No products in the cart.
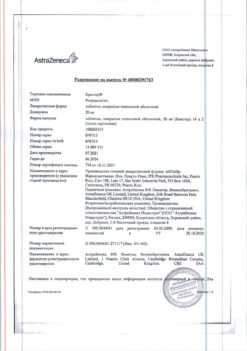
Biprol, 10 mg 30 pcs
€5.93 €5.19
Description
A selective beta1-adrenoblocker with no sympathomimetic activity of its own, has no membrane stabilizing effect.
It has antihypertensive, antiarrhythmic and antianginal action.
By blocking in low doses beta1-adrenoreceptors of the heart it decreases stimulated by catecholamines formation of cyclic adenosine monophosphate from adenosine triphosphate, decreases intracellular ions flux.br>
calcium, has negative chrono-, dromo-, batmo- and inotropic effects, reduces atrioventricular (AV) conduction and excitability.
In case of therapeutic dose it has beta2-adrenoblocking action.
The total peripheral vascular resistance at the beginning of the drug administration (during the first 24 hours) increases (as a result of reciprocal increase of activity of alpha-adrenoreceptors and elimination of
stimulation of beta2-adrenoreceptors) that after 1-3 days returns to the initial level, and decreases after the long-term administration.
Antihypertensive effect is associated with a decrease in the minute blood volume, sympathetic stimulation of peripheral vessels, reduction of the activity of the renin-angiotensin-aldosterone system (has great
important for patients with initial renin hypersecretion), restoration of aortic arch baroreceptors sensitivity (there is no increase of their activity in response to a decrease in blood pressure) and the effect on the central nervous system.
In case of arterial hypertension the effect is developed in 2-5 days, its stable effect – in 1-2 months.
Antianginal action is determined by the decrease of myocardial oxygen demand due to slow heart rate and decreased myocardial contractility, prolongation of diastole, improvement of myocardial perfusion.
By increasing end diastolic pressure in the left ventricle and increasing ventricular muscle fiber stretch may increase myocardial oxygen demand, especially in patients with chronic heart failure (CHF).
Antiarrhythmic action is due to the elimination of arrhythmogenic factors (tachycardia, increased sympathetic nervous system activity, increased cyclic adenosine monophosphate,
arterial hypertension), decreased rate of spontaneous excitation of sinus and ectopic pacemakers, and deceleration of AV conduction (predominantly antegrade and, to a lesser extent, retrograde) through the atrioventricular node and along accessory pathways.
In contrast to non-selective beta-adrenoblockers, when administered in medium therapeutic doses it has less pronounced effect on organs containing beta2-adrenoreceptors (pancreas, skeletalbr>
muscles, smooth muscles of peripheral arteries, bronchi and uterus) and carbohydrate metabolism; does not cause sodium ion retention in the body.
Pharmacokinetics
Absorption. Absorption is 80-90%, food intake does not affect absorption of the drug. Maximal concentration in blood plasma is observed after 1-3 hours. Bioavailability is about 90%. Binding with blood plasma proteins is about 30%.
Distribution. Volume of distribution is 3.5 l/kg. Permeability through the blood-brain barrier and the placental barrier is low.
Metabolism. Metabolized in liver with participation of CYP3A4 (up to 95%) and CYP2D6 isoenzymes. The effect of “primary passage” through the liver is insignificant (about 10%). Biotransformation of bisoprolol is not accelerated in patients with thyroid hyperfunction.
Excretion. Total clearance is 15.6±3.2 l/hour, renal clearance is 9.6±1.6 l/hour. Balanced clearance of bisoprolol is determined by the balance between its excretion through the kidneys in unchanged form (about
50%) and oxidation in the liver (about 50%) to inactive metabolites, which are then also excreted by the kidneys; less than 2% is excreted through the intestine (with bile).
It does not accumulate in the body. Half-life period is 9-12 hours.
Dependence of bisoprolol pharmacokinetics on dose is linear.
