captopril should not be abrupt, as this may cause a significant increase in BP.
Pharmacokinetics
Absorption is rapid and is about 75% of the dose taken. Food intake reduces bioavailability by 30-40%. Maximum plasma concentration is noted 1 h after oral administration.
Binding to plasma proteins is 25-30%, mainly to albumin. Less than 0.002% of the taken dose of captopril is secreted with breast milk, does not penetrate through the blood-brain barrier.
It is metabolized in the liver with the formation of captopril disulfide dimer and captopril-cysteine sulfide. Metabolites are pharmacologically inactive. The half-life (T1/2) of captopril is about 2-3 h. About 95% is excreted by the kidneys during the first day, of which 40-50% is unchanged, the rest
part – as metabolites. Four hours after a single oral dose, the urine contains about 38% of unchanged captopril and 28% as metabolites, after 6 hours – only as metabolites; in the daily urine – 38% of unchanged captopril and 62% as metabolites.
Cumulates in chronic renal failure. (T1/2) in renal failure is 3.5-32 h, therefore, patients with impaired renal function should reduce the dose of the drug and/or increase the interval between doses.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
Active ingredient: captopril – 50.0 mg.
Auxiliary substances: lactose monohydrate (milk sugar)- 94.0 mg, microcrystalline cellulose – 49.0 mg, corn starch – 5.0 mg, magnesium stearate – 2.0 mg.
How to take, the dosage
How to take, the dosage
Captopril is administered orally one hour before meals. The dosing regimen is determined individually.
In arterial hypertension, the drug is prescribed in an initial dose of 12.5 mg (for this dosing regimen, the drug must be taken in 25 mg tablets with a rice) 2 times daily. Attention should be paid to the tolerability of the first dose within 1 hour. If arterial hypotension developed, the patient should be transferred to the “lying” position with elevated legs (such reaction to the first dose should not be an obstacle to further therapy). If necessary, the dose is gradually (at 2-4 week intervals) increased until an optimal effect is achieved.
In mild to moderate arterial hypertension, the usual maintenance dose is 25 mg twice daily; the maximum dose is 50 mg twice daily. In severe arterial hypertension, the initial dose is 12.5 mg (for this dosing regimen, the drug should be taken in 25 mg tablets with a ricochet) 2 times daily. The dose is gradually increased to a maximum daily dose of 150 mg (50 mg 3 times daily).
In CHF, it is used together with other diuretics and/or in combination with cardiac glycosides (to avoid an initial excessive decrease of BP, the diuretic should be cancelled before the drug is prescribed; a marked decrease of the blood pressure should be excluded).
The initial daily dose is 6.25 mg (for this dosing regimen it is necessary to take the drug in 12.5 mg tablets with a rib or in 25 mg tablets with a cruciform rib) 3 times daily, further, if necessary, the dose is increased gradually (at intervals of at least 2 weeks). The average maintenance dose is 25 mg 2-3 times per day, and the maximum
In left ventricular dysfunction after myocardial infarction in clinically stable patients, Captopril may be started as early as 3 days after myocardial infarction. The initial dose is 6.25 mg per day (for this dosing regimen, the drug should be taken in 12.5 mg tablets with a rib or in 25 mg tablets with a cross-shaped rib), then the daily dose can be increased to 37.5-75 mg in 2-3 doses (depending on tolerance of the drug) up to a maximum dose of 150 mg per day.
In type 1 diabetes mellitus complicated by nephropathy, Captopril is prescribed in a dose of 75-100 mg in 2-3 doses. In type 1 diabetes with microalbuminuria (albumin excretion 30-300 mg/day), the drug dose is 50 mg 2 times a day. In case of proteinuria more than 500 mg/day the drug is effective in a dose of 25 mg 3 times a day.
Patients with impaired renal function should adjust the dose of captopril: the drug dose should be reduced or the intervals between doses should be increased. If necessary, “loop” diuretics rather than thiazide-type diuretics are prescribed additionally.
