No products in the cart.
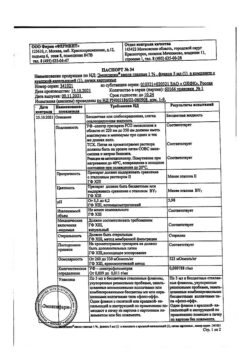
Brinarga, eye drops 1%+0.5% 5 ml
€23.88 €19.90
Description
Pharmacodynamics
Mechanism of action
Brinarga contains two active ingredients: brinzolamide and timolol maleate, which reduce elevated intraocular pressure (IOP) primarily by reducing intraocular fluid secretion, but in different ways. The combined effect of brinzolamide and timolol exceeds the effect of each agent alone to reduce IOP.
Brinzolamide is a carboanhydrase ΙΙ inhibitor. Inhibition of carboanhydrase in the ciliary body of the eyeball reduces intraocular fluid production, presumably by slowing the formation of bicarbonate ions with a consequent reduction in sodium and fluid transport.
Timolol is a non-selective blocker of β-adrenoreceptors without sympathomimetic activity, has no direct depressant effect on the myocardium and has no membrane stabilizing activity. A number of studies have shown that when used topically, timolol decreases intraocular fluid formation and slightly increases its outflow.
Pharmacokinetics
Absorption
When used topically, brinzolamide and timolol penetrate the systemic bloodstream.
The maximum concentration (Cmax) in erythrocytes is about 18.4 µM.
In equilibrium, after administration of brinzolamide and timolol, the mean Cmax of timolol in plasma and the area under the concentration-time curve over 12 hours (AUC0-12h) of timolol was 0.824 ± 0.453 ng/mL and 4.71 ± 4.29ng*h/mL, respectively, and the mean Cmah of timolol was achieved at 0.79 ± 0.45 h.
Distribution
Brinzolamide binds moderately to plasma proteins (about 60%) and accumulates in erythrocytes as a result of selective binding to carboanhydrase II and, to a lesser extent, to carboanhydrase I. Its active metabolite N-dezethylbrinzolamide also accumulates in erythrocytes, where it binds predominantly to carboanhydrase I. Due to the affinity of brinzolamide and its metabolite to erythrocytes and tissue carboanhydrase, their concentration in plasma is low.
Metabolism
The metabolism of brinzolamide occurs by N-dealkylation, O-dealkylation and oxidation of the N-propyl side chain. The main metabolite, N-dezethylbrinzolamide, in the presence of brinzolamide, binds to carboanhydrase I and also accumulates in erythrocytes. In vitro studies have shown that the CYP3A4 isoenzyme, but also the CYP2A6, CYP2B6, CYP2C8 and CYP2C9 isoenzymes are primarily responsible for the metabolism of brinzolamide.
The metabolism of timolol occurs in two ways: with the formation of an ethanol side chain on the thiadiazole ring and with the formation of an ethanol side chain at the morpholine nitrogen and a similar side chain with a carbonyl group coupled to the nitrogen. Thymolol metabolism is carried out mainly by CYP2D6.
Evolution
Brinzolamide is excreted mainly with urine and feces in comparative amounts of 32% and 29%, respectively. About 20% is excreted as metabolites in the urine. Brinzolamide and N-dezethylbrinzolamide as well as residual amounts (<1 %) of other metabolites (N-desmethoxypropyl and O-desmethyl) are found mainly in urine.
Timolol and its metabolites are excreted mainly by the kidneys. About 20% of timolol is excreted unchanged in the urine, the rest as metabolites. T1/2 timolol is 4.8 h after topical combined use of brinzolamide and timolol.
Indications
Indications
Reduction of elevated intraocular pressure in open-angle glaucoma and intraocular hypertension in patients in whom monotherapy was insufficient to reduce intraocular pressure.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Mechanism of action
The drug Brinarga contains two active substances: brinzolamide and timolol maleate, which reduce elevated intraocular pressure (IOP), primarily by reducing the secretion of intraocular fluid, but in different ways. The combined effect of brinzolamide and timolol exceeds the effect of each substance alone in reducing IOP.
