No products in the cart.
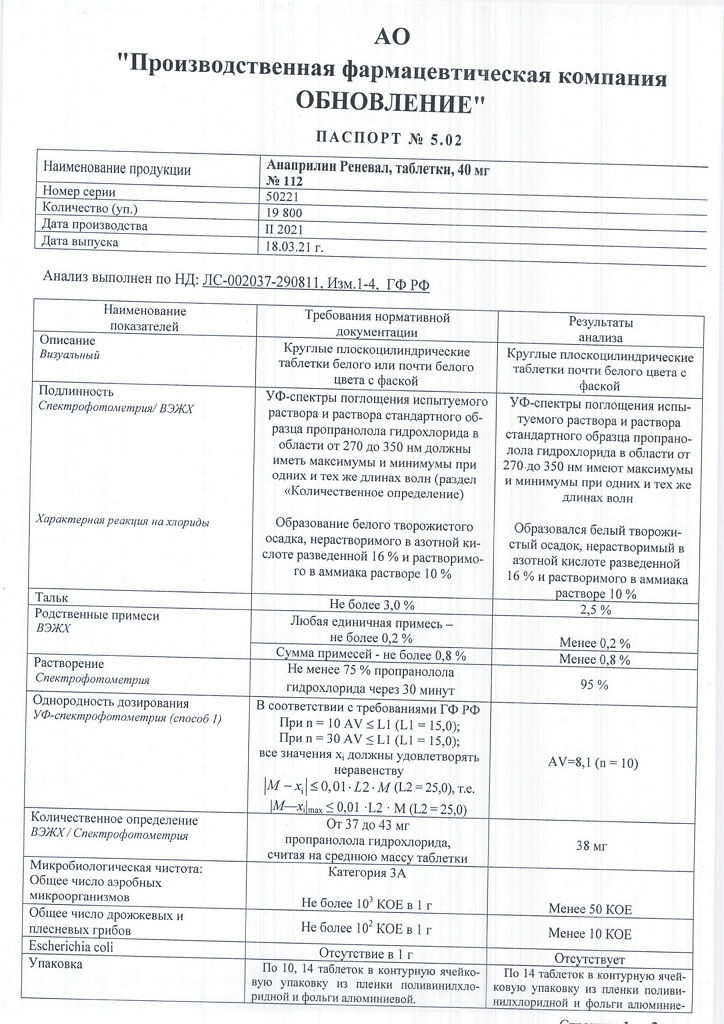
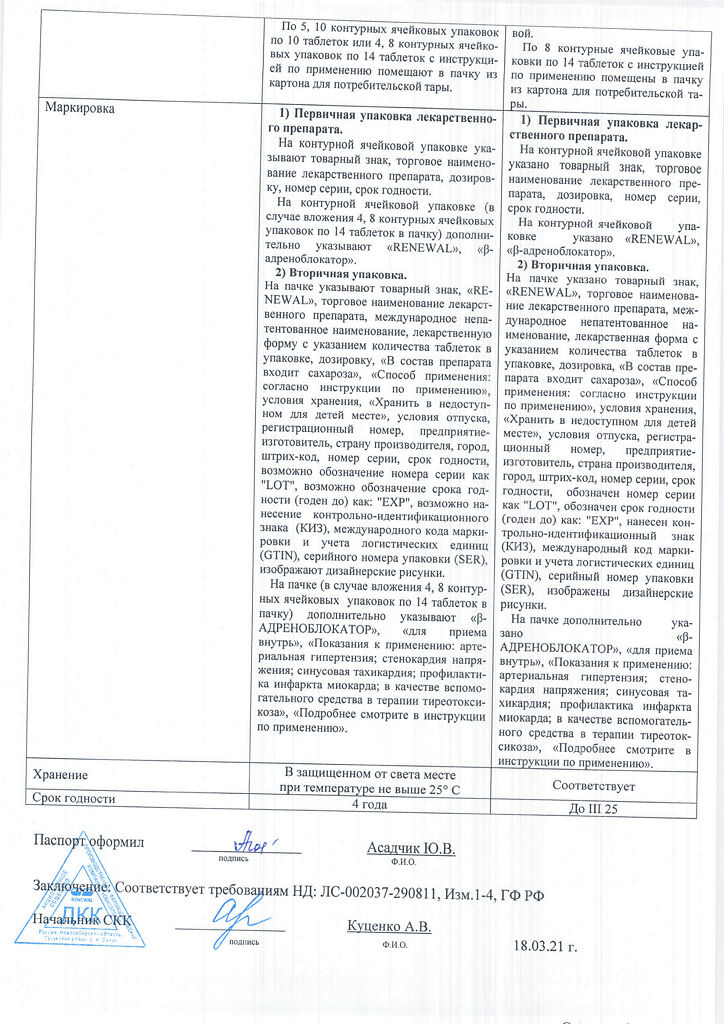
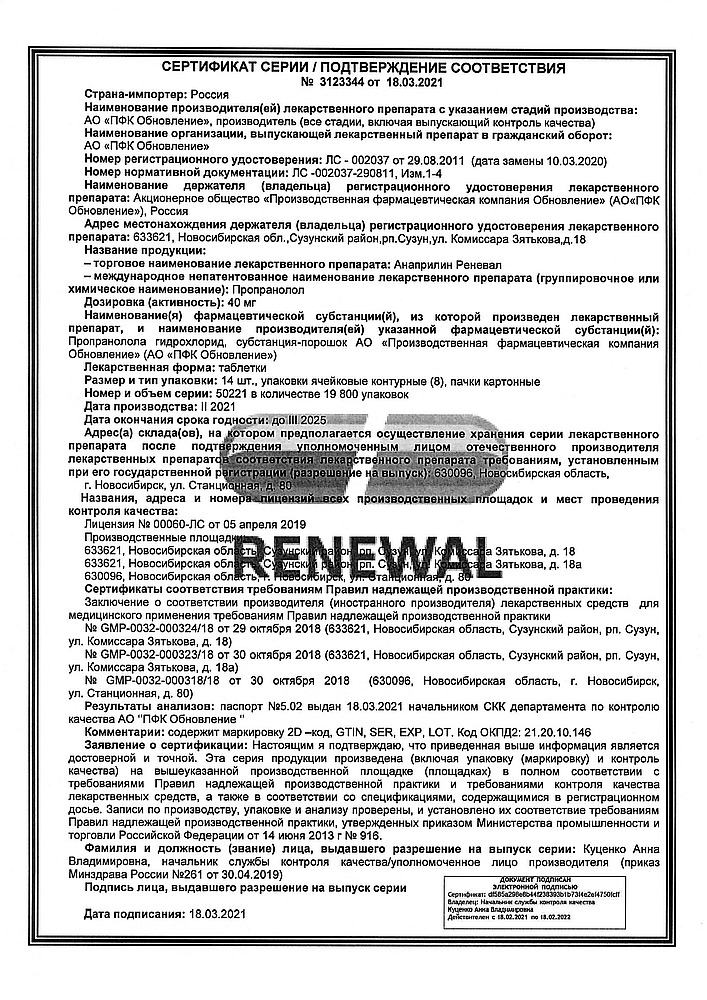
Anapriline Reneval, tablets 40 mg 112 pcs
€4.06 €3.99
Description
Nonselective beta-adrenoblocker. It has antianginal, hypotensive and antiarrhythmic effects. By nonselectively blocking beta-adrenoreceptors (75% beta1– and 25% beta2– adrenoreceptors), reduces catecholamine-stimulated formation of cAMP from ATP, resulting in decreased intracellular calcium supply, has negative chrono-, dromo-, batmo- and inotropic effects (decreases heart rate, inhibits conduction and excitability, decreases myocardial contractility).
In the beginning of beta-adrenoblocker use, total peripheral vascular resistance increases during the first 24 h (as a result of a reciprocal increase in alpha-adrenoreceptor activity and elimination of beta stimulation2-adrenoreceptors of skeletal muscle vessels), but in 1-3 days it returns to baseline and decreases with prolonged administration.
Hypotensive effect is associated with decreased cardiac output, sympathetic stimulation of peripheral vessels, decreased activity of reninangiotensin system (relevant in patients with initial renin hypersecretion), sensitivity of aortic arch baroreceptors (there is no increase of their activity in response to decreased blood pressure) and the effect on the central nervous system. Hypotensive effect stabilizes by the end of 2 weeks of course prescription.
The antianginal effect is caused by the decrease of myocardial oxygen demand (due to the negative chronotropic and inotropic effect). Decrease of heart rate leads to prolongation of diastole and improvement of myocardial perfusion.
By increasing left ventricular end-diastolic pressure and increasing ventricular muscle fiber stretch may increase oxygen demand, especially in patients with chronic heart failure.
The antiarrhythmic effect is caused by the elimination of arrhythmogenic factors (tachycardia, increased sympathetic nervous system activity, increased cyclic AMP, arterial hypertension), decreased rate of spontaneous excitation of sinus and ectopic pacemakers and slowing of atrioventricular conduction.
