No products in the cart.
Aprovask, 5 mg+150 mg 28 pcs.
€22.27 €18.55
Description
A combined antihypertensive drug. The pharmacodynamic properties of each of the active ingredients in Aprovask®, irbesartan and amlodipine contribute to their additive antihypertensive effect when used in combination compared to when each drug is used alone. Both angiotensin II receptor antagonists (ARA II) and slow calcium channel blockers decrease BP by reducing peripheral vascular resistance, and the blockade of calcium entry into the cell and the reduction of angiotensin II-induced vasoconstrictor action are complementary mechanisms.
Irbesartan
Irbesartan is a selective potent ARA II (subtype AT1). Angiotensin II is an important component of the RAAS involved in the pathophysiology of arterial hypertension and in sodium ion homeostasis. Irbesartan does not require metabolic activation to manifest its action.
Irbesartan blocks the strong vasoconstrictor and aldosterone-secreting actions of angiotensin II through selective antagonism to angiotensin II receptors (subtype-AT1) located in vascular smooth muscle cells and adrenal cortex. Irbesartan has no agonist activity for AT1 receptors. Its affinity for AT1 receptors is 8,500 times greater than that for AT2 receptors (receptors that have not been shown to be associated with cardiovascular equilibrium [homeostasis] maintenance).
Irbesartan does not inhibit RAAS enzymes (such as renin, ACE) and does not affect other hormone receptors or ion channels in the cardiovascular system involved in the regulation of BP and sodium ion homeostasis. Blockade of AT1 receptors by irbesartan breaks the feedback loop in the renin-angiotensin system, increasing plasma concentrations of renin and angiotensin II. Irbesartan decreases plasma concentrations of aldosterone, but there are no significant changes in serum potassium when using the drug at the recommended doses (average increase in serum potassium is less than 0.1 mEq/L). Irbesartan has no significant effect on serum triglyceride, cholesterol or glucose concentrations. Irbesartan has no effect on serum concentrations of uric acid or renal excretion of uric acid.
The antihypertensive effect of irbesartan develops after the first dose and becomes significant within 1-2 weeks of treatment with maximal effect occurring after 4-6 weeks. In long-term observational studies, the effect of irbesartan persisted for more than 1 year.
Single administration of irbesartan in doses up to 900 mg/day caused a dose-dependent decrease in BP. A single dose of irbesartan 150-300 mg/day resulted in greater systolic (SBP)/diastolic (BP) decrease (24 hours after the dose) in the supine or sitting position (on average 8-13/5-8 mmHg) than placebo. The drug effect 24 h after the dose was 60-70% of the corresponding maximum reduction of BP and BP. Optimal efficacy with respect to 24-hour BP reduction is achieved with a single daily dose of the drug.
The BP decreases approximately equally in standing and lying position. Orthostatic effect is rare, and as with ACE inhibitors, its occurrence may be expected in patients with hyponatremia or hypovolemia.
The antihypertensive effects of irbesartan and thiazide diuretics are additive. In patients who do not achieve target BP values with irbesartan monotherapy, adding small doses of hydrochlorothiazide (12.5 mg) once daily to irbesartan causes an additional (compared to the effect of adding placebo) 7-10/3-6 mm Hg decrease in BP/DP, 24 hours after administration, respectively.
Age and gender have no effect on the efficacy of irbesartan. As with treatment with other drugs that affect the RAAS, a weaker antihypertensive effect is observed in non-Hispanic patients on irbesartan monotherapy. When irbesartan is taken with low-dose hydrochlorothiazide (e.g., 12.5 mg/day), the antihypertensive effect in non-Hispanic patients is similar to that in Caucasian patients.
After discontinuation of irbesartan, BP gradually returns to baseline. No withdrawal syndrome has been observed with discontinuation of irbesartan.