Pharmacokinetics of bisoprolol is stable, independent of patient age and sex.
Pharmacokinetics in special clinical cases
Renal insufficiency. In case of marked renal function impairment (creatinine clearance less than 20 ml/min) and in patients with anuria half-life period may increase more than 2 times.
Hepatic insufficiency. In case of severe hepatic insufficiency half-life period is increased up to 13-15 hours.
Chronic heart failure. In patients with chronic heart failure (functional class III according to the NYHA classification), plasma concentration of bisoprolol is higher than in healthy volunteers, and the half-life is increased up to 17 hours.
Indications
Indications
Arterial hypertension.
Coronary heart disease: prevention of attacks of stable angina.
Pharmacological effect
Pharmacological effect
A selective beta1-blocker, without its own sympathomimetic activity, does not have a membrane-stabilizing effect.
Has antihypertensive, antiarrhythmic and antianginal effects.
By blocking beta1-adrenergic receptors of the heart in low doses, it reduces the formation of cyclic adenosine monophosphate from adenosine triphosphate, stimulated by catecholamines, and reduces the intracellular ion current
calcium, has a negative chrono-, dromo-, bathmo- and inotropic effect, reduces atrioventricular (AV) conductivity and excitability.
When the therapeutic dose is exceeded, it has a beta2-adrenergic blocking effect.
The total peripheral vascular resistance at the beginning of drug use (in the first 24 hours) increases (as a result of a reciprocal increase in the activity of alpha-adrenergic receptors and the elimination of
stimulation of beta2-adrenergic receptors), which after 1-3 days returns to the original level, and with long-term administration decreases.
The antihypertensive effect is associated with a decrease in minute blood volume, sympathetic stimulation of peripheral vessels, and a decrease in the activity of the renin-angiotensin-aldosterone system (has a large
significance for patients with initial hypersecretion of renin), restoration of the sensitivity of the baroreceptors of the aortic arch (there is no increase in their activity in response to a decrease in blood pressure) and an effect on the central nervous system.
In case of arterial hypertension, the effect develops after 2-5 days, stable effect – after 1-2 months.
The antianginal effect is due to a decrease in myocardial oxygen demand as a result of a decrease in heart rate and decreased myocardial contractility, prolongation of diastole, and improved myocardial perfusion.
By increasing end-diastolic pressure in the left ventricle and increasing the stretch of ventricular muscle fibers, it can increase myocardial oxygen demand, especially in patients with chronic heart failure (CHF).
The antiarrhythmic effect is due to the elimination of arrhythmogenic factors (tachycardia, increased activity of the sympathetic nervous system, increased content of cyclic adenosine monophosphate,
arterial hypertension), a decrease in the rate of spontaneous excitation of sinus and ectopic pacemakers and a slowdown in AV conduction (mainly in the antegrade and, to a lesser extent, in the retrograde directions) through the atrioventricular node and along additional pathways.
When used in average therapeutic doses, in contrast to non-selective beta-blockers, it has a less pronounced effect on organs containing beta2-adrenergic receptors (pancreas, skeletal
muscles, smooth muscles of peripheral arteries, bronchi and uterus) and carbohydrate metabolism; does not cause sodium ion retention in the body.
Pharmacokinetics
Suction. Absorption is 80-90%, food intake does not affect the absorption of the drug. The maximum concentration in blood plasma is observed after 1-3 hours. Bioavailability – about 90%. Bonding with blood plasma proteins is about 30%.
Distribution. The volume of distribution is 3.5 l/kg. Permeability through the blood-brain and placental barriers is low.
Metabolism. Metabolized in the liver with the participation of isoenzymes CYP3A4 (up to 95%) and CYP2D6. The first pass effect through the liver is insignificant (about 10%). The biotransformation of bisoprolol is not accelerated in patients with hyperthyroidism.