The inhibition of pulse conduction is observed predominantly in antegrade and to a lesser extent in retrograde direction through the atrioventricular node and along accessory pathways. According to the classification of antiarrhythmic drugs, it belongs to group II drugs.
Decreasing the severity of myocardial ischemia – by reducing myocardial oxygen demand, postinfarction mortality may also decrease due to antiarrhythmic action.
The ability to prevent the development of vascular headache is due to a decrease in the severity of cerebral artery dilation due to beta-adrenoblockade of vascular receptors, inhibition of catecholamine-induced platelet aggregation and lipolysis, reduction of platelet adhesiveness, prevention of clotting factor activation during adrenaline release, stimulation of tissue oxygen supply and reduction of renin secretion.
The reduction of tremor on propranololol administration may be due to blockade of beta2-adrenoreceptors. Increases the atherogenic properties of the blood. Increases uterine contractions (spontaneous and induced by drugs that stimulate the myometrium). Increases the tone of the bronchi.
Pharmacokinetics
It is quickly and fairly completely (90%) absorbed when ingested and relatively quickly eliminated from the body. Bioavailability after oral administration is 30-40 % (effect of “first passage” through the liver,
microsomal oxidation); with prolonged administration it increases (metabolites are formed which inhibit liver enzymes); its quantity depends on the character of food and intensity of liver blood flow.
It is metabolized by glucuronidation in the liver. Maximum concentration in blood plasma is reached after 1-1.5 hours. It is highly lipophilic and accumulates in lung tissue, brain, kidney and heart. It penetrates through the blood-brain barrier, placental barrier and into breast milk. Binding with blood plasma proteins is 90-95%. Distribution volume is 3-5 l/kg.
Getting into the intestine with bile, it is deglucuronized and reabsorbed. Period of semiejection is 3-5 hours; it may be prolonged up to 12 hours during a course of administration. Renal excretion is 90%, unchanged less than 1%. It is not eliminated by hemodialysis.
Indications
Indications
– Arterial hypertension;
– angina pectoris;
– unstable angina;
– sinus tachycardia (including with hyperthyroidism);
– supraventricular tachycardia;
– atrial fibrillation;
– supraventricular and ventricular extrasystole;
– prevention of myocardial infarction (systolic blood pressure more than 100 mm Hg);
– pheochromocytoma (together with alpha-blockers);
– essential tremor;
– migraine (prevention of attacks);
– as an adjuvant in the treatment of thyrotoxicosis and thyrotoxic crisis (in case of intolerance to thyreostatic drugs);
– sympatho-adrenal crises against the background of diencephalic syndrome.
Pharmacological effect
Pharmacological effect
Non-selective beta blocker. It has antianginal, hypotensive and antiarrhythmic effects. By non-selectively blocking beta-adrenergic receptors (75% beta1- and 25% beta2-adrenergic receptors), it reduces the formation of cAMP from ATP, stimulated by catecholamines, as a result of which it reduces the intracellular supply of calcium, has a negative chrono-, dromo-, batmo- and inotropic effect (reduces heart rate, inhibits conductivity and excitability, reduces contractility myocardium).
At the beginning of the use of beta-blockers, the total peripheral vascular resistance increases in the first 24 hours (as a result of a reciprocal increase in the activity of alpha-adrenergic receptors and the elimination of stimulation of beta2-adrenergic receptors in the vessels of skeletal muscles), but after 1-3 days it returns to the original level, and with long-term administration it decreases.
The hypotensive effect is associated with a decrease in cardiac output, sympathetic stimulation of peripheral vessels, a decrease in the activity of the renin-angiotensin system (important in patients with initial hypersecretion of renin), the sensitivity of the aortic arch baroreceptors (there is no increase in their activity in response to a decrease in blood pressure) and an effect on the central nervous system. The hypotensive effect stabilizes by the end of 2 weeks of the course.
The antianginal effect is due to a decrease in myocardial oxygen demand (due to the negative chronotropic and inotropic effect). A decrease in heart rate leads to prolongation of diastole and improved myocardial perfusion.
By increasing end-diastolic pressure in the left ventricle and increasing the stretch of ventricular muscle fibers, it can increase oxygen demand, especially in patients with chronic heart failure.
