No products in the cart.
Ascophen ULTRA, 250 mg+65 mg+250 mg 10 pcs
€4.81 €4.28
Description
Pharmacotherapeutic group: analgesic combined (non-steroidal anti-inflammatory agent + analgesic non-narcotic agent + psychostimulant).
The ATX code: [N02BA71].
Pharmacological properties
Pharmacodynamics:
A combined drug containing paracetamol, acetylsalicylic acid and caffeine.
Acetylsalicylic acid has antipyretic and anti-inflammatory effects, reduces pain, especially caused by inflammation, and inhibits platelet aggregation and thrombosis, improves microcirculation in the inflamed area.
Caffeine increases reflex excitability of the spinal cord, stimulates respiratory and vasomotor centers, increases blood vessels of skeletal muscles, brain, heart and kidneys; it decreases platelet aggregation; it reduces sleepiness and fatigue and increases mental and physical performance.
In this combination, a small dose of caffeine has practically no stimulating effect on the central nervous system, but it increases the tone of cerebral blood vessels and accelerates blood flow.
Paracetamol has analgesic, antipyretic and very weak anti-inflammatory activity, due to its effect on the thermoregulation center in the hypothalamus and weak ability to inhibit the synthesis of prostaglandins (Pg) in peripheral tissues.
Pharmacokinetics
Acetylsalicylic acid
When taken orally, absorption is complete. During absorption it undergoes presystemic elimination in the intestinal wall and systemic elimination in the liver (deacetylated). It is rapidly hydrolyzed by cholinesterases and albumin esterase, therefore half-life period is not more than 15-20 minutes.
In the body it circulates (75-90% in connection with albumin) and is distributed in the tissues as salicylic acid anion. The time of reaching maximum concentration is 2 hours. It is metabolized mainly in liver with formation of 4 metabolites found in many tissues and urine.
Extracted mainly by active secretion in the renal tubules as salicylate (60%) and its metabolites. Excretion of unchanged salicylate depends on urine pH (when urine is alkaline, ionization of salicylates increases, their reabsorption is impaired and excretion significantly increases).
The elimination rate depends on the dose: when taking small doses, the elimination half-life is 2-3 hours, with increasing doses it may increase to 15-30 hours. In infants the elimination of salicylates is much slower than in adults.
Caffeine
When taken orally absorption is good, occurs throughout the intestine. Absorption is mainly due to lipophilicity rather than water solubility.
The time to reach maximum concentration is 50-75 minutes after oral administration, the maximum concentration is 1.6-1.8 mg/l. It is rapidly distributed in all organs and tissues of the body; easily penetrates through the blood-brain barrier and the placenta.
The volume of distribution in adults is 0.4 – 0.6 l/kg, in infants 0.78-0.92 l/kg. Binding with blood proteins (albumin) is 25-36%. More than 90% is metabolized in liver, in children during first years of life up to 10-15%. In adults about 80% of caffeine dose is metabolized to paraxanthine, about 10% to theobromine and about 4% to theophylline.
These compounds are subsequently demethylated to monomethylxanthines and then to methylated uric acids. The elimination half-life in adults is 3.9-5.3 h (sometimes up to 10 h). Excretion of caffeine and its metabolites is carried out by kidneys (1-2% in adults is excreted unchanged).
Paracetamol
The absorption is high, the maximum concentration is reached after 0.5-2 hours; the maximum concentration is 5-20 mcg/ml. Binding with plasma proteins is 15%. Penetrates through the blood-brain barrier. Less than 1% of the dose taken by a nursing mother passes into breast milk.
The therapeutic effective concentration of paracetamol in plasma is achieved when administered at a dose of 10-15 mg/kg. It is metabolized in liver (90-95%): 80% enters into conjugation reactions to form inactive glucuronides and sulfates; 17% undergoes hydroxylation to form 8 active metabolites, which conjugate with glutathione to form already inactive metabolites.
