No products in the cart.
Atorvastatin, 10 mg 30 pcs
€4.84 €4.31
Description
Pharmacological action is hypolipidemic.
Competitively selectively inhibits HMG-CoA reductase, which converts 3- hydroxy-3-methylglutaryl-CoA into mevalonic acid (precursor of sterols, including cholesterol). Triglycerides and cholesterol in the liver are incorporated into LPLONP, enter the plasma, and are transported to peripheral tissues. LDLNP is formed from LDLNP, which is catabolized by interaction with high-affinity LDL receptors. Elevated plasma levels of total cholesterol, LDL cholesterol, and apolipoprotein B contribute to atherosclerosis and are risk factors for cardiovascular disease, whereas increased levels of HDL are associated with reduced risk of cardiovascular complications.
Atorvastatin lowers plasma cholesterol and lipoprotein levels by inhibiting HMG-CoA reductase and inhibits cholesterol synthesis in the liver by increasing the number of LDL receptors on the cell surface and enhances LDL uptake and catabolism. Suppresses the formation of LDL and the number of LDL particles. Reduces LDL-cholesterol levels in patients with homozygous familial hypercholesterolemia, which is usually resistant to therapy with hypolipidemic agents.
In most patients the effect is manifested 2 weeks after the start of therapy, the maximum effect develops by the 4th week and lasts for the whole period of treatment.
Toxic effect on CNS. Brain hemorrhage was observed in dogs when using atorvastatin for 3 months at a dose of 120 mg/kg/day, brain hemorrhage and formation of optic nerve vacuoles – in female dogs after 11 months of atorvastatin use at doses up to 280 mg/kg/day. The dose of 120 mg/kg/day created a systemic exposure approximately 16 times greater than that of the maximum therapeutic dose for humans (80 mg/day) in terms of AUC (0-24 h). In a two-year study, single tonic seizures were reported in two dogs (one at a dose of 10 mg/day, the other at a dose of 120 mg/day). There was no evidence of CNS damage in mice when atorvastatin was chronically administered for up to 2 years at doses up to 400 mg/day and in rats at doses up to 100 mg/day. These doses produced exposures 6-fold (mice) and 11-fold (rats) greater than those in humans at the recommended therapeutic dose of 80 mg per AUC(0-24 h).
Vascular damage in the CNS, characterized by perivascular hemorrhages, edema, and mononuclear cell infiltration of the perivascular spaces, has been reported in dogs given other drugs of this class. Chemically similar substances of the same class as atorvastatin caused dose-dependent degeneration of the optic nerve at a dose producing plasma concentrations 30 times greater than those in humans at the maximum recommended dose.
Carcinogenicity, mutagenicity, effects on fertility
In two-year studies of carcinogenicity in rats using doses of atorvastatin 10, 30 and 100 mg/kg/day, two rare tumors in muscle were found in females at the maximum dose: in one case it was rhabdomyosarcoma and in another, fibrosarcoma. This dose corresponded to systemic exposure values (plasma AUC0-24 h) 16 times greater than those in humans at an oral dose of 80 mg. In two-year studies of carcinogenicity in mice at doses of atorvastatin 100, 200, and 400 mg/kg/day, there was a significant increase in the incidence of liver adenoma at the maximum dose in males and liver carcinoma at the maximum dose in females. These cases were observed at a plasma AUC0 -24 h value approximately 6 times that of human exposure at an oral dose of 80 mg.
In vitro atorvastatin showed no mutagenic or clastogenic properties in the following tests (with/without metabolic activation): Ames test with Salmonella typhimurium and Escherichia coli, hypoxanthine-guanine phosphoribosyltransferase test and chromosome aberration test on Chinese hamster ovary cells. No in vivo mutagenicity was detected in a micronucleus test in mice.