The antiarrhythmic effect is due to the elimination of arrhythmogenic factors (tachycardia, increased activity of the sympathetic nervous system, increased cAMP content, arterial hypertension), a decrease in the rate of spontaneous excitation of sinus and ectopic pacemakers and a slowdown of atrioventricular conduction.
Inhibition of impulse conduction is observed predominantly in the antegrade and to a lesser extent in the retrograde directions through the atrioventricular node and along additional pathways. According to the classification of antiarrhythmic drugs, it belongs to group II drugs.
Reducing the severity of myocardial ischemia – by reducing myocardial oxygen demand, post-infarction mortality can also be reduced due to the antiarrhythmic effect.
The ability to prevent the development of headaches of vascular origin is due to a decrease in the severity of dilation of cerebral arteries due to beta-blockade of vascular receptors, inhibition of platelet aggregation and lipolysis caused by catecholamines, a decrease in platelet adhesiveness, prevention of activation of blood coagulation factors during the release of adrenaline, stimulation of oxygen supply to tissues and a decrease in renin secretion.
The reduction in tremor with the use of propranolol may be due to the blockade of beta2-adrenergic receptors. Increases the atherogenic properties of blood. Strengthens uterine contractions (spontaneous and caused by drugs that stimulate the myometrium). Increases bronchial tone.
Pharmacokinetics
It is quickly and fairly completely (90%) absorbed when taken orally and is relatively quickly eliminated from the body. Bioavailability after oral administration – 30-40% (first pass effect through the liver,
microsomal oxidation), with prolonged use – increases (metabolites are formed that inhibit liver enzymes), its value depends on the nature of the food and the intensity of hepatic blood flow.
Metabolized by glucuronidation in the liver. The maximum concentration in blood plasma is achieved after 1-1.5 hours. It is highly lipophilic and accumulates in lung tissue, brain, kidneys, and heart. Penetrates through the blood-brain and placental barriers into breast milk. Communication with blood plasma proteins is 90-95%. Volume of distribution: 3-5 l/kg.
It enters the intestine with bile, is deglucuronidated and reabsorbed. The half-life is 3-5 hours, during a course of administration it can be extended to 12 hours. Excreted by the kidneys is 90%, unchanged – less than 1%. It is not removed by hemodialysis.
Special instructions
Special instructions
Monitoring of patients taking the drug should include monitoring heart rate and blood pressure (daily at the beginning of treatment, then once every 3-4 months), recording an electrocardiogram.
In elderly patients, it is recommended to monitor renal function (once every 4-5 months).
If elderly patients develop increasing bradycardia (less than 50 beats/min), arterial hypotension (systolic blood pressure less than 100 mm Hg), atrioventricular block, bronchospasm, ventricular arrhythmias, severe impairment of liver and/or kidney function, it is necessary to reduce the dose of the drug or discontinue treatment.
The patient should be taught how to calculate heart rate and instructed to seek medical advice if the heart rate is less than 50 beats/min.
It is recommended to discontinue therapy if depression caused by taking beta-blockers develops.
Patients using contact lenses should take into account that during treatment there may be a decrease in the production of tear fluid.
Before prescribing the drug to patients with heart failure (early stages), it is necessary to use cardiac glycosides and/or diuretics.
Treatment of coronary heart disease and persistent arterial hypertension should be long-term – taking the drug is possible for several years.
Discontinuation of treatment is carried out gradually, under the supervision of a physician: abrupt withdrawal can dramatically increase myocardial ischemia, anginal syndrome, and worsen exercise tolerance. Cancellation is carried out gradually, reducing the dose by 25% every 3-4 days for 2 weeks or more.
In case of thyrotoxicosis, the drug may mask certain clinical signs of hyperthyroidism (for example, tachycardia). Abrupt withdrawal in patients with thyrotoxicosis is contraindicated as it can increase symptoms.
In patients suffering from diabetes, the drug is used under the control of blood glucose concentration (once every 4-5 months).
Prescribe with caution in combination with hypoglycemic agents, since hypoglycemia may develop during long breaks in food intake, as well as during insulin therapy. Moreover, its symptoms such as tachycardia or tremor will be masked due to the action of the drug.
The patient should be instructed that the main symptom of hypoglycemia during treatment with the drug is increased sweating. There is also a risk of hyperglycemia when taking oral hypoglycemic agents.
When taking clonidine concomitantly, it can be discontinued only a few days after discontinuation of the drug.
For pheochromocytoma, it is prescribed only in combination with alpha-blockers.
Concomitant use with antipsychotic drugs (neuroleptics) and tranquilizers is contraindicated.
