No products in the cart.
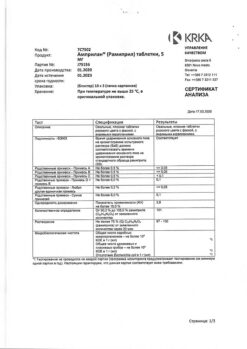
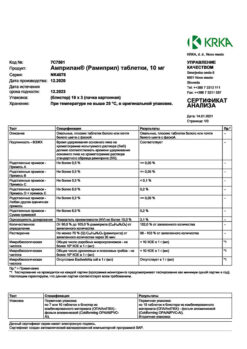
Amprilan, tablets 1,25mg 30 pcs
€11.03 €9.65
Description
ACE catalyzes the conversion of angiotensin I to angiotensin II. ACE is identical to kininase, the enzyme that catalyzes the breakdown of bradykinin. ACE blockade leads to a decrease in the concentration of angiotensin II, increased plasma renin activity, increased bradykinin effect and increased aldosterone secretion, which may cause increased serum potassium levels.
The antihypertensive and hemodynamic effects of ramipril in patients with arterial hypertension are the result of vasodilation and reduction of OPPS, which in turn gradually reduces BP. Cardiac rhythm usually does not change. Long-term therapy reduces left ventricular hypertrophy without adverse effects on cardiac function. The antihypertensive effect after a single oral dose of the drug is evident in 1-2 hours, reaches a maximum in 3-6 hours and lasts for 24 hours.
Ramipril is effective in the treatment of CHF. In patients with signs of CHF after myocardial infarction, ramipril reduces risk of sudden death, progression of heart failure and decreases number of hospitalizations for exacerbation of CHF. Both in patients with and without diabetes mellitus, the drug significantly reduces the existing microalbuminuria and the risk of nephropathy. These effects are noted in patients with both elevated and normal BP.
Indications
Indications
Arterial hypertension.
Chronic heart failure (as part of combination therapy), incl. developed on days 2–9 after myocardial infarction.
Diabetic nephropathy and nephropathy against the background of chronic diffuse kidney diseases (preclinical and clinical stages), incl. chronic glomerulonephritis with severe proteinuria.
Reducing the risk of myocardial infarction, stroke and cardiovascular mortality in patients at high cardiovascular risk, including patients with confirmed coronary artery disease (with or without a history of myocardial infarction), patients who have undergone percutaneous transluminal coronary angioplasty, coronary artery bypass grafting, with a history of stroke and patients with occlusive lesions of peripheral arteries.
Pharmacological effect
Pharmacological effect
ACE catalyzes the conversion of angiotensin I to angiotensin II. ACE is identical to kininase, an enzyme that catalyzes the breakdown of bradykinin. ACE blockade leads to a decrease in the concentration of angiotensin II, an increase in renin activity in the blood plasma, an increase in the effect of bradykinin and an increase in the secretion of aldosterone, which may cause an increase in the level of potassium in the blood serum.
The antihypertensive and hemodynamic effects of ramipril in patients with arterial hypertension are the result of vasodilation and a decrease in peripheral vascular resistance, which in turn gradually reduces blood pressure. Heart rate usually does not change. With long-term therapy, left ventricular hypertrophy decreases without adversely affecting cardiac function. The antihypertensive effect after taking one dose of the drug orally appears after 1–2 hours, reaches a maximum after 3–6 hours and persists for 24 hours.
Ramipril is effective in the treatment of CHF. In patients with signs of CHF after myocardial infarction, ramipril reduces the risk of sudden death, progression of heart failure and reduces the number of hospitalizations for exacerbation of CHF. In both patients with and without diabetes mellitus, the drug significantly reduces existing microalbuminuria and the risk of developing nephropathy. These effects are observed in patients with both high and normal blood pressure.
Special instructions
Special instructions
At the beginning of treatment, renal function should be assessed. Renal function should be carefully monitored in patients with impaired renal function, heart failure, bilateral renal artery stenosis or arterial stenosis of a solitary kidney, as well as in patients after kidney transplantation.