With a lack of glutathione these metabolites can block the enzyme systems of hepatocytes and cause their necrosis. CYP2E1, CYP1A2 isoenzymes are also involved in metabolism of the drug, and to a lesser extent CYP3A4 isoenzyme. The elimination half-life is 1-4 hours. Excreted by the kidneys as metabolites, mainly conjugates, less than 5% unchanged. In elderly patients the drug clearance is decreased and the elimination half-life is increased.
Indications
Indications
Pain syndrome of moderate and mild intensity of various origins in adults and children over 15 years of age:
headache;
migraine;
toothache;
neuralgia;
arthralgia;
myalgia;
algodismenorrhea (pain during menstruation).
Feverish syndrome in adults: with acute respiratory diseases, influenza.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: combined analgesic (non-steroidal anti-inflammatory drug + analgesic non-narcotic drug + psychostimulant).
ATX code: [N02BA71].
PHARMACOLOGICAL PROPERTIES
Pharmacodynamics:
A combination drug containing paracetamol, acetylsalicylic acid and caffeine.
Acetylsalicylic acid has an antipyretic and anti-inflammatory effect, relieves pain, especially caused by the inflammatory process, and also inhibits platelet aggregation and thrombus formation, improves microcirculation in the area of inflammation.
Caffeine increases the reflex excitability of the spinal cord, stimulates the respiratory and vasomotor centers, dilates the blood vessels of skeletal muscles, brain, heart, kidneys, reduces platelet aggregation; reduces drowsiness, fatigue, increases mental and physical performance.
In this combination, caffeine in a small dose has virtually no stimulating effect on the central nervous system, but increases the tone of cerebral vessels and helps accelerate blood flow.
Paracetamol has an analgesic, antipyretic and extremely weak anti-inflammatory effect, which is associated with its effect on the thermoregulation center in the hypothalamus and a weak ability to inhibit the synthesis of prostaglandins (Pg) in peripheral tissues.
Pharmacokinetics
Acetylsalicylic acid
When taken orally, absorption is complete. During absorption, it undergoes presystemic elimination in the intestinal wall and systemic elimination in the liver (deacetylated). It is quickly hydrolyzed by cholinesterases and albuminesterase, so the half-life is no more than 15-20 minutes.
It circulates in the body (75-90% in connection with albumin) and is distributed in tissues in the form of salicylic acid anion. The time to reach maximum concentration is 2 hours. Metabolized primarily in the liver with the formation of 4 metabolites found in many tissues and urine.
It is excreted primarily by active secretion in the renal tubules in the form of salicylate (60%) and its metabolites. The excretion of unchanged salicylate depends on the pH of the urine (with alkalinization of the urine, the ionization of salicylates increases, their reabsorption worsens and excretion increases significantly).
The rate of elimination depends on the dose: when taking small doses, the half-life is 2-3 hours, with increasing doses it can increase to 15-30 hours. In newborns, the elimination of salicylates is much slower than in adults.
Caffeine
When taken orally, absorption is good and occurs throughout the intestine. Absorption occurs primarily due to lipophilicity rather than water solubility.
The time to reach maximum concentration is 50-75 minutes. after oral administration, the maximum concentration is 1.6-1.8 mg/l. Quickly distributed in all organs and tissues of the body; easily penetrates the blood-brain barrier and placenta.
The volume of distribution in adults is 0.4 – 0.6 l/kg, in newborns – 0.78-0.92 l/kg. Communication with blood proteins (albumin) – 25-36%. More than 90% is metabolized in the liver, in children of the first years of life up to 10-15%. In adults, about 80% of a caffeine dose is metabolized to paraxanthine, about 10% to theobromine, and about 4% to theophylline.
These compounds are subsequently demethylated into monomethylxanthines and then into methylated uric acids. The half-life in adults is 3.9-5.3 hours (sometimes up to 10 hours). Caffeine and its metabolites are excreted by the kidneys (1-2% is excreted unchanged in adults).