Recommended dosage adjustment scheme for Captopril in patients with impaired renal function
Glomerular filtration rate (ml/min/1.73 m2)
Initial daily dose (mg)
Maximum daily dose (mg)
25-50
150
21-40
25
100
10-20
12.5
75
<10
6.25
37.5
In the elderly, the drug should be used in an initial dose of 6.25 mg (for this dosing regimen, take the drug in 12.5 mg tablets with a slash or 25 mg tablets with a cross-shaped slash) twice daily, to prevent impaired renal function, and maintain it at this level if possible. The dose of Captopril is recommended to be adjusted continuously depending on the therapeutic response of the patient and maintained at the lowest possible level.
Interaction
Interaction
Concomitant use of captopril and nonsteroidal anti-inflammatory drugs (NSAIDs) may result in decreased antihypertensive effect, especially in hypertension accompanied by low renin activity. In patients with risk factors (elderly patients, patients with hypovolemia, patients taking diuretics, with impaired renal function), simultaneous use of NSAIDs (including cyclooxygenase-2 inhibitors) and ACE inhibitors, including captopril, may lead to worsening of renal function, up to acute renal failure. Usually renal function impairment in such cases is reversible. Renal function should be periodically monitored in patients taking captopril and NSAIDs.
In therapy with captopril, potassium-saving diuretics (e.g., triamterene, amiloride, spironolactone and its derivative, eplerenone), potassium preparations, potassium supplements, salt substitutes (containing large amounts of potassium) should be prescribed only when hypokalemia is proven, because their concomitant use increases the risk of hyperkalemia.
Concomitant use of ACE inhibitors (especially in combination with diuretics) and lithium salts may increase plasma lithium concentration and, consequently, toxicity of lithium preparations. Plasma lithium concentration should be periodically determined.
When prescribing captopril with allopurinol or procainamide increases the risk of neutropenia and/or Stevens-Johnson syndrome.
The use of captopril in patients taking immunosuppressants (e.g., cyclophosphamide or azathioprine) increases the risk of hematological disorders.
Aliskiren
In patients with diabetes mellitus or impaired renal function (FFR less than
60 ml/min/1.73 m2), there is an increased risk of hyperkalemia, impaired renal function, and increased cardiovascular morbidity and mortality (see
Contraindications
).
. The literature has reported that in patients with established atherosclerotic disease, heart failure, or diabetes mellitus with target organ damage, concurrent therapy with an ACE inhibitor and angiotensin II receptor antagonists (ARA II) is associated with higher rates of arterial hypotension, syncope, hyperkalemia, and impaired renal function (including acute renal failure) compared with use of the RAAS-acting drug alone. Dual blockade (e.g., when ACE inhibitor is combined with ARA II) should be limited to individual cases with close monitoring of renal function, potassium, and BP.
Captopril may increase the effect of insulin and hypoglycemic agents administered orally, which may require decreasing the dose of hypoglycemic agents when used concomitantly with captopril.
Captopril may cause a false positive urine test for acetone.
Concomitant use with thiazide diuretics, vasodilators (minoxidil), verapamil, beta-adrenoblockers, tricyclic antidepressants or ethanol increases the antihypertensive effect.
Sympathomimetics may decrease the antihypertensive effect of captopril and ACE inhibitors.
Estramustine
Concomitant use may increase the risk of side effects such as angioedema.
Baclofen
It enhances the antihypertensive effect of ACE inhibitors. BP should be monitored carefully and, if necessary, the captopril dose should be reduced.
Glyptins (linagliptin, saxagliptin, sitagliptin, vildagliptin)
The co-administration of ACE inhibitors may increase the risk of angioedema due to inhibition of dipeptidyl peptidease IV (DPP-IV) activity by glyptin.