Amlodipine
Amlodipine is a slow calcium channel blocker from the group of dihydropyridine derivatives, which inhibits transmembrane entry of calcium ions into myocardial and vascular smooth muscle cells. The mechanism of antihypertensive action of amlodipine is associated with direct relaxant action on vascular smooth muscle.
The exact mechanism by which amlodipine reduces the frequency and severity of angina attacks is not fully established, but amlodipine reduces myocardial ischemia due to the following two effects.
1) Amlodipine dilates the peripheral arterioles and thereby reduces ROS, the so-called afterload. Because heart rate does not increase significantly when taking amlodipine, this decrease in cardiac output reduces myocardial energy expenditure and myocardial oxygen demand.
2) The mechanism of antianginal action of amlodipine also appears to be related to the dilation of the main coronary arteries and coronary arterioles, both in areas of myocardium with normal blood flow and in ischemic areas of myocardium. This dilation of the coronary vessels increases oxygen delivery to the myocardium in patients with coronary artery spasm (in Prinzmetal or variant angina).
In patients with arterial hypertension, administration of amlodipine once daily provides clinically significant reduction of BP in lying and standing position for 24 hours. Because of its slow onset of action, amlodipine is not indicated for the management of hypertensive crises.
In patients with angina pectoris, once daily administration of amlodipine during exercise testing increases total time to exercise, time to onset of angina attack and time to ST-segment depression of 1 mm on ECG. In addition, taking the drug reduces the daily number of angina attacks and the daily requirement for taking nitroglycerin tablets.
There have been no adverse metabolic effects or changes in blood lipid concentrations when taking amlodipine. Amlodipine can be administered to patients with bronchial asthma, diabetes mellitus and gout.
The clinical evidence for the efficacy of the fixed-dose combination of irbesartan and amlodipine came from two multicenter, prospective, open-label, parallel-group, blinded efficacy studies: the I-ADD and I-COMBINE studies. Results from both studies demonstrated significantly greater efficacy of fixed-dose combinations of irbesartan and amlodipine compared with amlodipine monotherapy or irbesartan monotherapy.
Indications
Indications
Arterial hypertension (if monotherapy with irbesartan or amlodipine is ineffective).
Pharmacological effect
Pharmacological effect
Combined antihypertensive drug. The pharmacodynamic properties of each of the active substances included in the drug Aprovac®, irbesartan and amlodipine, contribute to their additive antihypertensive effect when used in combination compared to that when each of these drugs is used separately. Both angiotensin II receptor antagonists (ARA II) and slow calcium channel blockers reduce blood pressure by reducing peripheral vascular resistance, blocking the entry of calcium into the cell and reducing the vasoconstrictor effect caused by angiotensin II are complementary mechanisms.
Irbesartan
Irbesartan is a selective, potent ARA II (subtype-AT1). Angiotensin II is an important component of the RAAS, involved in the pathophysiology of the development of arterial hypertension and in the homeostasis of sodium ions. Irbesartan does not require metabolic activation to exert its effect.
Irbesartan blocks the strong vasoconstrictor and aldosterone-secreting effects of angiotensin II due to selective antagonism of angiotensin II receptors (AT1 subtype) located in vascular smooth muscle cells and the adrenal cortex. Irbesartan does not have agonistic activity towards AT1 receptors. Its affinity for AT1 receptors is 8500 times greater than for AT2 receptors (receptors that have not been shown to be associated with maintaining cardiovascular equilibrium [homeostasis]).
Irbesartan does not inhibit RAAS enzymes (such as renin, ACE), and also does not affect other hormonal receptors or ion channels in the cardiovascular system involved in the regulation of blood pressure and sodium ion homeostasis. Blockade of AT1 receptors by irbesartan breaks the feedback loop in the renin-angiotensin system, increasing plasma concentrations of renin and angiotensin II. When using irbesartan, the plasma concentration of aldosterone decreases, however, when using the drug in recommended doses, there are no significant changes in the potassium content in the blood serum (the average increase in the potassium content in the blood serum is less than 0.1 mEq/L). Irbesartan does not have a significant effect on the concentrations of triglycerides, cholesterol or glucose in the blood serum. Irbesartan does not affect serum uric acid concentrations or renal excretion of uric acid.