Excretion. Total clearance is 15.6±3.2 l/hour, renal clearance is 9.6±1.6 l/hour. The balanced clearance of bisoprolol is determined by the balance between its excretion through the kidneys unchanged (about
50%) and oxidation in the liver (about 50%) to inactive metabolites, which are then also excreted by the kidneys; less than 2% is excreted through the intestines (with bile).
Does not accumulate in the body. Half-life 9-12 hours.
The dependence of the pharmacokinetics of bisoprolol on dose is linear.
The pharmacokinetics of bisoprolol is stable and does not depend on the age and gender of the patient.
Pharmacokinetics in special clinical situations
Kidney failure. In cases of severe renal impairment (creatinine clearance less than 20 ml/min) and in patients with anuria, the half-life may increase by more than 2 times.
Liver failure. In case of severe liver failure, an increase in the half-life to 13-15 hours is observed.
Chronic heart failure. In patients with chronic heart failure (functional class III according to the NYHA classification), the concentration of bisoprolol in the blood plasma is higher than in healthy volunteers, and the half-life increases to 17 hours.
Special instructions
Special instructions
Treatment with the drug is usually long-term.
Before starting treatment, it is recommended to conduct a study of external respiratory function in patients with a burdened bronchopulmonary history.
Patients with bronchospastic diseases can be prescribed bisoprolol in case of intolerance and/or ineffectiveness of other antihypertensive drugs, and the dose of the drug should be strictly monitored. An overdose is dangerous due to the development of bronchospasm.
Monitoring of patients taking bisoprolol should include monitoring heart rate, blood pressure (at the beginning of treatment – daily, then once every 3-4 months),
electrocardiograms, plasma glucose concentrations in patients with diabetes mellitus (once every 4-5 months).
In elderly patients, it is recommended to monitor renal function (once every 4-5 months). The patient should be trained in the method of counting heart rate and instructed about the need for medical consultation if it decreases below 60 beats/min.
In approximately 20% of patients with angina, beta blockers are ineffective.
The main causes are severe coronary atherosclerosis with a low ischemic threshold (heart rate less than 100 beats/min) and an increase in left ventricular end-diastolic volume, impairing subendocardial blood flow.
In smokers, the effectiveness of beta-blockers is lower.
Patients who use contact lenses should take into account that during treatment there may be a decrease in tear production.
When used in patients with pheochromocytoma, there is a risk of developing paradoxical arterial hypertension (unless effective alpha-blockade has been previously achieved).
In thyrotoxicosis, bisoprolol may mask certain clinical signs of thyrotoxicosis (for example, tachycardia). Abrupt withdrawal in patients with thyrotoxicosis is contraindicated as it can increase symptoms.
In diabetes mellitus, it can mask tachycardia caused by hypoglycemia. Unlike non-selective beta-blockers, it practically does not enhance insulin-induced hypoglycemia and does not delay the restoration of blood glucose concentrations to normal levels.
If clonidine is used simultaneously, it can be discontinued only a few days after bisoprolol is discontinued.
It is possible that the severity of the hypersensitivity reaction may increase and the absence of effect from usual doses of epinephrine against the background of a burdened allergic history.
If planned surgical intervention is necessary, the drug should be discontinued 48 hours before the start of general anesthesia.
If the patient took the drug before surgery, he should choose a drug for general anesthesia with minimal negative inotropic effects.
Reciprocal activation of the vagus nerve can be eliminated by intravenous atropine (1-2 mg).
Drugs that reduce catecholamine levels (for example, reserpine) may enhance the effect of beta-blockers, so patients taking such combinations of drugs should be closely monitored by a physician for hypotension or bradycardia.
If elderly patients develop increasing bradycardia (less than 60 beats/min), arterial hypotension (systolic blood pressure below 100 mm Hg), AV block, bronchospasm, ventricular arrhythmias, severe liver and kidney dysfunction, it is necessary to reduce the dose or stop treatment.
Treatment with bisoprolol should not be abruptly interrupted due to the risk of developing severe arrhythmias and myocardial infarction. Cancellation is carried out gradually, reducing the dose over 2 weeks or more (the dose is reduced by 25% in 3-4 days).