Gold preparations
In the use of ACE inhibitors, including captopril, patients receiving intravenous gold (sodium aurothiomalate) have described a symptom complex including facial hyperemia, nausea, vomiting, and hypotension.
Tricyclic antidepressants, antipsychotics (neuroleptics) and agents for general anesthesia
Simultaneous use with ACE inhibitors may lead to increased antihypertensive effect (see section “Special Precautions”).
Special Instructions
Special Instructions
Phypertension and renal function should be monitored before initiating, as well as regularly during treatment with Captopril. In patients with CHF, the drug should be used under close medical supervision.
Hypotension
In patients with arterial hypertension when using captopril, severe arterial hypotension is only rarely seen; the potential for this condition increases with increased fluid and salt loss (e.g., after intensive diuretic treatment), in patients with CHF, or those on dialysis. The possibility of a sharp decrease in BP can be minimized by prior cancellation (4-7 days) of a diuretic or by increasing sodium chloride (table salt) intake (about a week before the beginning of treatment), or by prescription of low doses (6.25-12.5 mg/day) of captopril at the beginning of treatment. When using hypotensive drugs, pronounced BP reduction in patients with cerebrovascular disorders, cardiovascular disease, may increase the risk of myocardial infarction or stroke.
Contraindications
Contraindications
Hypersensitivity to captopril or other ACE inhibitors or any of the excipients of the drug; history of angioedema on ACE inhibitors, hereditary and/or idiopathic angioedema; Severe renal and/or hepatic impairment, bilateral renal artery stenosis, stenosis of a single kidney with progressive azotemia, conditions after renal transplantation, refractory hyperkalemia, pregnancy, breastfeeding, age less than 18 years, Lactose intolerance, lactase deficiency and glucose-galactose malabsorption syndrome, concomitant use with aliskiren and aliskiren-containing drugs in patients with diabetes or impaired renal function (glomerular filtration rate (GFR) < 60 mL/min/1.73 m²) (see Sections
“Special Considerations” for more information. See sections
“Cautions” and “Interaction with other medicinal products”).
WARNING
Use with caution in patients with severe systemic autoimmune diseases (including systemic lupus erythematosus and scleroderma), suppression of medullary hematopoiesis (risk of neutropenia and agranulocytosis), cerebral ischemia, chronic heart failure (CHF), diabetes (increased risk of hyperkalemia), with primary hyperaldosteronism; in patients on hemodialysis, diet with restriction of table salt, coronary heart disease, with conditions accompanied by a decrease in circulating blood volume (CBC) (including vomiting, diarrhea, taking diuretics), with simultaneous use of potassium saving diuretics, potassium preparations, potassium containing salt substitutes and lithium, immunosuppressants, allopurinol, procainamide (risk of neutropenia and agranulocytosis), hyperkalemia, hemodialysis using high-flow membranes (e.g., AN69®), surgery/general anesthesia aortic stenosis/mitral stenosis/hypertrophic obstructive cardiomyopathy, desensitization therapy, low-density lipoprotein (LDL) apheresis, when used in non-human race, elderly patients.
Side effects
Side effects
The frequency of adverse reactions was determined according to World Health Organization recommendations: Very common (â¥1/10); common (â¥1/100, <1/10); infrequent (â¥1/1000, <1/100); rare (â¥1/10000, <1/1000); very rare (<1/10000), including individual reports; unspecified frequency (frequency cannot be calculated from available data).
The blood and lymphatic system: very rare – neutropenia, agranulocytosis, pancytopenia (in patients with renal dysfunction), lymphadenopathy, eosinophilia, thrombocytopenia, anemia (including aplastic, hemolytic), autoimmune diseases.
Metabolism and nutrition disorders: rarely – anorexia, very rarely – hyperkalemia, hypoglycemia.
Psychiatric disorders: often – sleep disorders, very rare – confusion, depression.