Brinzolamide is a carbonic anhydrase ΙΙ inhibitor. Inhibition of carbonic anhydrase in the ciliary body of the eyeball reduces the production of intraocular fluid, presumably due to a slowdown in the formation of bicarbonate ions with a subsequent decrease in sodium and fluid transport.
Timolol is a non-selective β-adrenergic receptor blocker without sympathomimetic activity, does not have a direct depressive effect on the myocardium, and does not have membrane-stabilizing activity. A number of studies have shown that when applied topically, timolol reduces the formation of intraocular fluid and slightly increases its outflow.
Pharmacokinetics
Absorption
When applied topically, brinzolamide and timolol penetrate into the systemic circulation.
The maximum concentration (Cmax) in erythrocytes is about 18.4 µM.
At steady state, after administration of brinzolamide and timolol, the average Cmax of timolol in plasma and the area under the concentration-time curve at 12 hours (AUC0-12h) of timolol was 0.824 ± 0.453 ng/ml and 4.71 ± 4.29 ng*h/ml, respectively, and the average Cmax of timolol was achieved at 0.79 ± 0.45 hours
Distribution
Brinzolamide is moderately bound to plasma proteins (about 60%) and accumulates in erythrocytes as a result of selective binding to carbonic anhydrase II and, to a lesser extent, to carbonic anhydrase I. Its active metabolite N-desethylbrinzolamide also accumulates in erythrocytes, where it binds predominantly to carbonic anhydrase I. Due to the affinity of brinzolamide and its metabolite to erythrocytes and tissue carbonic anhydrase, their concentration in plasma is low.
Metabolism
The metabolism of brinzolamide occurs through N-dealkylation, O-dealkylation and oxidation of the N-propyl side chain. The main metabolite, N-desethylbrinzolamide, in the presence of brinzolamide, binds to carbonic anhydrase I and also accumulates in erythrocytes. In vitro studies have shown that the metabolism of brinzolamide is mainly responsible for the CYP3A4 isoenzyme, as well as the CYP2A6, CYP2B6, CYP2C8 and CYP2C9 isoenzymes.
The metabolism of timolol occurs in two ways: with the formation of an ethanolamine side chain on the thiadiazole ring and with the formation of an ethanol side chain at the morpholine nitrogen and a similar side chain with a carbonyl group connected to the nitrogen. Timolol is metabolized mainly by CYP2D6.
Removal
Brinzolamide is excreted mainly in urine and feces in comparative amounts of 32% and 29%, respectively. About 20% is excreted as metabolites in the urine. The urine contains mainly brinzolamide and N-desethylbrinzolamide, as well as residual amounts (<1%) of other metabolites (N-desmethoxypropyl and O-desmethyl).
Timolol and its metabolites are excreted mainly by the kidneys. About 20% of timolol is excreted unchanged in the urine, the rest – in the form of metabolites. T1/2 of timolol is 4.8 hours after local combined use of brinzolamide and timolol.
Special instructions
Special instructions
Systemic effects
Brinzolamide and timolol may be subject to systemic absorption. Timolol, when applied topically, can cause the same adverse reactions from the cardiovascular and respiratory systems, as well as other undesirable reactions, as systemic beta-blockers.
Hypersensitivity reactions, characteristic of all sulfonamide derivatives, may develop when using the drug Brynarga due to systemic absorption. If serious adverse reactions or hypersensitivity reactions occur, the drug should be discontinued.
Heart disorders
In patients with cardiovascular disease (eg, coronary artery disease, Prinzmetal’s angina, heart failure) and hypotension, beta-blocker therapy should be critically evaluated and treatment with other active agents considered. Patients with cardiovascular disease should be closely monitored for signs of exacerbation of the disease and adverse reactions.
Vascular disorders
Caution should be used in patients with severe impairment/disorder of peripheral circulation (Raynaud’s disease or severe Raynaud’s syndrome).