The antihypertensive effect of irbesartan develops after the first dose and becomes significant within 1-2 weeks of treatment, with the maximum effect occurring after 4-6 weeks. In long-term observational studies, the effect of irbesartan was maintained for more than 1 year.
A single dose of irbesartan in doses up to 900 mg/day caused a dose-dependent decrease in blood pressure. A single dose of irbesartan in doses of 150-300 mg/day resulted in a greater decrease in systolic (SBP)/diastolic (DBP) blood pressure (24 hours after dosing) in the supine or sitting position (on average by 8-13/5-8 mmHg) than that observed with placebo. The effect of the drug 24 hours after dosing was 60-70% of the corresponding maximum reduction in DBP and SBP. Optimal effectiveness in reducing blood pressure within 24 hours is achieved with a single dose of the drug per day.
Blood pressure decreases to approximately the same extent in standing and lying positions. Orthostatic effects are rare and, as with ACE inhibitors, may be expected to occur in patients with hyponatremia or hypovolemia.
The antihypertensive effect of irbesartan and thiazide diuretics is additive. In patients who fail to achieve target blood pressure values with irbesartan monotherapy, adding small doses of hydrochlorothiazide (12.5 mg) to irbesartan once a day leads to an additional (compared to the effect of adding placebo) reduction in SBP/DBP, determined 24 hours after their administration, by 7-10/3-6 mmHg. Art., respectively.
Age and gender do not affect the effectiveness of irbesartan. As in the case of treatment with other drugs that affect the RAAS, patients of the Negroid race have a weaker antihypertensive effect with irbesartan monotherapy. When irbesartan is taken with low doses of hydrochlorothiazide (eg, 12.5 mg/day), the antihypertensive effect in black patients approaches that in Caucasian patients.
After discontinuation of irbesartan, blood pressure gradually returns to its original level. No withdrawal syndrome was observed upon discontinuation of irbesartan.
Amlodipine
Amlodipine is a slow calcium channel blocker from the group of dihydropyridine derivatives, which inhibits the transmembrane entry of calcium ions into myocardial cells and vascular smooth muscle. The mechanism of the antihypertensive effect of amlodipine is associated with a direct relaxing effect on vascular smooth muscle.
The exact mechanism by which amlodipine reduces the frequency and severity of angina attacks is not fully established, but amlodipine reduces myocardial ischemia through the following two effects.
1) Amlodipine dilates peripheral arterioles and thereby reduces peripheral vascular resistance, the so-called afterload. Because Heart rate practically does not increase when taking amlodipine; this decrease in the load on the heart muscle reduces the energy consumption of the myocardium and its need for oxygen.
2) The mechanism of the antianginal action of amlodipine also appears to be associated with the expansion of the main coronary arteries and coronary arterioles, both in areas of the myocardium with normal blood flow and in ischemic areas of the myocardium. This dilation of the coronary vessels increases oxygen delivery to the myocardium in patients with coronary artery spasm (Prinzmetal’s angina or variant angina).
In patients with arterial hypertension, taking amlodipine 1 time per day provides a clinically significant decrease in blood pressure in the supine and standing position for 24 hours. Due to the slow onset of its action, amlodipine is not intended for the relief of hypertensive crises.
In patients with angina pectoris, a single daily dose of amlodipine during an exercise test increases the total time of physical activity, the time before the onset of an angina attack and the time before the appearance of ST segment depression on an ECG with a depth of 1 mm. In addition, taking the drug reduces the daily number of angina attacks and the daily need for taking nitroglycerin tablets.
No adverse metabolic effects or changes in blood lipid concentrations were observed when taking amlodipine. Amlodipine can be prescribed to patients with bronchial asthma, diabetes mellitus and gout.