In studies in rats at doses of atorvastatin up to 175 mg/kg (exposure 15 times higher than in humans) no adverse effects on fertility were found. When rats were injected with atorvastatin at a dose of 100 mg/kg/day (16 times the AUC in humans at a dose of 80 mg) for 3 months, aplasia and aspermia in the testicular appendages were recorded in 2 of 10 rats; testicular weight was significantly reduced at doses of 30 and 100 mg/kg and appendage weight was lower at the 100 mg/kg dose. Male rats that received atorvastatin at a dose of 100 mg/kg/day for 11 weeks before mating had decreased sperm motility and concentration, and the number of abnormal spermatozoa was increased. Atorvastatin had no adverse effects on sperm parameters and reproductive organs in dogs receiving it at doses of 10, 40, and 120 mg/kg for 2 years.
Atorvastatin is rapidly absorbed after oral administration, the degree of absorption increases in proportion to increasing dose, Cmax is reached within 1-2 hours. Absolute bioavailability is approximately 14%, systemic availability with respect to HMG-CoA reductase inhibition is approximately 30%. Low systemic availability is due to presystemic metabolism in the gastrointestinal mucosa and/or during “first passage” through the liver. Mean volume of distribution of atorvastatin is approximately 381 l. Binding to plasma proteins is ≥98%. Blood/plasma level ratio is approximately 0.25, which indicates poor atorvastatin penetration into erythrocytes. In the liver atorvastatin is extensively metabolized with the participation of cytochrome P450 isoenzyme CYP3A4 to form ortho- and parahydroxylated derivatives and various beta-oxidation products. In vitro, ortho- and parahydroxylated metabolites have an inhibitory effect against HMG-CoA reductase, comparable with that of atorvastatin. The inhibitory effect against HMG-CoA reductase is approximately 70% determined by the activity of circulating metabolites. Atorvastatin and its metabolites are excreted mainly with bile after hepatic and/or extrahepatic metabolism (not subjected to marked hepatic recirculation). T1/2 atorvastatin is 14 h. Due to the presence of active metabolites, inhibitory activity against HMG-CoA reductase persists for about 20-30 hours. Less than 2% of the oral dose of atorvastatin is detected in urine. It is not excreted during hemodialysis.
Peculiarities of pharmacokinetics in specific groups of patients
In elderly patients plasma concentrations of atorvastatin are higher (approximately 40% for Cmax and 30% for AUC) than in elderly patients. Cmax values are 20% higher in women and AUC values are 10% lower (not clinically relevant). Renal diseases do not influence on plasma concentrations of atorvastatin or its effect on lipid metabolism parameters. In patients with alcoholic cirrhosis concentrations of atorvastatin are significantly increased: in mild degree of liver dysfunction (Child Pugh Class A) – 4 times (both Cmax and AUC), in moderate degree of dysfunction (Child Pugh Class B) – Cmax 16 times, AUC – 11 times higher than normal.
Indications
Indications
Primary hypercholesterolemia (heterozygous familial and non-familial hypercholesterolemia, Fredrickson type IIa), combined (mixed) hyperlipidemia (Fredrickson types IIb and III), dysbetalipoproteinemia (Fredrickson type III) (as an addition to diet), familial endogenous hypertriglyceridemia (Fredrickson type IV), resistant to dietary methods treatment. Homozygous hereditary hypercholesterolemia (as an addition to lipid-lowering therapy, including autohemotransfusion of blood purified from LDL). Diseases of the cardiovascular system (including in patients without clinical manifestations of coronary artery disease, but with increased risk factors for its occurrence – age over 55 years, nicotine addiction, arterial hypertension, genetic predisposition), incl. against the background of dyslipidemia – secondary prevention to reduce the total risk of death, myocardial infarction, stroke, re-hospitalization for angina pectoris and the need for revascularization.
Pharmacological effect
Pharmacological effect
Pharmacological action – hypolipidemic.