It is recommended to discontinue therapy (with a gradual dose reduction) if depression caused by taking the drug develops.
The drug should be discontinued before testing the content of catecholamines, normetanephrine and vanillinmandelic acid in the blood and urine, and the titer of antinuclear antibodies.
Impact on the ability to drive vehicles and operate machinery
During the treatment period, care must be taken when driving vehicles and performing other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Bisoprolol
Composition
Composition
Active ingredient:
Bisoprolol fumarate 5,000 mg/10,000 mg;
Excipients:
Microcrystalline cellulose 44,500 mg / 62,400 mg;
Ludipress LCE (lactose monohydrate 94.7-98.3%, povidone 3-4%) 40,000 mg / 38,500 mg;
Corn starch 8,000 mg / 11,000 mg;
Colloidal silicon dioxide 0.500 mg/0.600 mg;
Crospovidone (Kollidon CL) 1,000 mg/1,250 mg;
Magnesium stearate 1,000 mg / 1,250 mg;
Shell:
Titanium dioxide 0.287 mg/0.430 mg;
Macrogol (polyethylene glycol 4000) 0.287 mg / 0.430 mg;
Hypromellose 1.320 mg / 1.968 mg;
Talc 0.106 mg/0.172 mg.
Pregnancy
Pregnancy
The use of Biprol during pregnancy and lactation is possible if the benefit to the mother outweighs the risk of side effects in the fetus and child.
Contraindications
Contraindications
Hypersensitivity to bisoprolol, other components of the drug and other beta-blockers; shock (including cardiogenic); pulmonary edema; acute heart failure or CHF in the stage of decompensation, requiring inotropic therapy; AV block II-III degree, without pacemaker;
sinoatrial block; sick sinus syndrome; bradycardia (heart rate less than 60 beats/min); Prinzmetal’s angina; cardiomegaly (without signs of heart failure);
severe arterial hypotension (systolic blood pressure less than 100 mm Hg), especially with myocardial infarction; history of severe bronchial asthma and chronic obstructive pulmonary disease (COPD); simultaneous
taking floctafenine, sultopride, monoamine oxidase inhibitors (MAO), with the exception of MAO type B; simultaneous intravenous administration of verapamil or diltiazem; severe disorders of peripheral
blood circulation, Raynaud’s syndrome; pheochromocytoma (without simultaneous use of alpha-blockers); metabolic acidosis; age up to 18 years (efficacy and safety have not been established).
Lactase deficiency, lactose intolerance, lactose/isomaltose malabsorption syndrome (the drug contains lactose).
With caution
Severe liver failure, severe renal failure (creatinine clearance less than 20 ml/min), myasthenia gravis, thyrotoxicosis, diabetes mellitus (may mask symptoms of hypoglycemia), aggravated
allergic history, first degree AV block, depression (including a history), psoriasis, bronchial asthma, COPD, peripheral circulatory disorders, strict diet.
Side Effects
Side Effects
The frequency of the following side effects is indicated in accordance with the WHO classification: very often – more than 10%; often – more than 1% and less than 10%; infrequently – more than 0.1% or less
1%; rarely – more than 0.01% and less than 0.1%; very rare – less than 0.01%, including isolated cases.
From the central and peripheral nervous system:
often – increased fatigue, asthenia, dizziness, headache. Typically, these phenomena develop at the beginning of treatment, are usually mild and disappear within 1-2 weeks; uncommon – sleep disturbances, depression; rarely – nightmares, hallucinations, loss of consciousness.
From the cardiovascular system:
very often – bradycardia, palpitations; often – a pronounced decrease in blood pressure (especially in patients with CHF), manifestations of vasospasm (increased peripheral circulatory disorders,
feeling of coldness in the extremities (paresthesia); infrequently – impaired AV conduction (up to the development of complete transverse block and cardiac arrest), arrhythmias, aggravation of CHF with the development of peripheral edema (swelling of the ankles, feet) and shortness of breath, orthostatic hypotension, chest pain.
