No products in the cart.
Ariprizol, tablets 30 mg 30 pcs
€212.43 €184.10
Description
Pharmacodynamics
. The therapeutic action of aripiprazole in schizophrenia and type 1 bipolar disorder is presumably due to a combination of partial agonist activity against D2-dopamine and 5HT1a-serotonin receptors and antagonist activity against 5HT2a-serotonin receptors. Aripiprazole in animal experiments showed antagonism to dopaminergic hyperactivity and agonism to dopaminergic hypoactivity. Aripiprazole has high in vitro affinity for D2- and D3-dopamine receptors, 5HT1a- and 5HT2a-serotonin receptors and moderate affinity for D4-dopamine, 5HT2c- and 5HT7-serotonin, α1-adrenoreceptors and H1-histamine receptors. Aripiprazole is also characterized by moderate affinity for serotonin reuptake sites and no affinity for m-cholinoreceptors. Some of the clinical effects of aripiprazole may be due to interactions with receptors other than dopamine and serotonin receptors.
Aripiprazole oral administration in healthy volunteers at doses of 0.5 to 30 mg once daily for 2 weeks shows a dose-dependent decrease in the binding of 11C-raclopride, a D2/D3-dopamine receptor ligand, to the caudate nucleus and the fence, as measured by positron emission tomography.
Pharmacokinetics
Intake
Aripiprazole is rapidly absorbed after oral administration, with maximum plasma concentration reached after 3-5 hours. Aripiprazole undergoes minimal presystemic metabolism. The absolute bioavailability of the tablets is 87%. High-fat foods have no effect on aripiprazole pharmacokinetics.
Distribution
Aripiprazole is intensely distributed in tissues, the apparent volume of distribution is 4.9 l/kg, indicating significant extravascular distribution. At therapeutic blood concentrations, aripiprazole and its main metabolite dehydroapiprazole are more than 99% bound to plasma proteins, mainly to albumin.
Metabolism
Aripiprazole is metabolized in the liver in three ways: dehydrogenation, hydroxylation and N-dealkylation. According to in vitro studies, dehydrogenation and hydroxylation of aripiprazole occurs under the action of CYP3A4 and CYP2D6 isoenzymes, and N-dealkylation is catalyzed by CYP3A4 isoenzyme. Aripiprazole is the main active ingredient in blood. At equilibrium the area under the concentration-time curve (AUC) of dehydroapiprazole is about 40% of the AUC of aripiprazole in plasma.
Elimination
Mean half-life (T1/2) of aripiprazole is approximately 75 hours in patients with high CYP2D6 isoenzyme activity and approximately 146 hours in patients with low activity of this isoenzyme. Total clearance of aripiprazole is 0.7 mL/min/kg, mainly due to hepatic excretion
After a single oral administration of [14C]-labeled aripiprazole, approximately 27% radioactivity is determined in the urine and approximately 60% in the feces. Less than 1% of unchanged aripiprazole is detected in the urine, and approximately 18% of the ingested dose is excreted unchanged in the feces.
Pharmacokinetics in special patient groups
Pharmacokinetics in children
The pharmacokinetics of aripiprazole and dehydroapiprazole in children from 10 to 17 years was the same as in adults after adjusting for differences in body weight.
Elderly patients
No age-related differences in aripiprazole pharmacokinetic parameters were found in adult patients with schizophrenia and in healthy volunteers.
Gender
No differences in pharmacokinetic parameters of aripiprazole in adult patients with schizophrenia and in age-matched healthy volunteers were found.
Smoking and Race
There were no clinically significant differences in aripiprazole pharmacokinetics based on race and smoking.
Kidney function impairment
Pharmacokinetic parameters of aripiprazole and dehydroapiprazole in patients with severe renal disease do not differ from those in healthy volunteers.