Paracetamol
Absorption is high, maximum concentration is achieved after 0.5-2 hours; maximum concentration – 5-20 µg/ml. Communication with plasma proteins – 15%. Penetrates the blood-brain barrier. Less than 1% of the dose of paracetamol taken by a nursing mother passes into breast milk.
The therapeutic effective concentration of paracetamol in plasma is achieved when administered at a dose of 10-15 mg/kg. Metabolized in the liver (90-95%): 80% enters into conjugation reactions with the formation of inactive glucuronides and sulfates; 17% undergoes hydroxylation to form 8 active metabolites, which conjugate with glutathione to form inactive metabolites.
With a lack of glutathione, these metabolites can block the enzyme systems of hepatocytes and cause their necrosis. The metabolism of the drug also involves isoenzymes CYP2E1, CYP1A2 and, to a lesser extent, the CYP3A4 isoenzyme. The half-life is 1-4 hours. It is excreted by the kidneys in the form of metabolites, mainly conjugates, less than 5% unchanged. In elderly patients, drug clearance decreases and the half-life increases.
Special instructions
Special instructions
General
This medicine should not be taken at the same time as medicines containing ASA or paracetamol.
As with other migraine treatments, caution should be exercised to rule out other potentially serious neurological disorders before initiating treatment for suspected migraine in patients who have not previously been diagnosed with migraine or in those whose migraine presents with atypical symptoms.
If patients vomit during >20% of migraine attacks or require bed rest during >50% of migraine attacks, the drug should not be used.
If the migraine does not stop after taking the first two tablets of the drug, you should seek medical help.
The drug should not be used if the patient has had more than 10 headache attacks per month for at least the last three months. In this case, headache due to excessive use of drugs should be suspected and treatment should be discontinued.
Additionally, patients should seek medical attention. Caution should be used in patients with risk factors for dehydration, such as vomiting, diarrhea, or before or after major surgery.
Due to its pharmacodynamic properties, the drug can mask the signs and symptoms of infection.
Due to the content of acetylsalicylic acid in the preparation
The drug should be used with caution in patients with gout, impaired renal or hepatic function, dehydration, uncontrolled hypertension, glucose-6-phosphate dehydrogenase deficiency and diabetes mellitus.
Due to ASA inhibition of platelet aggregation, the drug may lead to an increase in bleeding time during and after surgical interventions (including minor ones, such as tooth extraction).
The drug should not be used simultaneously with anticoagulants and other drugs that interfere with blood clotting, without medical supervision (see section “Interaction with other drugs”). Patients with bleeding disorders should be closely monitored. Caution should be exercised in case of metro- or menorrhagia.
If a patient develops bleeding or ulceration of the gastrointestinal tract while taking the drug, it must be discontinued immediately. Potentially fatal bleeding, ulceration, and perforation of the gastrointestinal tract may occur at any time during treatment with any NSAID, with or without a history of precursors and severe gastrointestinal complications.
These complications tend to be more severe in older patients. Alcohol, glucocorticosteroids and NSAIDs may increase the risk of gastrointestinal bleeding (see section “Interaction with other drugs”).
The drug may contribute to the development of bronchospasm and the occurrence of exacerbation of bronchial asthma (including bronchial asthma caused by intolerance to analgesics) or other hypersensitivity reactions. Risk factors include bronchial asthma, seasonal allergic rhinitis, nasal polyposis, chronic obstructive pulmonary disease, chronic respiratory tract infections (especially those associated with symptoms characteristic of allergic rhinitis).
Such effects may also occur in patients with allergic reactions (eg, skin reactions, including itching and urticaria) to other substances. Particular caution is recommended in such patients.
Children under 18 years of age should not be prescribed medications containing acetylsalicylic acid as an antipyretic, since in the case of a viral infection they can increase the risk of Reye’s syndrome. Symptoms of Reye’s syndrome are hyperpyrexia, prolonged vomiting, metabolic acidosis, nervous system and mental disorders, hepatomegaly and liver dysfunction, acute encephalopathy, respiratory failure, convulsions, coma.