From the digestive system:
often – nausea, vomiting, diarrhea, abdominal pain, constipation, dry oral mucosa; rarely – hepatitis, increased activity of “liver” transaminases (alanine aminotransferase, aspartate aminotransferase), increased bilirubin concentration.
From the respiratory system:
infrequently – laryngo- and bronchospasm in patients with bronchial asthma or obstructive airway diseases; rarely – allergic rhinitis, nasal congestion.
From the musculoskeletal system:
uncommon – muscle weakness, cramps in the calf muscles, arthralgia.
From the senses:
rarely – visual impairment, decreased tear production (should be taken into account when wearing contact lenses), hearing impairment, change in taste;
very rarely – dry and sore eyes, conjunctivitis.
From the skin:
rarely – increased sweating, psoriasis-like skin reactions; very rarely – alopecia, exacerbation of psoriasis.
From the endocrine system:
rarely – hypoglycemia.
From the genitourinary system:
rarely – impaired potency, weakened libido.
From the immune system:
rarely – the appearance of antinuclear antibodies with unusual clinical symptoms of lupus-like syndrome, which disappear after treatment.
Allergic reactions:
rarely – skin hyperemia, skin itching, skin rash, urticaria.
Laboratory indicators:
rarely – hypertriglyceridemia; very rarely – thrombocytopenia, agranulocytosis, leukopenia.
Other:
rarely – withdrawal syndrome (increased angina attacks, increased blood pressure).
Interaction
Interaction
Floctafenine. In case of shock or arterial hypotension caused by floctafenine, beta-blockers cause a decrease in compensatory cardiovascular reactions (joint use is contraindicated).
Sultopride. Due to the additive effect, the development of severe bradycardia is possible (joint use is contraindicated).
MAO inhibitors. Concomitant use is not recommended (with the exception of MAO type B), since there is a high probability of a significant increase in the antihypertensive effect.
The break in treatment between taking MAO inhibitors and bisoprolol should be at least 14 days.
Blockers of “slow” calcium channels (diltiazem and verapamil). This combination should be avoided.
During treatment with Biprol, intravenous administration of verapamil or diltiazem and other antiarrhythmic drugs is contraindicated.
Due to the synergy of action, a sharp decrease in blood pressure, disturbances in automaticity (severe bradycardia, sinus node arrest), disturbances in AV conduction, and heart failure are possible.
If it is necessary to prescribe such a combination, careful clinical and electrocardiographic monitoring of patients is required, especially in the elderly and at the beginning of treatment.
Class I antiarrhythmic drugs (for example, quinidine, disopyramide, lidocaine, phenytoin; flecainide, propafenone), when used simultaneously, may reduce AV conductivity and myocardial contractility (combination with bisoprolol should be avoided).
Class III antiarrhythmic drugs (for example, amiodarone). When used together with bisoprolol, contractility, automaticity and conduction may be impaired due to inhibition of sympathetic compensatory mechanisms (this combination should be avoided).
Centrally acting antihypertensive drugs (clonidine, apraclonidine, alpha-methyldopa, guanfancin, moxonidine, rilmenidine).
When used together, there is an increased risk of developing severe bradycardia, sinus node arrest, AV conduction disturbances, a sharp decrease in blood pressure, and heart failure (synergistic effect).
This combination should be avoided. If use is necessary, careful clinical and electrocardiographic monitoring is required, especially in elderly patients and at the beginning of treatment.
Significant increase in blood pressure upon abrupt discontinuation of a centrally acting antihypertensive drug.
Cardiac glycosides. Decreased heart rate, conduction disturbances.
Topical beta-blockers (for example, eye drops for the treatment of glaucoma) may enhance the systemic effects of bisoprolol (lowering blood pressure, lowering heart rate).
Calcium channel blockers (eg, nifedipine). Possible excessive decrease in blood pressure.