Liver function impairment
After a single dose of aripiprazole by individuals with varying degrees of severity of cirrhosis (Child-Pugh Class A, B, and C), there was no significant effect of hepatic function impairment on the pharmacokinetics of aripiprazole and dehydroariprazole, however, only three patients with decompensated cirrhosis (Child-Pugh Class C) participated in the study, so definitive conclusions cannot be drawn about liver metabolic activity in patients with decompensated cirrhosis.
Indications
Indications
Schizophrenia: acute attacks and maintenance therapy
Bipolar I disorder: manic episodes and maintenance therapy to prevent relapse in patients with bipolar I disorder who have recently had a manic or mixed episode
Adjunct to lithium or valproic acid therapy for the treatment of manic or mixed episodes of bipolar I disorder with or without psychotic symptoms and maintenance therapy to prevent relapse in patients with bipolar I disorder
Adjunct to antidepressant therapy for major depressive disorder
Pharmacological effect
Pharmacological effect
Pharmacodynamics
It is believed that the therapeutic effect of aripiprazole in schizophrenia and bipolar disorder type 1 is due to a combination of partial agonist activity at D2-dopamine and 5HT1a-serotonin receptors and antagonistic activity at 5HT2a-serotonin receptors. Aripiprazole in animal experiments showed antagonism in relation to dopaminergic hyperactivity and agonism in relation to dopaminergic hypoactivity. Aripiprazole has high in vitro affinity for D2 and D3 dopamine receptors, 5HT1a and 5HT2a serotonin receptors and moderate affinity for D4 dopamine, 5HT2c and 5HT7 serotonin, α1 adrenergic receptors and H1 histamine receptors. Aripiprazole is also characterized by moderate affinity for serotonin reuptake sites and lack of affinity for m-cholinergic receptors. Some of the clinical effects of aripiprazole may be due to interactions with receptors other than dopamine and serotonin.
When aripiprazole was administered orally to healthy volunteers at a dose of 0.5 to 30 mg once daily for 2 weeks, there was a dose-dependent decrease in the binding of 11C-raclopride, a ligand of the D2/D3 dopamine receptors, to the caudate nucleus and the cervix as measured by positron emission tomography.
Pharmacokinetics
Suction
After oral administration, aripiprazole is rapidly absorbed, with its maximum concentration in the blood plasma achieved after 3-5 hours. Aripiprazole undergoes first-pass metabolism to a minimal extent. The absolute bioavailability of tablets is 87%. A high-fat meal does not affect the pharmacokinetics of aripiprazole.
Distribution
Aripiprazole is extensively distributed into tissues, with an apparent volume of distribution of 4.9 L/kg, indicating significant extravascular distribution. At therapeutic concentrations in the blood, aripiprazole and its main metabolite dehydroaripiprazole are more than 99% bound to plasma proteins, mainly albumin.
Metabolism
Aripiprazole is metabolized in the liver in three ways: dehydrogenation, hydroxylation and N-dealkylation. According to in vitro studies, dehydrogenation and hydroxylation of aripiprazole occurs under the action of the CYP3A4 and CYP2D6 isoenzymes, and N-dealkylation is catalyzed by the CYP3A4 isoenzyme. Aripiprazole is the main active ingredient in the blood. At steady state, the area under the concentration-time curve (AUC) of dehydroaripiprazole is approximately 40% of the plasma AUC of aripiprazole.
Removal
The average half-life (T1/2) of aripiprazole is approximately 75 hours in patients with high activity of the CYP2D6 isoenzyme and approximately 146 hours in patients with low activity of this isoenzyme. The total clearance of aripiprazole is 0.7 ml/min/kg, mainly due to hepatic excretion
After a single oral dose of [14C] labeled aripiprazole, approximately 27% of the radioactivity is detected in the urine and approximately 60% in the feces. Less than 1% of unchanged aripiprazole is determined in the urine, and approximately 18% of the dose taken is excreted unchanged in the feces.