Drugs that reduce catecholamine reserves (for example, reserpine) may enhance the effect of propranolol, so patients taking combinations of drugs should be under constant medical supervision to detect arterial hypotension and bradycardia.
During treatment, intravenous administration of verapamil and diltiazem should be avoided.
Use with caution in combination with psychotropic drugs, for example, monoamine oxidase inhibitors, when they are used in a course of more than 2 weeks.
A few days before general anesthesia with chloroform or ether, it is necessary to stop taking the drug (increased risk of depression of function
myocardium and the development of arterial hypotension).
In smokers, the effectiveness of the drug is reduced.
The drug should be discontinued before testing the content of catecholamines, normetanephrine and vanillinmandelic acid in the blood and urine, and titers of antinuclear antibodies.
During treatment, it is not recommended to take alcohol (ethanol) – a sharp decrease in blood pressure is possible.
Natural licorice should be avoided: foods rich in protein may increase bioavailability.
Impact on the ability to drive vehicles and other mechanisms
During the treatment period, it is necessary to refrain from driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Propranolol
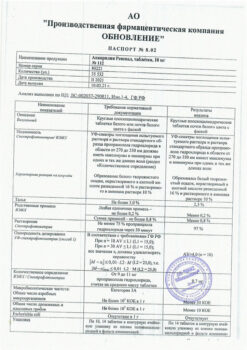
Composition
Composition
For one tablet
Active substance
Propranolol hydrochloride (anaprilin) - 40 mg
Excipients – to obtain a tablet weighing – 200 mg
sucrose (sugar) − 108 mg
potato starch – 45 mg
calcium stearate − 2 mg
talc – 5 mg
Pregnancy
Pregnancy
The use of the drug during pregnancy is possible only if the benefit to the mother outweighs the risk of side effects in the fetus and child, and careful monitoring of the fetus’s condition is necessary. The drug should be discontinued 48-72 hours before birth.
Possible effect on the fetus: intrauterine growth restriction,
hypoglycemia, bradycardia. Propranolol is excreted in breast milk. If necessary, use
of the drug during lactation, breastfeeding should be stopped.
Contraindications
Contraindications
Hypersensitivity to the drug, atrioventricular block II-III degree, sinoauricular block, sinus bradycardia, arterial hypotension, uncontrolled chronic heart failure IIB-III degree, acute heart failure, acute myocardial infarction (systolic blood pressure less than 100 mm Hg), cardiogenic shock, pulmonary edema, sick sinus syndrome, Prinzmetal’s angina, cardiomegaly (without signs of heart failure), vasomotor rhinitis, occlusive diseases of peripheral vessels, diabetes mellitus, metabolic acidosis (including diabetic ketoacidosis), bronchial asthma, a tendency to bronchospastic reactions, chronic obstructive pulmonary disease (including a history), pheochromocytoma (without simultaneous use of alpha-blockers), spastic colitis, concomitant use with antipsychotics and anxiolytics (chlorpromazine, trioxazine, etc.), monoamine oxidase inhibitors, lactation period, age up to 18 years (efficacy and safety have not been established).
With caution
Hepatic and/or renal failure, hyperthyroidism, myasthenia gravis, heart failure, pheochromocytoma, psoriasis, pregnancy, history of allergic reactions, Raynaud’s syndrome, old age.
Side Effects
Side Effects
From the cardiovascular system: sinus bradycardia, atrioventricular block, heart failure, palpitations, myocardial conduction disturbances, arrhythmias, decreased blood pressure, orthostatic hypotension, chest pain, spasm of peripheral arteries, cold extremities, mesenteric thrombosis.
From the digestive system: dryness of the oral mucosa, nausea, vomiting, diarrhea, constipation, pain in the epigastric region, impaired liver function, changes in taste, ischemic colitis.
From the nervous system: headache, insomnia, “nightmarish” dreams, asthenic syndrome, agitation, depression, paresthesia, increased fatigue, weakness, dizziness, drowsiness, confusion or short-term memory loss, hallucinations, tremor, catatonia, emotional lability, decreased speed of psychomotor reactions.
From the respiratory system: rhinitis, nasal congestion, shortness of breath, bronchospasm, laryngospasm.
Metabolism: hypoglycemia (in patients with type 1 diabetes mellitus), hyperglycemia (in patients with type 2 diabetes mellitus).
From the senses: dryness of the mucous membrane of the eyes (decreased secretion of tear fluid), impaired visual acuity, keratoconjunctivitis.
From the reproductive system: decreased libido, decreased potency, Peyronie’s disease.