Hyperthyroidism
β-blockers may mask the symptoms of hyperthyroidism.
Muscle weakness
β-blockers have been reported to increase muscle weakness that occurs with some symptoms of myasthenia gravis (eg, diplopia, ptosis, and general weakness).
Respiratory system disorders
Respiratory reactions, including death from bronchospasm, have been reported in patients with asthma after taking topical beta-blockers.
Hypoglycemia/diabetes
β-blockers should be prescribed with caution to patients with a tendency to spontaneous hypoglycemia or patients suffering from labile diabetes, since these drugs may mask the symptoms of acute hypoglycemia.
Acid-base imbalance
The development of acid-base imbalance with the use of oral forms of carbonic anhydrase inhibitors has been described. In patients at risk of renal failure, the drug should be used with caution due to the possible risk of metabolic acidosis.
Concentration
Oral carbonic anhydrase inhibitors may affect the ability to perform activities requiring increased alertness and/or physical coordination in elderly patients. These phenomena can be observed because brinzolamide penetrates the systemic circulation when applied topically.
Anaphylactic reactions
Patients with atopy or a history of severe anaphylactic reactions to various allergens who are receiving beta-blockers may react more severely to exposure to these allergens and may also be resistant to normal doses of epinephrine for the treatment of anaphylactic reactions.
Choroidal detachment of the eye
Cases of detachment of the choroid have been described when using drugs that prevent the formation of intraocular fluid (for example, timolol, acetazolamide) after filtering operations.
Surgical anesthesia
The action of β-blockers in ophthalmic drugs can block the systemic action of β-agonists, for example, epinephrine. The anesthesiologist should be informed that the patient is taking timolol.
Concomitant therapy
When using the drug Brynarga in patients taking systemic beta-blockers, it is necessary to take into account the possible mutual enhancement of the pharmacological action of the drugs, both in relation to the known systemic effects of beta-blockers and in relation to the reduction of intraocular pressure.
Careful monitoring of such patients is necessary.
The combined use of two local β-blockers is not recommended. There is a potential for increased systemic effects resulting from carbonic anhydrase inhibition in patients taking oral carbonic anhydrase inhibitors and Brynarga. The simultaneous administration of Brynarga and oral carbonic anhydrase inhibitors is not recommended.
Effects on the organ of vision
The effect of brinzolamide on corneal endothelial function in patients with corneal disorders (especially patients with low endothelial cell counts) has not been studied. Contact lens wearers should be closely monitored for corneal health while using brinzolamide as carbonic anhydrase inhibitors may affect corneal hydration. Close monitoring of patients with corneal disorders, such as patients with diabetes mellitus or corneal dystrophy, is recommended.
Benzalkonium chloride
Benzalkonium chloride, which is part of the drug Brinarga, can cause eye irritation and also change the color of soft contact lenses. Contact with soft contact lenses should be avoided.
Before using the drug, contact lenses should be removed and put back no earlier than 15 minutes after using the drug.
Brynarga contains benzalkonium chloride, which may cause punctate keratopathy and/or toxic ulcerative keratopathy. With long-term use of the drug, patients should be carefully monitored.
Liver dysfunction
Brynarga should be used with caution in patients with severe hepatic impairment.
Impact on the ability to drive vehicles and machinery
Brynarga has a slight effect on the ability to drive and operate machinery.
If the patient experiences temporary blurred vision after using the drug, it is not recommended to drive a car or engage in activities that require increased attention and reaction until it recovers.
Carbonic anhydrase inhibitors may impair the ability to perform tasks requiring concentration and/or coordination.
Active ingredient
Active ingredient
Brinzolamide, Timolol
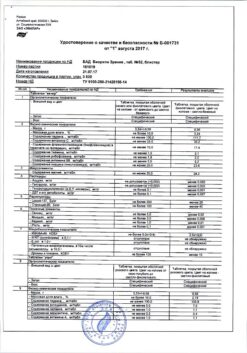
Composition
Composition
Active ingredients
Brinzolamide 10 mg,
Timolol maleate 6.83 mg, equivalent to timolol 5 mg.