ASA may interfere with laboratory tests of thyroid function due to false-positive low concentrations of levothyroxine (T4) and triiodothyronine (T3) (see section “Interactions with other drugs”).
Due to the content of paracetamol in the preparation
Caution should be exercised when prescribing the drug to patients with impaired renal or hepatic function, or alcohol dependence.
The risk of paracetamol poisoning is increased in patients taking other potentially hepatotoxic drugs or drugs that induce liver microsomal enzymes (eg, rifampicin, isoniazid, chloramphenicol, hypnotics and anticonvulsants including phenobarbital, phenytoin and carbamazepine). Patients with a history of alcoholism are at particular risk for liver damage (see section “Interaction with other drugs”).
When using the drug, serious skin reactions may develop, such as acute generalized exanthematous pustulosis, Stevens-Johnson syndrome, toxic epidermal necrolysis, which can be fatal. Patients should be informed of the signs of serious skin reactions. The drug should be discontinued at the first manifestation of skin reactions or any other signs of hypersensitivity.
Due to the caffeine content in the preparation
The drug should be prescribed with caution to patients with gout, hyperthyroidism and arrhythmia.
When using the drug, you should limit your consumption of products containing caffeine, since excess caffeine intake can lead to nervousness, irritability, insomnia and, in some cases, increased heart rate.
Impact on the ability to drive vehicles and machinery
Studies have not been conducted to study the effect on the ability to drive vehicles and operate machinery. If you experience undesirable reactions such as dizziness or drowsiness, you should refrain from these activities and tell your doctor.
Active ingredient
Active ingredient
Acetylsalicylic acid, Caffeine, Paracetamol
Composition
Composition
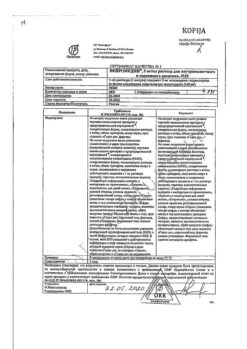
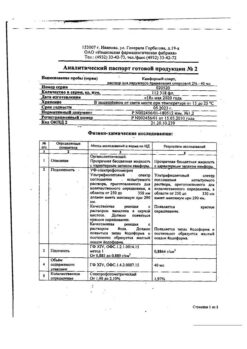
Active ingredients:
acetylsalicylic acid – 250.0 mg,
paracetamol – 250.0 mg,
caffeine (caffeine anhydrous) – 65.0 mg.
Excipients: microcrystalline cellulose – 66.01 mg, hyprolose (low-substituted hydroxypropylcellulose) – 21.50 mg, talc – 10.00 mg, hyprolose (hydroxypropylcellulose) – 7.30 mg, colloidal silicon dioxide (aerosil) – 3.40 mg, stearic acid – 2.50 mg, calcium stearate – 1.29 mg.
Shell: Opadry 20A28380 WHITE – 13.5 mg [hypromellose (hydroxypropyl methylcellulose 2910) – 4.556 mg, hydroxypropyl cellulose – 4.556 mg, talc – 2.700 mg, titanium dioxide – 1.688 mg].
Pregnancy
Pregnancy
Taking the drug is contraindicated during pregnancy and breastfeeding, because The safety of this combination in pregnant and breastfeeding women has not been studied.
Contraindications
Contraindications
Hypersensitivity to the main or auxiliary components of the drug;
erosive and ulcerative lesions of the gastrointestinal tract (GIT) (in the acute phase), gastrointestinal bleeding or perforation, a history of peptic ulcer;
complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid or other non-steroidal anti-inflammatory drugs (including a history);
hemophilia and other blood clotting disorders; hemorrhagic diathesis, hypoprothrombinemia;
vitamin K deficiency;
portal hypertension;
severe renal or liver failure;
chronic heart failure of NYHA functional class III-IV;
arterial hypertension of the III degree;
pregnancy;
breastfeeding period;
glaucoma;
deficiency of glucose-6-phosphate dehydrogenase;
increased nervous excitability, sleep disturbances;
surgical interventions accompanied by heavy bleeding;
children up to 15 years of age as an anesthetic, for febrile syndrome – up to 18 years of age;
simultaneous use of methotrexate at a dose of more than 15 mg/week.