Competitively selectively inhibits HMG-CoA reductase, which converts 3-hydroxy-3-methylglutaryl-CoA into mevalonic acid (a precursor of sterols, including cholesterol). Triglycerides and cholesterol in the liver are included in VLDL, enter the plasma and are transported to peripheral tissues. VLDL produces LDL, which is catabolized by interaction with high-affinity LDL receptors. An increase in plasma levels of total cholesterol, LDL cholesterol, and apolipoprotein B contributes to the development of atherosclerosis and is a risk factor for the development of cardiovascular diseases, while an increase in HDL levels is associated with a decrease in the risk of cardiovascular complications.
Atorvastatin reduces the levels of cholesterol and lipoproteins in the blood plasma by inhibiting HMG-CoA reductase, and also inhibits the synthesis of cholesterol in the liver, increasing the number of LDL receptors on the cell surface, and enhances the uptake and catabolism of LDL. Suppresses the formation of LDL and the number of LDL particles. Reduces LDL cholesterol levels in patients with homozygous familial hypercholesterolemia, which is usually resistant to treatment with lipid-lowering drugs.
In most patients, the effect appears 2 weeks after the start of therapy, the maximum effect develops by the 4th week and persists throughout the entire treatment period.
Toxic effect on the central nervous system. Cerebral hemorrhage was observed in dogs when using atorvastatin for 3 months at a dose of 120 mg/kg/day, cerebral hemorrhage and formation of optic nerve vacuoles was observed in female dogs after 11 months of using atorvastatin at doses up to 280 mg/kg/day. A dose of 120 mg/kg/day resulted in a systemic exposure approximately 16 times greater than the maximum human therapeutic dose (80 mg/day) based on AUC (0–24 hours). In a two-year study, single tonic seizures were recorded in two dogs (one at a dose of 10 mg/day, the other at a dose of 120 mg/day). There were no signs of CNS damage in mice with chronic administration of atorvastatin for up to 2 years at doses up to 400 mg/day and in rats at doses up to 100 mg/day. These doses produced exposures 6 times (mice) and 11 times (rats) the human exposure at the recommended therapeutic dose of 80 mg AUC (0-24 hours).
Vascular injury in the central nervous system, characterized by perivascular hemorrhage, edema, and mononuclear cell infiltration of the perivascular spaces, has been reported in dogs treated with other drugs in this class. Chemically similar substances in the same class as atorvastatin caused dose-dependent optic nerve degeneration at a dose producing plasma concentrations 30 times higher than those in humans at the maximum recommended dose.
Carcinogenicity, mutagenicity, effect on fertility
In two-year carcinogenicity studies in rats using atorvastatin doses of 10, 30 and 100 mg/kg/day, two rare muscle tumors were found in females at the highest dose: one was a rhabdomyosarcoma, the other a fibrosarcoma. This dose corresponded to systemic exposure values (plasma AUC0–24 h) that were 16 times higher than human exposure values at an 80 mg oral dose. In two-year carcinogenicity studies in mice at atorvastatin doses of 100, 200 and 400 mg/kg/day, there was a significant increase in the incidence of liver adenoma at the highest dose in males and liver carcinoma at the highest dose in females. These cases were observed at a -24 hour plasma AUC0 value approximately 6 times the human exposure value at an 80 mg oral dose.
In vitro, atorvastatin was not mutagenic or clastogenic in the following tests (with or without metabolic activation): the Ames test with Salmonella typhimurium and Escherichia coli, the hypoxanthine-guanine phosphoribosyltransferase test and the chromosomal aberration test on Chinese hamster ovary cells. No in vivo mutagenicity was detected in the micronucleus test in mice.
In studies in rats at doses of atorvastatin up to 175 mg/kg (exposure 15 times higher than exposure in humans), no negative effects on fertility were detected. When atorvastatin was administered to rats at a dose of 100 mg/kg/day (16 times higher than the AUC in humans at a dose of 80 mg), aplasia and aspermia were recorded in the epididymis in 2 out of 10 rats for 3 months; Testicular weight was significantly reduced at 30 and 100 mg/kg and epididymal weight was lower at 100 mg/kg. In male rats that received atorvastatin at a dose of 100 mg/kg/day for 11 weeks before mating, sperm motility and concentration were reduced, and the number of abnormal sperm was increased. Atorvastatin had no adverse effects on sperm parameters and reproductive organs in dogs treated at doses of 10, 40 and 120 mg/kg for 2 years.