Pharmacokinetics in special groups of patients
Use in children
The pharmacokinetics of aripiprazole and dehydroaripiprazole in children 10 to 17 years of age were the same as in adults after adjustment for differences in body weight.
Elderly patients
No differences in the pharmacokinetics of aripiprazole in adult patients with schizophrenia and healthy volunteers due to age were identified.
Gender
There were no differences in the pharmacokinetics of aripiprazole in adult patients with schizophrenia and healthy volunteers due to gender.
Smoking and Race
There were no clinically significant differences in the pharmacokinetics of aripiprazole depending on race and smoking.
Renal dysfunction
The pharmacokinetic parameters of aripiprazole and dehydroaripiprazole in patients with severe kidney disease do not differ from those in healthy volunteers.
Liver dysfunction
After a single dose of aripiprazole in subjects with varying degrees of severity of liver cirrhosis (Child-Pugh Classes A, B and C), there was no significant effect of liver dysfunction on the pharmacokinetics of aripiprazole and dehydroaripiprazole; however, only three patients with decompensated liver cirrhosis (Child-Pugh Class C) were included in the study, and therefore it is impossible to make definitive conclusions. conclusions about the metabolic activity of the liver in patients with decompensated liver cirrhosis.
Special instructions
Special instructions
The therapeutic effect of antipsychotic drugs develops over several days to several weeks. During this period, it is necessary to monitor the patient’s condition.
Suicidal attempts.
The phenomenon of suicidal behavior is characteristic of psychosis and mood swings, in some cases it is observed immediately after the start or change of treatment with antipsychotic drugs, including treatment with aripiprazole. When treating with antipsychotic drugs, it is necessary to monitor patients at increased risk. The results of one epidemiological study showed that patients with schizophrenia or bipolar disorder did not experience an increased risk of suicidality when treated with aripiprazole compared with other antipsychotic drugs. There are insufficient clinical data to assess this risk in younger patients (<18 years of age), but there is evidence to suggest that the risk remains after 4 weeks of treatment with antipsychotic drugs, including aripiprazole.
Cardiovascular diseases.
Aripiprazole should be used with caution in patients with cardiovascular disease (myocardial infarction, coronary artery disease, heart failure, history of cardiac conduction disorders), cerebrovascular accidents, conditions predisposing to arterial hypotension (dehydration, hypovolemia, therapy with antihypertensive drugs) or hypertension, including essential or malignant.
Cases of venous thromboembolism have been reported with the use of antipsychotic drugs. Since patients treated with antipsychotic drugs often have acquired risk factors for the development of venous thromboembolism, it is necessary to determine all possible risk factors for the development of venous thromboembolism before and during treatment with Ariprizole® with preventive measures.
Conduction disorders.
In clinical studies of aripiprazole, the incidence of QT prolongation was comparable to the placebo group. Aripiprazole, like other antipsychotic drugs, should be used with caution in patients with a family history of QT prolongation.
Tardive dyskinesia.
In clinical studies lasting less than 1 year, infrequent cases of dyskinesia requiring urgent treatment were observed during treatment with aripiprazole. If a patient develops signs and symptoms of tardive dyskinesia while being treated with Ariprizole, dose reduction or discontinuation of treatment should be considered.
Symptoms of dyskinesia may temporarily increase or even appear for the first time after discontinuation of therapy.
Other extrapyramidal disorders.
Akathisia and parkinsonism were observed in clinical studies of aripiprazole in children. If signs and symptoms of other extrapyramidal disorders occur, consider reducing the aripiprazole dose and monitor the patient.
Neuroleptic malignant syndrome (NMS).
Neuroleptic malignant syndrome is a potentially life-threatening constellation of symptoms associated with the use of antipsychotic drugs. In clinical studies, rare cases of NMS were observed during treatment with aripiprazole, which is manifested by hyperpyrexia, muscle rigidity, mental disturbances and instability of the autonomic nervous system (irregular pulse and blood pressure, tachycardia, sweating, cardiac arrhythmia). In addition, in some cases, increased CPK activity, myoglobinuria (rhabdomyolysis) and acute renal failure occur. If symptoms of NMS or unexplained fever occur, all antipsychotics, including Ariprizole®, should be discontinued.