Clinical evidence of the efficacy of the fixed-dose combination of irbesartan and amlodipine was obtained from two multicenter, prospective, open-label, parallel-group, blinded efficacy studies: the I-ADD and I-COMBINE studies. The results of both studies demonstrated significantly greater efficacy of fixed-dose combinations of irbesartan and amlodipine compared with amlodipine monotherapy or irbesartan monotherapy.
Special instructions
Special instructions
Excessive decrease in blood pressure: patients with hypovolemia and hyponatremia
Irbesartan rarely caused an excessive decrease in blood pressure in patients with arterial hypertension without other concomitant pathology. As with ACE inhibitors, an excessive decrease in blood pressure with associated symptoms may be expected in patients with hypovolemia and hyponatremia, which include patients undergoing intensive diuretic therapy and/or patients with salt restrictions or patients on hemodialysis. Hyponatremia and hypovolemia should be corrected before starting treatment with Aprovask®, or the use of the drug at lower initial doses should be considered.
Patients with chronic heart failure
In a long-term placebo-controlled study (PRAISE-2) of amlodipine in patients with NYHA functional class III-IV chronic heart failure of non-ischemic etiology, amlodipine was associated with an increase in reports of pulmonary edema, despite no significant difference in the rate of progression of heart failure compared with placebo.
Liver failure
As with other slow calcium channel blockers, T1/2 of amlodipine is increased in patients with impaired liver function, and dosage recommendations for patients with impaired liver function have not been established. Therefore, Aprovask® should be used with caution in such patients.
Hypertensive crisis
The safety and effectiveness of the drug Aprovask® in hypertensive crisis have not been established.
Effect on kidney function
Due to inhibition of the RAAS, changes in renal function can be expected in predisposed patients. In patients whose renal function is dependent on the activity of the RAAS (hypertensive patients with renal artery stenosis of one or both kidneys or patients with chronic heart failure of functional class III-IV [NYHA classification]), treatment with other drugs that affect the RAAS has been associated with the development of oliguria and/or progressive azotemia and rarely with renal failure and/or death. The possibility of such an effect cannot be excluded when using ARA II, including irbesartan.
Double blockade of the RAAS when combining the drug Aprovask® with drugs containing aliskiren and an ACE inhibitor
Double blockade of the RAAS when using a combination of the drug Aprovask® with an ACE inhibitor or with aliskiren is not recommended, because there is an increased risk of developing a sharp decrease in blood pressure, hyperkalemia and renal dysfunction.
In patients with diabetes mellitus or moderate to severe renal failure (with GFR < 60 ml/min/1.73 m2 body surface area), the use of Aprovask® in combination with aliskiren is contraindicated.
For patients with diabetic nephropathy, the use of Aprovask® in combination with ACE inhibitors is contraindicated.
Use in elderly patients
In clinical studies, no difference in the effectiveness or safety of irbesartan was observed in elderly patients (65 years and older) compared with younger patients.
Use in pediatrics
Safety and effectiveness in children have not yet been established.
Impact on the ability to drive vehicles and operate machinery
The effect of the drug Aprovask® on the ability to drive vehicles or engage in other potentially hazardous activities that require increased attention has not been studied. However, based on the pharmacodynamic properties, the effect of the drug Aprovask® on this ability is unlikely. In case of dizziness, vertigo, weakness, driving or engaging in other potentially hazardous activities is not recommended.
Active ingredient
Active ingredient
Amlodipine, Irbesartan
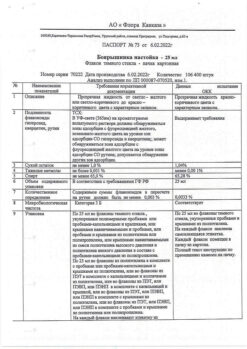
Composition
Composition
1 tab. amlodipine besylate 7 mg, which corresponds to the content of amlodipine 5 mg, irbesartan 150 mg
Excipients:
microcrystalline cellulose 50 microns – 66 mg,
croscarmellose sodium – 12 mg,
hypromellose 6 mPa s – 5 mg,
microcrystalline cellulose 100 microns – 5 mg,
colloidal silicon dioxide – 2.5 mg,
magnesium stearate – 2.5 mg.