Atorvastatin is rapidly absorbed after oral administration, the degree of absorption increases in proportion to increasing doses, Cmax is achieved within 1–2 hours. Absolute bioavailability is approximately 14%, systemic availability in relation to inhibition of HMG-CoA reductase is approximately 30%. Low systemic availability is due to first-pass metabolism in the gastrointestinal mucosa and/or during the “first pass” through the liver. The mean volume of distribution of atorvastatin is approximately 381 L. Plasma protein binding is ≥98%. The blood/plasma ratio is approximately 0.25, indicating poor penetration of atorvastatin into red blood cells. In the liver, atorvastatin is extensively metabolized with the participation of the CYP3A4 isoenzyme of cytochrome P450 with the formation of ortho- and parahydroxylated derivatives and various beta-oxidation products. In vitro, ortho- and parahydroxylated metabolites have an inhibitory effect on HMG-CoA reductase comparable to that of atorvastatin. The inhibitory effect on HMG-CoA reductase is approximately 70% determined by the activity of circulating metabolites. Atorvastatin and its metabolites are excreted mainly in bile after hepatic and/or extrahepatic metabolism (not subject to significant enterohepatic recirculation). T1/2 of atorvastatin is 14 hours. Due to the presence of active metabolites, the inhibitory activity against HMG-CoA reductase persists for about 20–30 hours. Less than 2% of the oral dose of atorvastatin is determined in the urine. It is not excreted during hemodialysis.
Features of pharmacokinetics in certain groups of patients
In elderly patients, plasma concentrations of atorvastatin are higher (approximately 40% for Cmax and 30% for AUC) than in younger adults. Cmax values in women are 20% higher, AUC is 10% lower (no clinical significance). Kidney disease does not affect plasma concentrations of atorvastatin or its effect on lipid metabolism. In patients with alcoholic cirrhosis of the liver, atorvastatin concentrations are significantly increased: with mild liver dysfunction (Child Pugh Class A) – 4 times (both C max and AUC), with moderate liver dysfunction (Child Pugh Class B) – Cmax 16 times, AUC – 11 times higher than normal.
Special instructions
Special instructions
Before starting Atorvastatin therapy, the patient must be prescribed a standard cholesterol-lowering diet, which he must follow during the entire treatment period.
The use of HMG-CoA reductase inhibitors to reduce blood lipid levels can lead to changes in biochemical parameters reflecting liver function. Liver function should be monitored before starting therapy, 6 weeks, 12 weeks after starting Atorvastatin and after each dose increase, and periodically, for example, every 6 months. An increase in the activity of liver enzymes in the blood serum may be observed during therapy with Atorvastatin. Patients who experience elevated enzyme levels should be monitored until enzyme levels return to normal. If alanine aminotransferase (ALT) or aspartic aminotransferase (AST) values are more than 3 times the upper acceptable limit, it is recommended to reduce the dose of Atorvastatin or discontinue treatment.
Atorvastatin should be used with caution in patients who abuse alcohol and/or have liver disease. Active liver disease or persistent increases in aminotransferase activity of unknown origin are contraindications to the use of Atorvastatin.
Treatment with Atorvastatin may cause myopathy. The diagnosis of myopathy (muscle pain and weakness in combination with an increase in creatine phosphokinase (CPK) activity more than 10 times the upper limit of normal) should be considered in patients with widespread myalgia, muscle soreness or weakness, and/or a marked increase in CPK activity. Patients should be warned that they should immediately tell their doctor if they experience unexplained muscle pain or weakness if they are accompanied by malaise or fever. Atorvastatin therapy should be discontinued in the event of a marked increase in CPK activity or in the presence of confirmed or suspected myopathy. The risk of myopathy during treatment with other drugs in this class was increased with concomitant use of cyclosporine, fibrates, erythromycin, niacin, or azole antifungals. Many of these drugs inhibit cytochrome P450 3A4-mediated metabolism and/or drug transport. Atorvastatin is biotransformed by CYP 3A4. When prescribing Atorvastatin in combination with fibrates, erythromycin, immunosuppressive agents, azole antifungals or nicotinic acid in lipid-lowering doses, the expected benefits and risks of treatment should be carefully weighed and patients should be regularly monitored for muscle pain or weakness, especially during the first months of treatment and during periods of increasing dosage of any drug. In such situations, periodic determination of CPK activity can be recommended, although such monitoring does not prevent the development of severe myopathy.