Cramps.
In clinical studies, infrequent cases of seizures were observed during treatment with aripiprazole. Therefore, aripiprazole should be used with caution in patients with a history of seizures and a risk of developing them.
Psychoses associated with senile dementia.
In three placebo-controlled clinical trials of aripiprazole in elderly patients (mean age 82.4 years, age range 56-99 years) with psychosis due to Alzheimer’s disease, an increased risk of death was observed compared with the placebo group. The mortality rate with aripiprazole was 3.5% compared with 1.7% in the placebo group. Although the causes of death varied, the underlying causes of most deaths were either cardiovascular disorders (including heart failure, sudden death) or infection (including pneumonia).
During these same clinical studies, cerebrovascular adverse reactions (including stroke, transient ischemic attack), including death, were reported in elderly patients (mean age 84 years, age range 78-88 years). Overall, 1.3% of patients treated with aripiprazole experienced cerebrovascular adverse events compared with 0.6% of patients treated with placebo. This difference was not statistically significant. However, one of these fixed-dose studies of aripiprazole found a significant dose relationship with cerebrovascular adverse reactions.
Ariprizole® is not recommended for use in patients with psychosis due to dementia.
Hyperglycemia and diabetes mellitus.
Hyperglycemia, in some cases severe and accompanied by ketoacidosis or hyperosmolar coma with a fatal outcome, has been noted in patients taking atypical antipsychotics. The relationship between atypical antipsychotics and hyperglycemic-type disorders remains unclear. In clinical studies of aripiprazole, there was no significant difference in the incidence of adverse reactions involving hyperglycemia (including diabetes) or changes in laboratory glycemic values compared with the placebo group.
Patients diagnosed with diabetes mellitus while taking atypical antipsychotics should regularly monitor their blood glucose concentrations.
Patients who have risk factors for developing diabetes mellitus (obesity, a family history of diabetes mellitus) when taking atypical antipsychotics should have their blood glucose levels determined at the beginning of the course and periodically while taking the drug. In patients taking atypical antipsychotics, constant monitoring of symptoms of hyperglycemia (increased thirst, frequent urination, polyphagia, weakness) is necessary. Particular attention should be paid to patients with diabetes mellitus and risk factors for its development.
Hypersensitivity.
As with other medications, hypersensitivity reactions in the form of allergic symptoms may occur when taking aripiprazole.
Increase in body weight.
Weight gain is commonly observed in patients with schizophrenia and bipolar mania due to the development of comorbidities, the use of antipsychotic drugs that cause weight gain, and unhealthy lifestyle choices that can lead to acute complications. Case reports of weight gain have been received during the post-marketing period in patients taking aripiprazole. Typically, these adverse reactions were observed in patients with significant risk factors, such as diabetes mellitus, thyroid disease or pituitary adenoma. In clinical studies, aripiprazole did not cause clinically significant weight gain.
In clinical studies of adolescent patients with bipolar mania treated with aripiprazole, body weight increased after 4 weeks of treatment. Continuous monitoring of body weight is necessary in adolescent patients with bipolar mania. If weight gain is clinically significant, the dose of aripiprazole should be reduced.
Dysphagia.
When using antipsychotics, there have been cases of disturbances in esophageal peristalsis and, as a consequence, aspiration pneumonia. The drug should be prescribed with caution to patients with risk factors for developing aspiration pneumonia.
Pathological attraction to gambling.
Post-marketing reports of pathological gambling have been reported in patients taking aripiprazole, regardless of whether these patients had a history of pathological gambling. Patients with a history of pathological gambling may be at increased risk of developing this disorder and should be closely monitored while using aripiprazole.
Lactose.