Film shell composition:
opadry white (hypromellose – 62.5%, titanium dioxide (E171) – 31.25%, macrogol 400 – 6.25%) – 10 mg.
Contraindications
Contraindications
– hypersensitivity to irbesartan, amlodipine and other dihydropyridine derivatives, as well as to the excipients of the drug;
– cardiogenic shock;
– clinically significant aortic stenosis;
– unstable angina (with the exception of Prinzmetal’s angina);
– pregnancy;
– period of breastfeeding;
– children and adolescents under 18 years of age (efficacy and safety have not been established);
– simultaneous use with drugs containing aliskiren in patients with diabetes mellitus or with moderate to severe renal failure (GFR < 60 ml/min/1.73 m2);
– simultaneous use with ACE inhibitors in patients with diabetic nephropathy.
With caution:
In patients with hypovolemia and hyponatremia, occurring, for example, during intensive treatment with diuretics, hemodialysis, following a diet with limited salt intake, diarrhea, vomiting.
In patients whose renal function depends on the activity of the RAAS (such as patients with arterial hypertension with renal artery stenosis of one or both kidneys, patients with chronic heart failure of functional class III-IV according to the NYHA classification), treatment with drugs that affect the RAAS has been associated with the development of oliguria and/or progressive azotemia and rarely – acute renal failure and/or death, the risk of which cannot be excluded when taking ARA II, including irbesartan).
In patients with chronic heart failure of functional class II-IV according to the NYHA classification of non-ischemic etiology (due to the content of the drug amlodipine, the use of which in such patients was associated with an increase in reports of the development of pulmonary edema compared with placebo, despite the absence of differences in the incidence of progression of heart failure).
In patients with liver failure (risk of increasing T1/2 of amlodipine).
In patients with renal failure and after kidney transplantation (due to the content of irbesartan in the drug, monitoring of potassium levels and creatinine concentrations in the blood is recommended); after a recent kidney transplant (no experience with the clinical use of irbesartan).
In patients with aortic and mitral valve stenosis or hypertrophic obstructive cardiomyopathy (HOCM).
In patients with coronary artery disease and/or clinically significant cerebral atherosclerosis (with an excessive decrease in blood pressure, there is a risk of increased ischemic disorders, including the development of acute myocardial infarction and stroke).
In patients with SSSU (due to the content of amlodipine in the drug).
Side Effects
Side Effects
The frequency of adverse events/reactions (AEs/ARs) reported in clinical studies of the fixed-dose combination of irbesartan and amlodipine (clinical studies I-ADD, I-COMBINE and I-COMBO), in clinical studies of irbesartan and during its post-marketing use, as well as in clinical studies of amlodipine, was determined according to the WHO classification as follows: very often (≥ 10%); often (≥ 1% and < 10%); uncommon (≥ 0.1% and < 1%); rare (≥ 0.01% and < 0.1%); very rare (<0.01%), frequency unknown - based on the available data, it is impossible to estimate the frequency of occurrence of AEs/NRs.
The frequency of HP reported during post-marketing use of the drug was defined as “frequency unknown”, because information about these HPs came from spontaneous reports, without indicating the number of patients taking the drug.
In clinical studies comparing the fixed-dose combination of irbesartan/amlodipine with irbesartan or amlodipine monotherapy, the types and incidence of treatment-emergent adverse events possibly related to the study treatment were similar to those observed in prior clinical studies or in post-marketing reports with irbesartan and amlodipine monotherapy. The most common AE was peripheral edema, primarily related to amlodipine.
Adverse events observed during treatment and possibly related to the study drug in clinical studies of irbesartan/amlodipine (I-ADD, I-COMBINE and I-COMBO)
Fixed combination irbesartan/amlodipine
General reactions: often – peripheral edema, edema; infrequently – asthenia.