When using Atorvastatin, as well as other drugs of this class, cases of rhabdomyolysis with acute renal failure caused by myoglobinuria have been described. Atorvastatin therapy should be temporarily discontinued or discontinued if signs of possible myopathy occur or if there is a risk factor for the development of renal failure secondary to rhabdomyolysis (eg, severe acute infection, hypotension, major surgery, trauma, severe metabolic, endocrine and electrolyte disturbances, and uncontrolled seizures).
Before starting Atorvastatin therapy, an attempt should be made to control hypercholesterolemia through adequate dietary therapy, increased physical activity, weight loss in obese patients, and treatment of other conditions.
Patients should be warned to seek immediate medical attention if they experience unexplained muscle pain or weakness, especially if accompanied by malaise or fever.
Active ingredient
Active ingredient
Atorvastatin
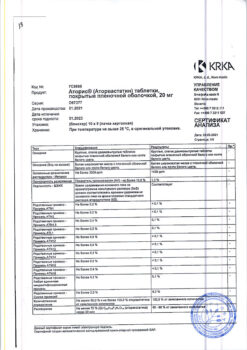
Composition
Composition
1 film-coated tablet contains:
active substance: atorvastatin calcium trihydrate – 10.85 mg, which corresponds to 10 mg of atorvastatin;
excipients: calcium carbonate, microcrystalline cellulose, milk sugar (lactose), starch 1500, colloidal silicon dioxide (aerosil), magnesium stearate, opadry II (polyvinyl alcohol, macrogol (polyethylene glycol), talc, titanium dioxide).
Contraindications
Contraindications
Hypersensitivity, active liver disease (including active chronic hepatitis, chronic alcoholic hepatitis), increased activity of liver transaminases (more than 3 times compared to the upper limit of normal) of unknown origin, liver failure, liver cirrhosis of any etiology, pregnancy and lactation.
Side Effects
Side Effects
In controlled clinical trials (n=2502), less than 2% of patients discontinued treatment due to side effects caused by atorvastatin. The most common adverse effects associated with atorvastatin were constipation, flatulence, dyspepsia and abdominal pain.
From the nervous system and sensory organs: ≥2% – headache, asthenic syndrome, insomnia, dizziness;
From the cardiovascular system: ≥2% – chest pain; blood pressure, phlebitis, arrhythmia, angina pectoris, anemia, lymphadenopathy, thrombocytopenia.
From the respiratory system: ≥2% – sinusitis, pharyngitis, bronchitis, rhinitis;
From the gastrointestinal tract: ≥2% – abdominal pain, constipation or diarrhea, dyspepsia, flatulence, nausea;
From the musculoskeletal system: ≥2% – arthralgia, myalgia, arthritis;
From the genitourinary system: ≥2% – urogenital infections, peripheral edema;
From the skin:
Allergic reactions: ≥2% – skin rash;
Other: ≥2% – infections, accidental trauma, influenza-like syndrome, back pain; ALP, increased ALT or AST, exacerbation of gout.
Side effects noted in post-marketing studies with atorvastatin therapy: anaphylaxis, angioedema, bullous rash (including erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis), rhabdomyolysis, tendon rupture.
Interaction
Interaction
The risk of developing myopathy during treatment with statins increases when used in combination with cyclosporine, fibrates, erythromycin, nicotinic acid in lipid-lowering doses, strong CYP3A4 inhibitors (including clarithromycin, HIV protease inhibitors, itraconazole).