The drug Ariprizole® contains lactose, so it is not recommended for patients with rare hereditary diseases associated with galactose intolerance, lactase deficiency or glucose-galactose malabsorption.
Patients with concomitant attention deficit hyperactivity disorder (ADHD).
Despite the high incidence of co-occurrence of bipolar I disorder and ADHD, there are very limited data on the safety of the concomitant use of aripiprazole and psychostimulants, so caution should be exercised if they are used together.
Impact on the ability to drive vehicles and machinery
As with the use of other antipsychotics, when prescribing aripiprazole, the patient should be warned about the dangers of working with moving mechanisms and driving a car.
Active ingredient
Active ingredient
Aripiprazole
Composition
Composition
One tablet contains:
Contraindications
Contraindications
Hypersensitivity to aripiprazole or to any component of the drug;
age under 18 years;
lactase deficiency, rare hereditary galactosemia, glucose-galactose malabsorption.
With caution
In patients with cardiovascular diseases (coronary heart disease or previous myocardial infarction, heart failure and conduction disorders), cerebrovascular diseases and conditions predisposing to arterial hypotension (dehydration, hypovolemia and taking antihypertensive drugs) due to the possibility of developing orthostatic hypotension; in patients with seizures or suffering from diseases in which seizures are possible; in patients with an increased risk of hyperthermia (for example, during intense physical activity, overheating, taking m-anticholinergic drugs, dehydration due to the ability of antipsychotics to disrupt thermoregulation); in patients with an increased risk of aspiration pneumonia due to the risk of impaired motor function of the esophagus and aspiration; in obese patients and with a family history of diabetes; in patients at high risk of suicide (psychotic illnesses, bipolar disorders, major depressive disorder); in persons aged 18-24 years due to the risk of developing suicidal behavior.
Side Effects
Side Effects
The most commonly reported side effects in placebo-controlled clinical trials were akathisia and nausea, each of which occurred in more than 3% of patients treated with aripiprazole.
The following side effects are more common (≥ 1/100) compared to placebo or are identified as possible clinically significant side effects (*).
The following classification is used to indicate the frequency of side effects: often (˃ 1/100 and ˂ 1/10) and infrequently (˃ 1/1000 and ˂ 1/100):
Mental disorders:
often – restlessness, insomnia, anxiety;
infrequently – depression*, increased sexuality.
Nervous system disorders:
often – extrapyramidal disorders, akathisia, tremor, dizziness, drowsiness, sedation, headache.
Visual disorders:
often – blurred vision; infrequently – diplopia.
Cardiovascular system disorders:
uncommon – tachycardia*, orthostatic hypotension*.
Gastrointestinal disorders:
often – dyspepsia, vomiting, nausea, constipation, hypersecretion of saliva.
General violations:
often – fatigue.
Post-marketing surveillance
The following adverse reactions have been reported during post-marketing studies. The incidence of adverse reactions is considered unknown because it cannot be estimated based on available data.
From the hematopoietic organs: leukopenia, neutropenia, thrombocytopenia.
From the immune system: allergic reactions (anaphylactic shock, angioedema, including inflammation of the tongue, swelling of the tongue, swelling of the face, itching or urticaria).
From the endocrine system: hyperglycemia, diabetes mellitus, diabetic ketoacidosis, diabetic hyperosmolar coma.
Metabolism and nutrition: weight gain, weight loss, anorexia, hyponatremia.
Mental disorders: agitation, nervousness, pathological gambling, attempted suicide, suicidal thoughts, completed suicide.
From the nervous system: speech disorder, neuroleptic malignant syndrome, seizures, serotonin syndrome.
From the cardiovascular system: prolongation of the QT interval, ventricular arrhythmia, sudden death, cardiac arrest, tachycardia, bradycardia, syncope, increased blood pressure, thromboembolism (including pulmonary embolism and deep vein thrombosis).
From the respiratory system: oropharyngeal spasm, laryngospasm, aspiration pneumonia.