With caution
Mild to moderate renal or liver failure, old age, gout, alcoholism, epilepsy and a tendency to seizures, chronic heart failure of NYHA functional class I-II, coronary heart disease, cerebrovascular diseases, peripheral arterial diseases, smoking, chronic obstructive pulmonary disease, simultaneous use of methotrexate at a dose of less than 15 mg/week, concomitant therapy with anticoagulants, older age, simultaneous use with non-steroidal anti-inflammatory drugs, glucocorticosteroids, anticoagulants, antiplatelet agents, selective serotonin reuptake inhibitors.
Side Effects
Side Effects
Many of the listed adverse reactions are clearly dose-dependent and vary from patient to patient. The frequency of adverse drug reactions is classified according to the recommendations of the World Health Organization: very common (>1/10), common (>1/100 to ≤1/10), uncommon (>1/1000 to ≤1/100), rare (>1/10000 to ≤1/1000), very rare (≤1/10000), frequency unknown (incidence cannot be determined) based on available data).
Infections and infestations:
rarely – pharyngitis.
Metabolic and nutritional disorders:
rarely – loss of appetite.
Mental disorders:
often – nervousness;
infrequently – insomnia;
rarely – anxiety, euphoric mood, internal tension.
Nervous system disorders:
often – dizziness;
uncommon – tremor, paresthesia, headache;
rarely – taste disorder, attention disorder, amnesia, impaired coordination of movement, hyperesthesia, pain in the paranasal sinuses.
Visual disorders:
rarely – visual impairment.
Hearing disorders:
infrequently – tinnitus.
Cardiovascular system disorders:
infrequently – arrhythmia.
Vascular disorders:
rarely – hyperemia, peripheral circulation disorders.
Disorders of the respiratory system, chest and mediastinal organs:
rarely – nosebleeds, hypoventilation, rhinorrhea.
Digestive system disorders:
often – nausea, abdominal discomfort;
uncommon – dry mouth, diarrhea, vomiting;
rarely – belching, flatulence, dysphagia, paresthesia in the mouth, increased salivation.
Disorders of the skin and subcutaneous tissues:
rarely – hyperhidrosis, itching, urticaria.
Musculoskeletal disorders:
rarely – musculoskeletal stiffness, neck pain, back pain, muscle spasms.
General disorders:
infrequently – fatigue, increased excitability;
rarely – asthenia, heaviness in the chest.
Other:
uncommon – increased heart rate.
Post-marketing surveillance data
System-organ class
From the immune system
Hypersensitivity
Mental disorders
Anxiety
Nervous disorders
Migraine, drowsiness
Skin and subcutaneous tissue disorders
Erythema, rash, angioedema, erythema multiforme
Cardiovascular disorders
Feeling of heartbeat
Vascular disorders
Lower blood pressure
Respiratory, thoracic and mediastinal disorders
Shortness of breath, bronchospasm
Digestive system disorders
Epigastric pain, dyspepsia, abdominal pain, gastrointestinal bleeding (including from the upper gastrointestinal tract, bleeding from the stomach, from a stomach ulcer, from a duodenal ulcer, from a rectum), erosive and ulcerative lesions of the gastrointestinal tract (including gastric ulcer, duodenal ulcer, colon, peptic ulcer)
Disorders of the liver and biliary tract
Liver failure
General violations
Malaise, feeling of discomfort
There is no data on an increase or expansion of the range of adverse effects of individual components when used as part of a combination in accordance with the instructions for use.
The increased risk of bleeding after taking acetylsalicylic acid persists for 4-8 days. Very rarely, severe bleeding (for example, cerebral hemorrhage) is possible, especially in patients with untreated hypertension and (or) with simultaneous use of anticoagulants, in some cases life-threatening.