When using atorvastatin in combination with inhibitors of the CYP3A4 isoenzyme (for example, cyclosporine, macrolide antibiotics – erythromycin and clarithromycin; itraconazole, HIV protease inhibitors), plasma concentrations of atorvastatin may increase (atorvastatin is metabolized with the participation of CYP3A4); Particular caution should be exercised when using atorvastatin in combination with the above-mentioned drugs (see “Special Instructions”).
With the combined use of atorvastatin at a dose of 40 mg and itraconazole at a dose of 200 mg 1 time per day, an increase in the AUC of atorvastatin by 3 times was detected compared to the AUC with monotherapy.
The simultaneous use of atorvastatin with protease inhibitors (lopinavir/ritonavir, ritonavir/saquinavir) was accompanied by an increase in the concentration of atorvastatin in the blood plasma. With simultaneous use of atorvastatin at a dose of 40 mg and the combination of lopinavir + ritonavir (at a dose of 400/100 mg 2 times a day), an increase in the AUC of atorvastatin by 5.9 times was detected compared to the AUC with monotherapy. When atorvastatin was used at a dose of 40 mg with the combination of ritonavir + saquinavir (at a dose of 400/400 mg 2 times a day), its AUC increased by 3.9 times.
Antacids reduce the concentration of atorvastatin by 35% (the effect on LDL cholesterol does not change).
With repeated administration of digoxin and atorvastatin, digoxin Css increases by approximately 20% (patients need to be monitored).
When atorvastatin is used together with oral contraceptives, the AUC of norethindrone and ethinyl estradiol increases by approximately 30 and 20% (this effect should be taken into account when choosing an oral contraceptive for a woman receiving atorvastatin).
When taken concomitantly with erythromycin (CYP3A4 inhibitor), the plasma concentration of atorvastatin increases by approximately 40%. The lipid-lowering effect of the combination of atorvastatin with colestipol is superior to that of each drug separately. Concomitant use with drugs that reduce the concentration or activity of endogenous steroid hormones (including ketoconazole, spironolactone, cimetidine) increases the risk of reducing the production of endogenous steroid hormones (caution should be exercised).
When atorvastatin was administered concomitantly with a suspension containing magnesium aluminum hydroxide, atorvastatin plasma concentrations were reduced by approximately 35%, but the degree of reduction in LDL/cholesterol levels did not change.
Overdose
Overdose
Treatment: there is no specific antidote; symptomatic therapy is carried out.
Hemodialysis is ineffective.
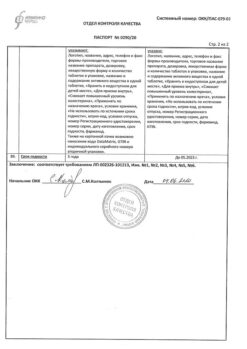
Storage conditions
Storage conditions
Store in a dry place, protected from light, out of reach of children, at a temperature of 15 C to 30 C.
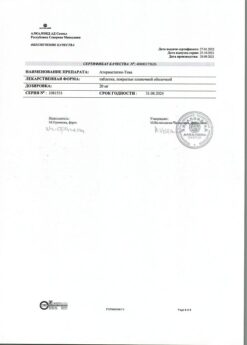
Shelf life
Shelf life
2 years.
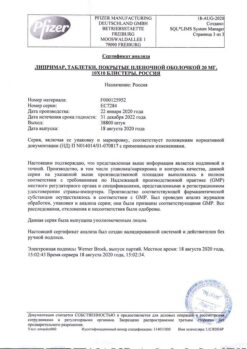
Manufacturer
Manufacturer
Ozon, Russia
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | Store in a dry place protected from light, out of the reach of children, at a temperature of 15 C to 30 C. |
| Manufacturer | Ozon, Russia |
| Medication form | pills |
| Brand | Ozon |
Other forms…
Related products
Buy Atorvastatin, 10 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.