From the gastrointestinal tract: pancreatitis, dysphagia, heaviness in the abdomen, diarrhea.
From the liver and biliary tract: liver failure, jaundice, hepatitis, increased activity of alanine aminotransferase (ALT) and aspartate aminotransferase (AST).
From the skin and subcutaneous tissues: rash, photosensitivity, alopecia, hyperhidrosis.
From the musculoskeletal system: rhabdomyolysis, myaglia, muscle weakness.
From the urinary system: urinary incontinence, urinary retention.
From the reproductive system: priapism.
General disorders: disturbances in temperature regulation (including hypothermia, pyrexia), chest pain, peripheral edema, increased creatine phosphokinase (CPK) activity, increased blood glucose levels, fluctuations in blood glucose levels, increased glycohemoglobin levels.
Interaction
Interaction
Aripiprazole may enhance the effect of antihypertensive drugs because it has an antagonistic effect on alpha1-adrenergic receptors.
The mechanism of action of aripiprazole is associated with an effect on the central nervous system; this must be taken into account when used together with other drugs that have a central effect.
Caution should be exercised during the simultaneous use of aripiprazole and drugs that cause prolongation of the QT interval or disrupt electrolyte balance.
Effect of other drugs on aripiprazole
The H2-histamine receptor blocker famotidine reduces the rate of absorption of aripiprazole, however, this is not considered to have a clinically significant effect. Aripiprazole is metabolized in various ways, including through the CYP2D6 and CYP3A4 isoenzymes, but is not metabolized through the CYP1A isoenzyme, so dosage adjustment is not required for smoking patients.
Quinidine and other inhibitors of the CYP2D6 isoenzyme
Results from a clinical study in healthy patients showed that a potent inhibitor of the CYP2D6 isoenzyme (quinidine) increased the AUC of aripiprazole by 107%, while the Cmax remained unchanged. The AUC and Cmax of dehydroaripiprazole, the active metabolite, were reduced by 32% and 47%, respectively.
It is necessary to reduce the dose of aripiprazole by approximately half of the prescribed dose when coadministering aripiprazole with quinidine. Other strong CYP2D6 inhibitors, such as fluoxetine and paroxetine, may have similar effects, so a similar reduction in the dose of aripiprazole is recommended if they are used simultaneously.
Ketoconazole and other inhibitors of the CYP3A4 isoenzyme
Results from a clinical study in healthy patients showed that a potent inhibitor of the CYP3A4 isoenzyme (ketoconazole) increased aripiprazole AUC and Cmax by 63% and 37%, respectively. The AUC and Cmax of dehydroaripiprazole increased by 77% and 43%, respectively.
In slow metabolizers of the CYP2D6 isoenzyme, simultaneous use of potent inhibitors of the CYP3A4 isoenzyme may lead to high plasma concentrations of aripiprazole compared to rapid metabolizers of the CYP2D6 isoenzyme. When considering the simultaneous use of ketoconazole or other strong CYP3A4 inhibitors with aripiprazole, the possible benefit should outweigh the possible risk to the patient.
When using ketoconazole and aripiprazole simultaneously, the dose of Ariprizole should be reduced by approximately half the recommended dose.
When aripiprazole is co-administered with other strong CYP3A4 inhibitors, such as itraconazole and HIV protease inhibitors, a similar effect can be expected, so the dose of Ariprizole should also be reduced.
In case of discontinuation of an inhibitor of the CYP2D6 or CYP3A4 isoenzyme, the dose of Ariprizole should be increased to the level corresponding to the level before co-administration. With simultaneous use of aripiprazole and weak inhibitors of CYP3A4 isoenzymes (for example, diltiazem or escitalopram) or CYP2D6, a slight increase in the concentration of aripiprazole in blood plasma can be expected.