From the organ of hearing and labyrinthine disorders: infrequently – vertigo.
From the cardiovascular system: often – palpitations, orthostatic hypotension; infrequently – sinus bradycardia, excessive decrease in blood pressure.
From the nervous system: often – dizziness, headache, drowsiness; infrequently – paresthesia.
From the reproductive system: infrequently – erectile dysfunction.
From the respiratory system: infrequently – cough.
From the digestive system: often – swelling of the gums; infrequently – nausea, pain in the upper abdomen, constipation.
From the urinary system: often – proteinuria; infrequently – azotemia, hypercreatinemia.
From the side of metabolism: infrequently – hyperkalemia.
From the musculoskeletal system: uncommon – joint stiffness, arthralgia, myalgia.
Adverse events observed with irbesartan in clinical studies (including the I-ADD, I-COMBINE and I-COMBO clinical studies) and during its post-marketing use
From the immune system: frequency unknown – hypersensitivity reactions (allergic reactions), incl. angioedema, urticaria.
From the side of metabolism: frequency unknown – hyperkalemia.
From the organ of hearing and labyrinthine disorders: often – vertigo; frequency unknown – tinnitus.
From the nervous system: often – dizziness, headache*; infrequently – orthostatic dizziness.
* The incidence of headache in the I-ADD, I-COMBINE and I-COMBO studies was rated as “uncommon”.
From the cardiovascular system: infrequently – tachycardia.
From the skin and subcutaneous tissues: frequency unknown – leukocytoclastic vasculitis.
From the respiratory system: infrequently – cough.
From the digestive system: often – nausea/vomiting, pain in the upper abdomen, disorders of the tongue, glossodynia (burning sensation and soreness in the tongue); infrequently – diarrhea, dyspepsia, heartburn; frequency unknown – jaundice, increased liver function tests, hepatitis; frequency unknown – dysgeusia (taste perversion).
From the liver and biliary tract: frequency unknown – jaundice, increased liver function tests, hepatitis.
From the skin and subcutaneous tissues: infrequently – alopecia.
Allergic reactions: frequency unknown – angioedema, urticaria.
From the musculoskeletal system: frequency unknown – myalgia.
From the urinary system: frequency unknown – impaired renal function, including isolated cases of renal failure in patients with risk factors for its development.
From the reproductive system: infrequently – erectile dysfunction.
General reactions: often – increased fatigue*, swelling; infrequently – chest pain; frequency unknown – asthenia.
*The incidence of fatigue in the I-ADD, I-COMBINE and I-COMBO studies was rated as “uncommon”.
Injuries, intoxications and complications of manipulations: infrequently – falls.
Adverse events observed with amlodipine in clinical studies (including the I-ADD, I-COMBINE and I-COMBO clinical studies)
From the hematopoietic system: very rarely – thrombocytopenia.
From the immune system: very rarely – allergic reactions, incl. angioedema, urticaria.
From the side of metabolism: very rarely – hyperglycemia.
Mental disorders: infrequently – insomnia, mood lability.
From the nervous system: often – dizziness, headache*, drowsiness; infrequently – hypoesthesia, paresthesia, tremor, taste disturbances, syncope; very rarely – peripheral neuropathy.
* The incidence of headache in the I-ADD, I-COMBINE and I-SOMBO studies was rated as “uncommon”.
On the part of the organ of vision: infrequently – visual disturbances.
From the organ of hearing and labyrinthine disorders: infrequently – ringing in the ears, vertigo.
From the cardiovascular system: often – a feeling of palpitations, “flushes” of blood to the skin with a feeling of heat, redness of the skin*; very rarely – myocardial infarction, cardiac arrhythmias, ventricular tachycardia and atrial fibrillation (atrial fibrillation), vasculitis.
* The incidence of skin redness in the I-ADD, I-COMBINE and I-COMBO studies was rated as “uncommon”.