If you experience the side effects listed in the instructions, or they get worse, or you notice any other side effects not listed in the instructions, tell your doctor.
Interaction
Interaction
Acetylsalicylic acid
Other non-steroidal anti-inflammatory drugs: Increased damaging effect on the mucous membrane of the gastrointestinal tract (GIT), increasing the risk of developing gastrointestinal bleeding. If simultaneous use is necessary, it is recommended to use gastroprotectors for the prevention of NPVH1-induced ulcers of the gastrointestinal tract, therefore simultaneous use is not recommended.
Glucocorticosteroids:
Increased damaging effect on the gastrointestinal mucosa, increased risk of gastrointestinal bleeding. If simultaneous use is necessary, it is recommended to use gastroprotectors, especially in persons over 65 years of age, therefore simultaneous use is not recommended.
Oral anticoagulants (for example, coumarin derivatives): Acetylsalicylic acid (ASA) may potentiate the effect of anticoagulants. Clinical and laboratory monitoring of bleeding time and prothrombin time is necessary. Simultaneous use is not recommended.
Thrombolytics:
Increased risk of bleeding. The use of ASA in patients within the first 24 hours after an acute stroke is not recommended. Simultaneous use is not recommended.
Heparin:
Increased risk of bleeding. Clinical and laboratory monitoring of bleeding time is required. Simultaneous use is not recommended.
Platelet aggregation inhibitors (ticlopidine, paracetamol, clopidogrel, cilostazol): Increased risk of bleeding. Clinical and laboratory monitoring of bleeding time is required. Simultaneous use is not recommended.
Selective serotonin reuptake inhibitors (SSRIs): Concomitant use may affect blood clotting or platelet function, resulting in an increased risk of bleeding in general, and gastrointestinal bleeding in particular, and concomitant use is not recommended.
Phenytoin: ASA increases plasma concentrations of phenytoin, which requires monitoring.
Valproic acid: ASA interferes with plasma protein binding and may therefore increase its toxicity. Monitoring of plasma concentrations of valproic acid is necessary.
Aldosterone antagonists (spironolactone, canrenoate): ASA may reduce their activity due to impaired sodium excretion; proper blood pressure control is necessary.
Loop diuretics (eg, furosemide): ASA may reduce their activity due to impaired glomerular filtration due to inhibition of prostaglandin synthesis in the kidneys.
Concomitant use of nonsteroidal anti-inflammatory drugs (NSAIDs) may lead to acute renal failure, especially in dehydrated patients. If diuretics are used concomitantly with ASA, ensure the patient is adequately rehydrated and monitor renal function and blood pressure, especially when diuretic treatment is initiated.
Antihypertensive drugs (ACE inhibitors, angiotensin II receptor antagonists, blockers of “slow” calcium channels): ASA can reduce their activity due to inhibition of prostaglandin synthesis in the kidneys. Concomitant use may lead to acute renal failure in elderly or dehydrated patients. If diuretics are used concomitantly with ASA, it is necessary to ensure adequate rehydration of the patient and monitor renal function and blood pressure. When used concomitantly with verapamil, bleeding time should be monitored.
Uricosurics (eg, probenecid, sulfinpyrazone): ASA may reduce their activity by inhibiting tubular reabsorption, leading to high plasma concentrations of ASA.
Methotrexate ≤15 mg/week: ASA, like all NSAIDs, reduces the tubular secretion of methotrexate, increasing its plasma concentration and thus toxicity. In this regard, the simultaneous use of NSAIDs in patients receiving high doses of methotrexate is not recommended (see section “Contraindications”).
In patients taking low doses of methotrexate, the risk of interaction between methotrexate and NSAIDs should also be considered, especially if renal function is impaired. If combination therapy is necessary, it is necessary to monitor a general blood count, liver and kidney function, especially in the first days of treatment.
Sulfonylureas and insulin: ASA enhances their hypoglycemic effect, therefore, when taking a high dose of salicylates, a reduction in the dose of hypoglycemic drugs may be necessary. It is recommended to monitor blood glucose levels more often.