Carbamazepine and other inducers of the CYP3A4 isoenzyme
With simultaneous use of aripiprazole and carbamazepine, a strong inducer of the CYP3A4 isoenzyme, the geometric mean Cmax and AUC of aripiprazole were reduced by 68% and 73%, respectively, and the geometric mean Cmax and AUC of dehydroaripiprazole by 69% and 71%, respectively, compared with the use of 30 mg aripiprazole as monotherapy. When used together with carbamazepine, the dose of aripiprazole must be doubled. When aripiprazole is used together with other strong inducers of the CYP3A4 isoenzyme, such as rifampicin, rifabutin, phenytoin, phenobarbital, primidone, efavirenz, nevirapine and St. John’s wort, a similar effect can be expected, so the dose of Ariprizole should be increased. If you stop taking the CYP3A4 isoenzyme inducer, the dose of Ariprizole should be reduced to the recommended dose.
Valproic acid and lithium preparations
With simultaneous use of aripiprazole with lithium or valproic acid, no significant clinical changes in the concentration of aripiprazole in blood plasma were observed.
Serotonin syndrome
Cases of serotonin syndrome have been reported in patients taking aripiprazole. Signs and symptoms of this condition may occur especially when used with other serotonergic drugs, such as selective serotonin reuptake inhibitors (SSRIs) and selective serotonin-norepinephrine reuptake inhibitors (SNRIs), or drugs that increase plasma concentrations of aripiprazole.
Effect of aripiprazole on other drugs
In clinical studies, aripiprazole in doses of 10-30 mg/day did not have a significant effect on the metabolism of the substrates of the isoenzymes CYP2D6 (dextromethorphan/3-methoxymorphinan), CYP2C9 (warfarin), CYP2C19 (omeprazole) and CYP3A4 (dextromethorphan). In addition, aripiprazole and dehydroaripiprazole did not alter the biotransformation of drugs metabolized by the CYP1A2 isoenzyme in vitro.
Therefore, it is unlikely that aripiprazole would cause clinically significant effects of aripiprazole on drugs metabolized by these isoenzymes. When aripiprazole was co-administered with valproic acid, lithium or lamotrigine, no clinically significant changes in plasma concentrations of valproic acid, lithium or lamotrigine were observed.
Overdose
Overdose
Clinical studies have described cases of accidental or intentional overdose of aripiprazole with a single dose of up to 1260 mg, which were not accompanied by death.
Symptoms: lethargy, increased blood pressure, drowsiness, tachycardia, loss of consciousness, nausea, vomiting, diarrhea. In hospitalized patients, no clinically significant changes in basic physiological parameters, laboratory parameters and ECG were detected.
Cases of overdose of aripiprazole in children (taking up to 195 mg) without death have been described. Potentially dangerous symptoms of overdose are drowsiness, extrapyramidal disorders and transient loss of consciousness.
Treatment: monitoring vital signs, ECG to detect possible arrhythmia, supportive care, airway management, oxygenation, effective ventilation, activated charcoal, symptomatic treatment, careful medical observation until all symptoms disappear. There are no data on the use of hemodialysis for aripiprazole overdose; a beneficial effect of this method is unlikely, since aripiprazole is not excreted unchanged by the kidneys and is largely bound to plasma proteins.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25 °C. Keep out of the reach of children!
Shelf life
Shelf life
3 years.
Do not use after expiration date.
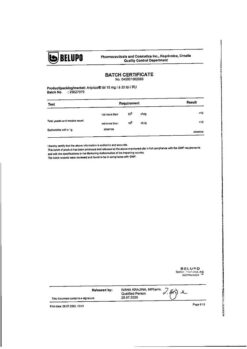
Manufacturer
Manufacturer
Belupo, medicines and cosmetics d.d., Croatia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25 °C. Keep out of reach of children! |
| Manufacturer | Belupo,medicines and cosmetics d.d., Croatia |
| Medication form | pills |
| Brand | Belupo,medicines and cosmetics d.d. |
Other forms…
Related products
Buy Ariprizol, tablets 30 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.