Excipients:
Benzalkonium chloride 0.1 mg; disodium edetate 0.1 mg; sodium chloride 1.0 mg; tyloxapol 0.25 mg; mannitol 33 mg; carbomer 974P 4.2 mg; sodium hydroxide and/or hydrochloric acid to pH 7.3; water for injections up to 1.0 ml.
Pregnancy
Pregnancy
Brinarga is contraindicated for use during pregnancy and breastfeeding.
Contraindications
Contraindications
Individual hypersensitivity to the components of the drug, sulfonamides or other β-blockers.
Reactive respiratory diseases, incl. bronchial asthma (BA), history of BA, severe chronic obstructive pulmonary diseases. Sinus bradycardia, sick sinus syndrome, sinoatrial block, atrioventricular (AV) block II-III degree, severe heart failure or cardiogenic shock.
Severe allergic rhinitis.
Hyperchloremic acidosis. Severe renal failure.
Pregnancy, breastfeeding, children under 18 years of age.
Side Effects
Side Effects
Security Profile Overview
The most commonly reported adverse reactions in clinical studies were blurred vision, eye irritation, and eye pain, which occurred in approximately 2-7% of patients.
Below are the adverse reactions noted during clinical studies of Brynarga and its individual components – brinzolamide and timolol.
Adverse reactions are listed using the following frequency designations: very common (>1/10), common (>1/100 to 1/1000 to 1/10000 to <1/1000), very rare (<1/10000) and frequency unknown (cannot be estimated from available data). Within each frequency category, adverse reactions are listed in order of decreasing severity.
Infectious and parasitic diseases Frequency unknown: nasopharyngitis3, pharyngitis3, sinusitis3, rhinitis3
Blood and lymphatic system disorders Frequency unknown: decreased red blood cell count3, increased blood chloride3
Immune system disorders Frequency unknown: anaphylaxis2, systemic lupus erythematosus2, systemic allergic reactions, including angioedema2, local and generalized rash2, hypersensitivity1, urticaria2, itching2.
Metabolic and nutritional disorders Frequency unknown: hypoglycemia2, decreased appetite3
Mental disorders Uncommon: insomnia1
Frequency unknown: depression1, memory loss2, apathy3, depressed mood3, decreased libido3, nightmares2,3, nervousness3.
Nervous system disorders Common: dysgeusia1
Frequency unknown: cerebral ischemia2, cerebrovascular accident2, syncope2, increased signs and symptoms of myasthenia gravis2, somnolence3, motor dysfunction3, amnesia3, memory impairment3, paresthesia2,3, tremor3, hypoesthesia3, ageusia3, dizziness1,2, headache1
Eye disorders Common: blurred vision1, eye pain1, eye irritation1
Uncommon: corneal erosion1, punctate keratitis1, anterior chamber effusion1, photophobia1, dry eye syndrome1, eye discharge1, itching in the eye1,3, foreign body sensation in the eyes1, ocular hyperemia1, scleral hyperemia1, increased lacrimation1, conjunctival hyperemia1, eyelid erythema1
Frequency unknown: increased optic disc excavation3, choroidal detachment after filtering surgery2, keratitis2,3, keratopathy3, corneal epithelial defect3, disruption of the corneal epithelium3, increased IOP3, deposits in the eye3, corneal staining3, corneal edema3, decreased corneal sensitivity2, conjunctivitis3, inflammation of the meibomian glands3, diplopia2,3, decreased visual contrast3, photopsia3, decreased visual acuity2,3, visual impairment1, pterygium3, discomfort in the eye3, dry keratoconjunctivitis3, eye hypoesthesia3, scleral pigmentation3, subconjunctival cyst3, visual impairment3, swelling of the eyes3, allergic reactions of the eye3, madarosis3, eyelid disorders3, eyelid edema1, ptosis2, blepharitis3, asthenopia3, formation of crusts on the edges of the eyelids3, increased lacrimation3
Hearing and labyrinthine disorders Frequency unknown: vertigo3, tinnitus3