Alcohol: Increases the risk of gastrointestinal bleeding; simultaneous use should be avoided.
Paracetamol
Inducers of liver microsomal enzymes or potentially hepatotoxic substances (for example, alcohol, rifampicin, isoniazid, hypnotics and antiepileptic drugs, including phenobarbital, phenytoin and carbamazepine): Increased toxicity of paracetamol, which can lead to liver damage even at non-toxic doses of paracetamol, so liver function should be monitored. Simultaneous use is not recommended.
Chloramphenicol: Paracetamol may increase the risk of increased chloramphenicol concentrations. Simultaneous use is not recommended.
Zidovudine: Paracetamol may increase the tendency to develop neutropenia, and therefore hematological parameters should be monitored. Simultaneous use is possible only with the permission of a doctor.
Probenecid: Probenecid reduces the clearance of paracetamol, which requires a reduction in the dose of paracetamol. Simultaneous use is not recommended.
Indirect anticoagulants: Repeated use of paracetamol for more than one week increases the anticoagulant effect. Occasional use of paracetamol has no significant effect.
Propantheline and other drugs that slow gastric emptying: Reduce the rate of absorption of paracetamol, which may delay or reduce rapid pain relief.
Metoclopramide and other drugs that accelerate gastric emptying: Increases the rate of absorption of paracetamol and, accordingly, the effectiveness and onset of analgesic action.
Cholestyramine: Reduces the rate of absorption of paracetamol, therefore, if maximum analgesia is needed, cholestyramine is taken no earlier than 1 hour after taking paracetamol.
Caffeine
Hypnotics (eg, benzodiazepines, barbiturates, H1-blockers): Concomitant use may reduce the hypnotic effect or reduce the anticonvulsant effect of barbiturates, so concomitant use is not recommended. If simultaneous use is necessary, it is advisable to take the combination in the morning.
Lithium: Caffeine withdrawal may increase plasma lithium concentrations because caffeine increases the renal clearance of lithium, so a lithium dose reduction may be necessary when caffeine is withdrawn. Simultaneous use is not recommended.
Disulfiram: Patients being treated with disulfiram should be warned to avoid caffeine to avoid the risk of worsening alcohol withdrawal syndrome due to the stimulating effects of caffeine on the cardiovascular and central nervous systems.
Ephedrine-like substances: Increased risk of developing drug dependence. Simultaneous use is not recommended.
Sympathomimetics or levothyroxine: Due to mutual potentiation, they can enhance the chronotropic effect. Simultaneous use is not recommended.
Theophylline: Concomitant use reduces the excretion of theophylline.
Antibacterial drugs from the quinolone group, enoxacin and pipemidic acid, terbinafine, cimetidine, fluvoxamine and oral contraceptives: Increased half-life of caffeine due to inhibition of liver cytochrome P450, so patients with impaired liver function, cardiac arrhythmias and latent epilepsy should avoid caffeine.
Nicotine, phenytoin and phenylpropanolamine: Reduce the terminal half-life of caffeine.
Clozapine: Caffeine increases clozapine serum concentrations, likely through both pharmacokinetic and pharmacodynamic mechanisms. Monitoring of serum concentrations of clozapine is necessary. Concomitant use is not recommended.
Impact on laboratory tests
High doses of ASA can distort the results of a number of clinical and biochemical laboratory studies.
The use of paracetamol may affect the results of determining uric acid using the phosphotungstic acid method and glycemia using the glucose oxidase/peroxidase method.
Caffeine may reverse the effects of dipyridamole on myocardial blood flow, thereby confounding the results of this study. During the study, it is necessary to refrain from taking caffeine for 8-12 hours.
Overdose
Overdose
Acetylsalicylic acid.
For mild intoxications – dizziness, tinnitus, deafness, increased sweating, nausea, vomiting, headache and confusion. Occurs at plasma concentrations of 150-300 mcg/ml.
Treatment is dose reduction or discontinuation of therapy.