From the respiratory system: often – cough; infrequently – shortness of breath, rhinitis; very rarely – coughing.
From the digestive system: often – nausea, abdominal pain, glossodynia, glossitis; infrequently – dyspepsia, vomiting, change in the rhythm of bowel movements, dryness of the mucous membranes of the oral cavity; very rarely – pancreatitis, gastritis, gum hyperplasia.
From the liver and biliary tract: very rarely – hepatitis, jaundice and increased activity of liver enzymes (mainly associated with cholestasis).
From the skin and subcutaneous tissues: often – contact dermatitis; uncommon – skin rash, itching, purpura, increased sweating, changes in skin pigmentation (appearance of discolored areas of the skin), alopecia; very rarely – erythema multiforme.
From the musculoskeletal system: uncommon – arthralgia, muscle cramps, myalgia, back pain.
From the urinary system: infrequently – increased frequency of urination, painful urge to urinate, nocturia.
From the reproductive system: infrequently – impotence, gynecomastia.
General reactions: often – increased fatigue, swelling*, peripheral edema; infrequently – chest pain, asthenia, feeling of malaise, pain; rarely – swelling of the face.
* according to the I-ADD, I-COMBINE and I-COMBO studies, the incidence of edema: “uncommon”.
Laboratory and instrumental data: infrequently – increase in body weight, loss of body weight.
Interaction
Interaction
Combination of irbesartan and amlodipine
Based on pharmacokinetic studies in which irbesartan and amlodipine were taken individually and in combination, there was no pharmacokinetic interaction between irbesartan and amlodipine.
No studies have been conducted on the drug interaction of the drug Aprovask® with other drugs.
Irbesartan
Based on in vitro data, no interactions should be expected with drugs metabolized by the following isoenzymes: CYP1A1, CYP1A2, CYP2A6, CYP2B6, CYP2D6, CYP2E1 or CYP3A4.
Irbesartan is predominantly metabolized by the CYP2C9 isoenzyme, however, during clinical interaction studies when irbesartan was administered concomitantly with warfarin, which is metabolized by the CYP2C9 isoenzyme, no significant pharmacokinetic interaction was observed.
The pharmacokinetic parameters of irbesartan do not change when used simultaneously with nifedipine and hydrochlorothiazide.
Irbesartan does not change the pharmacokinetics of simvastatin, which is metabolized by the CYP3A4 isoenzyme or digoxin (a P-glycoprotein substrate).
The combination of Aprovask® with drugs containing aliskiren is contraindicated in patients with diabetes mellitus or moderate to severe renal failure (GFR < 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
The use of Aprovask® in combination with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended for other patients.
Based on experience with the use of other drugs that affect the RAAS, the simultaneous use of irbesartan with potassium preparations; salt substitutes containing potassium; Potassium-sparing diuretics or other drugs that can increase plasma potassium levels (heparin) can sometimes significantly increase serum potassium concentrations, which requires careful monitoring of plasma potassium levels in patients during treatment.
In elderly patients, patients with hypovolemia (due to taking diuretics) or with impaired renal function, simultaneous use of NSAIDs, including selective COX-2 inhibitors, with ARB II, including irbesartan, can lead to deterioration of renal function, including the development of acute renal failure. These effects are usually reversible. Renal function should be periodically monitored in patients concomitantly taking ARB II and NSAIDs, including selective COX-2 inhibitors.
During the combined use of irbesartan with lithium preparations, an increase in the concentration of lithium in the blood plasma and the toxic effect of lithium have been described. In patients taking irbesartan together with lithium preparations, lithium concentrations in the blood plasma should be monitored.
Amlodipine
Amlodipine has been safely combined with thiazide diuretics, beta-blockers, alpha-blockers, ACE inhibitors, long-acting nitrates, sublingual nitroglycerin, NSAIDs, antibiotics and oral hypoglycemic agents.
Data from in vitro studies with human plasma showed that amlodipine does not affect the plasma protein binding of digoxin, phenytoin, warfarin or indomethacin.