Cardiac disorders Frequency not known: cardiac arrest2, heart failure2, chronic heart failure2, AV block2, cardiorespiratory distress syndrome3, angina3, bradycardia2,3, irregular heart rate3, arrhythmia2,3, palpitations2,3, tachycardia3, increased heart rate3, pain in breast2, swelling2
Vascular disorders Uncommon: decreased blood pressure1
Not known: hypotension2, hypertension3, increased blood pressure1, Raynaud’s phenomenon2, cold hands and feet2
Respiratory, thoracic and mediastinal disorders Uncommon: cough1
Frequency unknown: bronchospasm2 (mainly in patients with a history of bronchospastic disease), shortness of breath1, asthma3, epistaxis1, bronchial hyperresponsiveness3, laryngeal irritation3, nasal congestion3, upper respiratory tract congestion3, postnasal drip3, sneezing3, nasal dryness3, pharyngolaryngitis pain3, rhinorrhea3
Gastrointestinal (GIT) disorders Frequency unknown: vomiting2,3, upper abdominal pain1,3, abdominal pain2, diarrhea1,3, dry mouth1, nausea1,3, esophagitis3, dyspepsia2,3, abdominal discomfort3, stomach discomfort3, increased peristalsis3, gastrointestinal disorder3, hypoesthesia and paresthesia of the oral cavity3, flatulence3
Liver and biliary disorders Frequency unknown: abnormal liver function tests3
Skin and subcutaneous tissue disorders Frequency unknown: urticaria3, maculopapular rash2,3, generalized pruritus3, skin induration3, dermatitis3, alopecia1, psoriasiform rash or exacerbation of psoriasis2, rash1, erythema1,3
Musculoskeletal and connective tissue disorders Not known: myalgia1, muscle cramps3, arthralgia3, back pain3, limb pain3
Renal and urinary tract disorders Frequency unknown: pain in the kidney area3, pollakiuria3
Genital and breast disorders Frequency unknown: erectile dysfunction3, sexual dysfunction2, decreased libido2
General and administration site conditions Not known: chest pain1, pain3, fatigue1,2, asthenia2,3, malaise3, chest discomfort3, abnormal sensations3, anxiety3, irritability3, peripheral edema3, drug residue3
Laboratory and instrumental
data Frequency unknown: increased blood potassium1, increased blood lactate dehydrogenase1
1 Adverse reactions observed when using the combination of brinzolamide + timolol.
2 Adverse reactions observed with timolol monotherapy.
3 Adverse reactions observed with brinzolamide monotherapy.
Description of selected adverse reactions
Dysgeusia (bitter or unusual taste in the mouth after instillation) is a commonly reported systemic adverse reaction associated with the use of Brynarga during clinical trials. This is probably related to brinzolamide and is caused by the penetration of eye drops into the nasopharynx through the lacrimal duct. Occlusion of the tear ducts or gentle closure of the eyelids after instillation may help reduce this effect (see Dosage and Administration).
Brinarga contains brinzolamide, which is a carbonic anhydrase inhibitor and has systemic absorption. Effects arising from the gastrointestinal tract, nervous system, blood and lymphatic system, kidneys and urinary tract, metabolism and nutrition are mainly associated with the systemic action of carbonic anhydrase inhibitors. Similar adverse reactions characteristic of oral forms of carbonic anhydrase inhibitors can also be observed when they are used topically.
When applied topically, timolol enters the systemic circulation, which can cause undesirable reactions similar to those that occur with systemic administration of beta-blockers. The listed adverse reactions include reactions that occur with the use of other β-blockers in the form of eye drops. Additional adverse reactions associated with the use of individual active ingredients that may potentially occur with the use of Brynarga are described above. The incidence of systemic adverse reactions with topical administration is lower than with systemic administration. For information about decreased systemic absorption, see section “Dosage and Administration.”