Cardiovascular system disorders: infrequent – tachycardia or tachyarrhythmia, palpitations, orthostatic hypotension, angina pectoris, Raynaud’s syndrome, blood flushing to the face, pallor, peripheral edema; very rare – cardiac arrest, cardiogenic shock.
Respiratory system: often – cough (dry unproductive), dyspnea; very rarely – bronchospasm, rhinitis, allergic alveolitis, eosinophilic pneumonia, pulmonary edema.
The central nervous system: often – disorder of taste, dizziness, somnolence, rarely – headache, paresthesia, very rarely – cerebral circulation disorders, including stroke and syncope. Sensory system disorders: very rare – visual acuity disorder.
Digestive system disorders: frequent – dry oral mucosa, nausea, vomiting, abdominal pain, diarrhea, constipation; rare – stomatitis, aphthous stomatitis, gum hyperplasia; very rare – angioedema of the intestine; glossitis, peptic ulcer, pancreatitis, liver dysfunction, cholestasis, jaundice, hepatitis (including rare cases of hepatonecrosis), increased activity of
“hepatic” enzymes.
Skin and subcutaneous tissue disorders: frequently – skin itching with or without rashes, alopecia; infrequently – angioedema; very rarely – urticaria, Stevens-Johnson syndrome, erythema multiforme, photosensitivity, erythroderma, exfoliative dermatitis, pemphigoid reactions.
Muscular system disorders: very rare – myalgia, arthralgia.
Arenal system disorders: rare – renal dysfunction, acute renal failure, increased concentration of urea and creatinine in the blood, polyuria, oliguria, increased frequency of urination, very rare – nephrotic syndrome, sexual dysfunction, gynecomastia.
General disorders and symptoms: infrequent – chest pain, increased fatigue, malaise; very rare – fever.
Laboratory findings: very rare – proteinuria, eosinophilia, hyperkalemia, hyponatremia, hypoglycemia, increased concentration of nitrogen, urea in plasma, acidosis, increased concentration of creatinine and bilirubin in serum, decrease of hemoglobin and hematocrit, decrease of leukocyte number, platelets, increased titer for antinuclear antibodies, increased CRP. When ACE inhibitors, including captopril, were used by patients receiving intravenous gold (sodium aurothiomalate), a symptom complex including facial hyperemia, nausea, vomiting, and arterial hypotension has been described.
Overdose
Overdose
Pregnancy use
Pregnancy use
Pregnancy
Captopril is contraindicated in pregnancy (see section
“Contraindications”).
Captopril should not be used in the first trimester of pregnancy. Appropriate controlled clinical trials of ACE inhibitors in pregnant women have not been conducted. The limited data available on the effects of the drug in the first trimester of pregnancy indicate that the use of ACE inhibitors does not lead to fetotoxicity-related fetal malformations. Epidemiological evidence of the risk of teratogenic effects of ACE inhibitors in the first trimester of pregnancy has not been conclusive, but some increased risk cannot be excluded. If pregnancy is planned or occurs during the use of Captopril, the drug should be discontinued immediately and, if necessary, other hypotensive therapy with a proven safety profile in pregnancy should be prescribed.
It is known that exposure of the fetus to ACE inhibitors in the second and third trimesters of pregnancy may lead to impaired fetal development (reduced renal function, oligohydramnios, delayed ossification of the skull bones) and fetal death as well as the development of complications in the newborn (renal failure, hypotension, hyperkalemia).
Similarities
Similarities
Additional information
| Weight | 0.015 kg |
|---|---|
| Shelf life | 3 years. Do not use after the expiration date. |
| Conditions of storage | Store in a light-protected place at a temperature not exceeding 25 °С. Keep out of reach of children. |
| Manufacturer | Ozon, Russia |
| Medication form | pills |
| Brand | Ozon |
Other forms…
Related products
Buy Captopril, tablets 50 mg 20 pcs with delivery to USA, UK, Europe and over 120 other countries.