At concentrations above 300 mcg/ml, more severe intoxication occurs, manifested by hyperventilation, fever, anxiety, ketoacidosis, respiratory alkalosis and metabolic acidosis. Central nervous system depression can lead to coma, and cardiovascular collapse and respiratory failure may also occur.
The greatest risk of developing chronic intoxication is observed in children and the elderly when taking more than 100 mg/kg/day for several days.
Treatment – If there is a suspicion of ingestion of more than 120 mg/kg of salicylates within the last hour, activated charcoal is injected repeatedly orally. When taking more than 120 mg/kg of salicylates, their plasma concentration should be determined, although it is impossible to predict its severity only on the basis of this indicator; clinical and biochemical parameters must also be taken into account.
If plasma concentrations exceed 500 mcg/mL (350 mcg/mL for children <5 years), intravenous sodium bicarbonate is effective in removing salicylates from plasma. If plasma concentrations exceed 700 mcg/mL (lower concentrations in children and the elderly) or in severe metabolic acidosis, hemodialysis or hemoperfusion is the treatment of choice.
Paracetamol overdose. In case of overdose, intoxication is possible, especially in elderly patients, children, patients with liver diseases (caused by chronic alcoholism), in patients with nutritional disorders, as well as in patients taking inducers of microsomal liver enzymes, in which fulminant hepatitis, liver failure, cholestatic hepatitis, cytolytic hepatitis can develop, in the above cases – sometimes with a fatal outcome.
The clinical picture of acute overdose develops within 24 hours after taking paracetamol. Symptoms: gastrointestinal disorders (nausea, vomiting, loss of appetite, abdominal discomfort and (or) abdominal pain), pale skin.
When simultaneous administration of 7.5 g or more to adults or more than 140 mg/kg to children, cytolysis of hepatocytes occurs with complete and irreversible liver necrosis, the development of liver failure, metabolic acidosis and encephalopathy, which can lead to coma and death.
12-48 hours after the administration of paracetamol, there is an increase in the activity of microsomal liver enzymes, lactate dehydrogenase, bilirubin concentration and a decrease in prothrombin content. Clinical symptoms of liver damage appear 2 days after an overdose of the drug and reach a maximum on days 4-6.
Treatment is immediate hospitalization. Determination of the quantitative content of paracetamol in blood plasma before starting treatment as early as possible after an overdose.
The introduction of SH-group donors and precursors for the synthesis of glutathione – methionine and acetylcysteine – is most effective in the first 8 hours. The need for additional therapeutic measures (further administration of methionine, intravenous (iv) administration of acetylcysteine) is determined depending on the concentration of paracetamol in the blood, as well as the time elapsed after its administration.
Symptomatic treatment. Laboratory tests of the activity of microsomal liver enzymes should be carried out at the beginning of treatment and then every 24 hours. In most cases, the activity of microsomal liver enzymes normalizes within 1-2 weeks. In very severe cases, a liver transplant may be required.
Caffeine. Common symptoms include gastralgia, agitation, delirium, anxiety, nervousness, restlessness, insomnia, mental agitation, muscle twitching, confusion, convulsions, dehydration, frequent urination, pyrexia, headache, increased tactile or pain sensitivity, nausea and vomiting (sometimes with blood), tinnitus.
In case of severe overdose, hyperglycemia may occur. Cardiac disorders are manifested by tachycardia and arrhythmia.
Treatment is to reduce the dose or stop caffeine.
Storage conditions
Storage conditions
Store in original packaging, in a dry place at a temperature not exceeding 25 °C.
Shelf life
Shelf life
2 years.
Manufacturer
Manufacturer
Pharmstandard-Leksredstva, Russia
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | Store in the original package, in a dry place at a temperature no higher than 25 ° C. |
| Manufacturer | Pharmstandard-Leksredstva, Russia |
| Medication form | pills |
| Brand | Pharmstandard-Leksredstva |
Related products
Buy Ascophen ULTRA, 250 mg+65 mg+250 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.