From the skin: alopecia, exacerbation of psoriasis, increased sweating, skin hyperemia, exanthema, psoriasis-like skin reactions, Stevens-Johnson syndrome, toxic epidermal necrolysis, exfoliative dermatitis, erythema multiforme.
From the endocrine system: decreased thyroid function.
Allergic reactions: skin rash, itching.
Laboratory indicators: agranulocytosis, increased activity of “liver” transaminases and bilirubin concentration.
Other: muscle weakness, back or joint pain, chest pain, leukopenia, thrombocytopenia, withdrawal syndrome.
During post-marketing use, cases of gingival hyperplasia have been reported with the use of propranolol. There are no data on the incidence of this adverse reaction.
Interaction
Interaction
The hypotensive effect of propranolol is enhanced when combined with diuretics, reserpine, hydralazine and other antihypertensive drugs, as well as ethanol.
The hypotensive effect is weakened by non-steroidal anti-inflammatory drugs (sodium retention and blocking renal prostaglandin synthesis), estrogens (sodium retention) and monoamine oxidase inhibitors.
Cimetidine increases bioavailability.
Increases the concentration of lidocaine in the blood plasma, reduces the clearance of theophylline.
Co-administration with phenothiazine derivatives increases the concentrations of both drugs in the blood plasma.
Enhances the effect of thyreostatic and uterotonic drugs; reduces the effect of antihistamines.
Increases the likelihood of developing severe systemic reactions (anaphylaxis) due to the introduction of allergens used for immunotherapy or for skin testing.
Amiodarone, verapamil and diltiazem – increased severity of the negative chrono-, ino- and dromotropic effects of propranolol.
Iodine-containing radiocontrast drugs for intravenous administration increase the risk of anaphylactic reactions.
Phenytoin, when administered intravenously, and drugs for inhalation general anesthesia (hydrocarbon derivatives) increase the severity of the cardiodepressive effect and the likelihood of lowering blood pressure.
Changes the effectiveness of insulin and oral hypoglycemic drugs, masks the symptoms of developing hypoglycemia (tachycardia, increased blood pressure).
Reduces the clearance of xanthines (except difillin).
The hypotensive effect is weakened by glucocorticosteroids.
Cardiac glycosides, methyldopa, reserpine and guanfacine, antiarrhythmic drugs increase the risk of developing or worsening bradycardia, atrioventricular block, cardiac arrest and heart failure.
Nifedipine can lead to a significant decrease in blood pressure.
Prolongs the effect of non-depolarizing muscle relaxants and the anticoagulant effect of coumarins.
Tri- and tetracyclic antidepressants, antipsychotic drugs (neuroleptics), ethanol, sedatives and hypnotics increase depression of the central nervous system.
Concomitant use with monoamine oxidase inhibitors is not recommended due to a significant increase in the hypotensive effect; the break in treatment between taking monoamine oxidase inhibitors and propranolol should be at least 14 days.
Non-hydrogenated ergot alkaloids increase the risk of developing peripheral circulatory disorders.
Sulfasalazine increases concentration
propranolol in the blood plasma (inhibits metabolism), rifampicin shortens
half-life.
Overdose
Overdose
Symptoms: bradycardia, dizziness or fainting, decreased blood pressure, arrhythmias, difficulty breathing, cyanosis of fingernails or palms, or convulsions.
Treatment: gastric lavage, administration of activated charcoal, if atrioventricular conduction is impaired, 1-2 mg of atropine, epinephrine are administered intravenously, if efficiency is low, a temporary pacemaker is installed; for ventricular extrasystole – lidocaine (class IA drugs are not used); in case of arterial hypotension, the patient should be in the Trendelenburg position.
If there are no signs of pulmonary edema, plasma-substituting solutions are administered intravenously; if ineffective, epinephrine, dopamine, dobutamine; for convulsions – intravenous diazepam; for bronchospasm, inhaled or parenterally – beta-adrenergic stimulants.
Storage conditions
Storage conditions
Store in a dry place, protected from light.
Shelf life
Shelf life
4 years.
Manufacturer
Manufacturer
Update of PFC JSC, Russia
Additional information
| Shelf life | 4 years. |
|---|---|
| Conditions of storage | Store in a dry place protected from light. |
| Manufacturer | Update PFC AO, Russia |
| Medication form | pills |
| Brand | Update PFC AO |
Other forms…
Related products
Buy Anapriline Reneval, tablets 40 mg 112 pcs with delivery to USA, UK, Europe and over 120 other countries.