Parasympathomimetics. When used together, there is a risk of developing bradycardia.
Mefloquine. Combined use with bisoprolol increases the risk of bradycardia (additive effect).
Phenytoin for intravenous administration, drugs for inhalation general anesthesia
(hydrocarbon derivatives) increase the severity of the cardiodepressive effect and the likelihood of lowering blood pressure.
Concomitant use with beta-agonists (for example, isoprenaline, dobutamine) may lead to a decrease in the effect of both drugs.
The combination of bisoprolol with adrenergic agonists that affect beta and alpha adrenergic receptors (for example, norepinephrine, epinephrine) may enhance the vasoconstrictor effect of these drugs that occurs with the participation of alpha adrenergic receptors, leading to an increase in blood pressure.
Such interactions are more likely when using non-selective beta-blockers.
Bisoprolol can alter the effectiveness of insulin and oral hypoglycemic agents and mask the symptoms of developing hypoglycemia (tachycardia, increased blood pressure).
Bisoprolol reduces the clearance of lidocaine and xanthines (except diphylline) and increases their concentration in plasma, especially in patients with initially increased clearance of theophylline under the influence of smoking.
The antihypertensive effect is weakened by non-steroidal anti-inflammatory drugs (sodium ion retention and blockade of prostaglandin synthesis by the kidneys), glucocorticosteroids and estrogens (sodium ion retention).
Diuretics, sympatholytics, hydralazine and other antihypertensive drugs. Risk of excessive reduction in blood pressure.
Bisoprolol prolongs the action of non-depolarizing muscle relaxants and the anticoagulant effect of coumarins.
Tri- and tetracyclic antidepressants, antipsychotic drugs (neuroleptics), ethanol, sedatives and hypnotics – when used together with bisoprolol, increased depression of the central nervous system.
Non-hydrogenated ergot alkaloids increase the risk of developing peripheral circulatory disorders.
Ergotamine increases the risk of developing peripheral circulatory disorders.
Sulfasalazine increases the plasma concentration of bisoprolol.
Rifampicin reduces the half-life of bisoprolol.
Allergens used for immunotherapy or allergen extracts for skin testing increase the risk of severe systemic allergic reactions or anaphylaxis in patients receiving bisoprolol.
Iodine-containing radiopaque diagnostic agents for intravenous administration increase the risk of developing anaphylactic reactions.
Overdose
Overdose
Symptoms:
arrhythmia, ventricular extrasystole, severe bradycardia, AV block, marked decrease in blood pressure, acute heart failure, hypoglycemia, acrocyanosis, difficulty breathing, bronchospasm, dizziness, fainting, convulsions.
Treatment:
gastric lavage, administration of adsorbents, symptomatic therapy. For severe bradycardia, intravenous administration of atropine.
If the effect is insufficient, a drug with a positive chronotropic effect can be administered with caution.
Sometimes temporary placement of an artificial pacemaker may be necessary.
If AV block develops, intravenous administration of 1-2 mg of atropine, epinephrine or installation of a temporary pacemaker.
For ventricular extrasystole – lidocaine (class IA drugs are not used).
If there is a marked decrease in blood pressure, the patient should be transferred to the Trendelenburg position;
if there are no signs of pulmonary edema, intravenous administration of plasma-substituting solutions; if they are ineffective, administration of epinephrine, dopamine, dobutamine (to maintain chronotropic and inotropic effects and eliminate a pronounced decrease in blood pressure).
For hypoglycemia, intravenous administration of a dextrose (glucose) solution may be indicated.
For heart failure – cardiac glycosides, diuretics.
For convulsions, intravenous diazepam.
For bronchospasm – inhaled beta2-adrenergic agonists.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 °C
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Hemofarm LLC, Russia
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C |
| Manufacturer | Chemopharm LLC, Russia |
| Medication form | pills |
| Brand | Chemopharm LLC |
Other forms…
Related products
Buy Biprol, 10 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.