Concomitant use of amlodipine and cimetidine did not affect the pharmacokinetics of amlodipine.
Concomitant administration of 250 mg grapefruit juice with a single dose of 10 mg amlodipine in 20 healthy volunteers did not have a significant effect on the pharmacokinetics of amlodipine.
When amlodipine and sildenafil were taken in combination, each drug independently exhibited its blood pressure-lowering effect.
Simultaneous course administration of amlodipine at a dose of 10 mg and atorvastatin at a dose of 80 mg led to unreliable changes in the pharmacokinetic parameters of atorvastatin in the state of achieving Css.
Concomitant administration of amlodipine with digoxin did not alter serum digoxin concentrations or renal clearance of digoxin in healthy volunteers.
Concomitant use of amlodipine did not change the prothrombin time when taking warfarin.
Pharmacokinetic studies with cyclosporine have demonstrated that amlodipine does not have a significant effect on the pharmacokinetics of cyclosporine.
With simultaneous use of tacrolimus and amlodipine, an increase in the concentration of tacrolimus in the blood plasma is possible. It is necessary to monitor the concentration of tacrolimus in the blood plasma and, if necessary, adjust its dose.
Concomitant use of amlodipine with simvastatin may increase the exposure of simvastatin compared to simvastatin therapy. When using simvastatin and amlodipine simultaneously, it is necessary to limit the daily dose of simvastatin to 20 mg.
Overdose
Overdose
Symptoms: when adults take irbesartan in doses up to 900 mg/day, no toxicity has been established.
Available data for amlodipine suggest that severe overdose may lead to significant peripheral vasodilation and possibly the development of reflex tachycardia. The development of a pronounced and prolonged excessive decrease in blood pressure, up to the development of shock with a fatal outcome, has been reported.
Treatment: The patient should be under close medical supervision. Treatment should be symptomatic and support the basic vital functions of the body.
There is no specific information on the treatment of irbesartan overdose. Suggested measures in case of overdose of the drug Aprovask® include gastric lavage. Administration of activated charcoal to healthy volunteers immediately after or 2 hours after oral administration of 10 mg amlodipine showed a slight decrease in amlodipine absorption.
Due to the fact that amlodipine is characterized by a high degree of binding to blood proteins, and irbesartan is not excreted from the body by hemodialysis, it is unlikely that hemodialysis would be useful in case of overdose.
In case of severe overdose, active monitoring of cardiac activity and respiration should be initiated. Frequent blood pressure measurements are necessary. A clinically significant decrease in blood pressure due to an overdose of amlodipine requires active maintenance of cardiovascular activity, including placing the limbs in an elevated position. Blood volume and diuresis should be monitored. It may be necessary to administer vasoconstrictor drugs to restore vascular tone and blood pressure (provided there are no contraindications to their administration). IV administration of calcium gluconate may be helpful in reversing the effects of calcium channel blockade.
Storage conditions
Storage conditions
The drug should be stored out of the reach of children at a temperature not exceeding 30°C.
Shelf life
Shelf life
3 years.
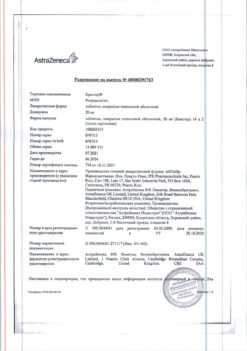
Manufacturer
Manufacturer
Sanofi-Aventis de Mexico S.A. de S.V., Mexico
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | The drug should be kept out of reach of children at a temperature not exceeding 30 ° C. |
| Manufacturer | Sanofi-Aventis de Mexico S.A. de S.V., Mexico |
| Medication form | pills |
| Brand | Sanofi-Aventis de Mexico S.A. de S.V. |
Other forms…
Related products
Buy Aprovask, 5 mg+150 mg 28 pcs. with delivery to USA, UK, Europe and over 120 other countries.