Interaction
Interaction
Brynarga contains brinzolamide, a carbonic anhydrase inhibitor, which when applied topically can be absorbed systemically. Cases of acid-base imbalance resulting from the use of oral carbonic anhydrase inhibitors have been described. The possibility of such disorders should also be taken into account in patients using the drug Brinarga.
Concomitant use with oral carbonic anhydrase inhibitors is not recommended, as there is a possibility of increased systemic adverse reactions. The cytochrome P-450 isoenzymes responsible for the metabolism of brinzolamide are: CYP3A4 (mainly), CYP2A6, CYP2B6, CYP2C8 and CYP2C9. Caution should be exercised when prescribing drugs that inhibit the CYP3A4 isoenzyme, such as ketoconazole, itraconazole, clotrimazole, ritonavir and troleandomycin, due to the possible inhibition of the metabolism of brinzolamide by the CYP3A4 isoenzyme. Caution should be exercised when co-prescribing inhibitors of the CYP3A4 isoenzyme. However, accumulation of brinzolamide is unlikely since it is excreted by the kidneys. Brinzolamide is not an inhibitor of cytochrome P-450 isoenzymes.
Increased systemic action of β-blockers (decreased heart rate, depression) can develop with simultaneous use of CYP2D6 inhibitors (quinidine, fluoxetine, paroxetine) and timolol.
There is a potential for increased hypotensive effects and/or the development of severe bradycardia when topical beta-blockers are used concomitantly with oral calcium channel blockers, guanethidine, beta-blockers, antiarrhythmic drugs (including amiodarone), digitalis glycosides and parasympathomimetics.
β-blockers may reduce the response to epinephrine when treating anaphylactic reactions. The drug should be prescribed with caution to patients with atopy or a history of anaphylaxis (see section “Special Instructions”).
In some cases, as a result of the simultaneous use of topical β-blockers and adrenaline (epinephrine), mydriasis may develop.
The effect on intraocular pressure or the known effects of systemic beta-blockers may be enhanced if timolol is administered to a patient already receiving a systemic beta-blocker. Such patients must be carefully monitored.
The use of two local beta-blockers is not recommended.
When used with other local ophthalmic drugs, the interval between their use should be at least 5 minutes.
Overdose
Overdose
Symptoms
Symptoms of beta-blocker overdose may occur in case of accidental ingestion of the drug: bradycardia, hypotension, heart failure and bronchospasm.
As a result of the action of brinzolamide, electrolyte imbalance, development of acidosis, and disorders of the central nervous system may occur.
Treatment
Symptomatic and supportive therapy. It is necessary to monitor the level of electrolytes in the blood serum (in particular, the content of potassium) and blood pH. Studies have shown that timolol hemodialysis is ineffective.
Storage conditions
Storage conditions
At temperatures from 4 to 30 °C. Keep out of the reach of children.
Shelf life
Shelf life
2 years.
4 weeks after opening.
Do not use after expiration date.
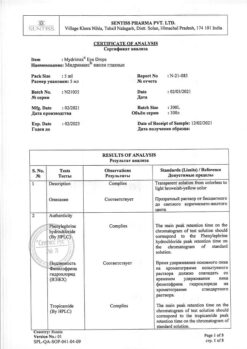
Manufacturer
Manufacturer
Sentiss Pharma Pvt.Ltd, India
Additional information
| Shelf life | 2 years. 4 weeks after opening. Do not use after the expiration date. |
|---|---|
| Conditions of storage | At the temperature from 4 to 30 ° C. Keep out of reach of children. |
| Manufacturer | Sentiss Pharma Pvt.Ltd, India |
| Medication form | eye drops |
| Brand | Sentiss Pharma Pvt.Ltd |
Related products
Buy Brinarga, eye drops 1%+0.5% 5 ml with delivery to USA, UK, Europe and over 120 other countries.