Liver failure
In rare cases, during the use of ACE inhibitors, cholestatic jaundice occurs, with the progression of which fulminant liver necrosis develops, sometimes with a fatal outcome. If jaundice appears or a significant increase in the activity of liver transaminases while taking ACE inhibitors, the use of Amprilan® should be discontinued.
In patients with uncomplicated arterial hypertension, symptomatic arterial hypotension rarely develops after taking the first dose of the drug. The risk of developing arterial hypotension is increased in the following patients:
With severe CHF: treatment begins with the lowest possible dose of Amprilan® (1.25 mg).
Those taking diuretics: if possible, it is necessary to cancel the diuretic in advance or reduce its dose; treatment begins with a minimum dose of Amprilan® (1.25 mg).
With the risk of developing hypovolemia due to insufficient fluid intake, diarrhea, vomiting, or increased sweating in conditions of insufficient compensation for salt and fluid loss. It is usually recommended to adjust the blood volume before starting treatment, but if these conditions become clinically significant, treatment with Amprilan® can be started and/or continued with a minimum dose (1.25 mg) and under medical supervision.
Aortic stenosis/mitral stenosis/HOCM
ACE inhibitors should be used with caution in patients with left ventricular outflow tract obstruction and aortic and/or mitral stenosis.
Neutropenia/agranulocytosis
In patients taking ACE inhibitors, cases of neutropenia/agranulocytosis, thrombocytopenia and anemia may develop. In patients with normal renal function in the absence of other complications, neutropenia rarely develops and resolves spontaneously after discontinuation of ACE inhibitors.
Ramipril should be used with great caution in patients with connective tissue diseases and simultaneously receiving immunosuppressive therapy, allopurinol or procainamide, especially with existing renal impairment. These patients may develop severe infections that do not respond to intensive antibiotic therapy. When using ramipril, it is recommended to periodically monitor the number of leukocytes in the blood. The patient should be warned that if any signs of an infectious disease appear (sore throat, fever), consult a doctor immediately.
Hyperkalemia
May develop during treatment with ACE inhibitors, incl. and ramipril. Risk factors for hyperkalemia are renal failure, old age, diabetes mellitus, some concomitant conditions (decrease in blood volume, acute heart failure in the stage of decompensation, metabolic acidosis), simultaneous use of potassium-sparing diuretics (such as spironolactone, eplerenone, triamterene, amiloride), as well as potassium preparations or potassium-containing substitutes for table salt and the use of other drugs that increase the level of potassium in the blood plasma (for example, heparin). Hyperkalemia can cause serious heart rhythm problems, sometimes fatal.
Potassium-sparing diuretics and potassium supplements
The combined use of Amprilan® and potassium-sparing diuretics, as well as potassium preparations and potassium-containing table salt substitutes is not recommended.
Surgery/general anesthesia
The use of ACE inhibitors in patients undergoing surgery under general anesthesia can lead to a significant decrease in blood pressure, especially when using general anesthesia agents that have a hypotensive effect.
It is recommended to stop taking ACE inhibitors, incl. ramipril, 12 hours before surgery, warning the anesthesiologist about the use of ACE inhibitors.
Cough
During therapy with an ACE inhibitor, a dry cough may occur, which disappears after discontinuation of drugs in this group. If a dry cough appears, you should be aware of the possible connection of this symptom with taking an ACE inhibitor.
Anaphylactoid reactions during desensitization procedures
There are isolated reports of the development of long-term, life-threatening anaphylactoid reactions in patients receiving ACE inhibitors during desensitizing therapy with the venom of hymenoptera insects (bees, wasps). ACE inhibitors should be used with caution in patients prone to allergic reactions undergoing desensitization procedures. Prescription of an ACE inhibitor should be avoided in patients receiving immunotherapy with hymenoptera venom. However, the development of anaphylactoid reactions can be avoided by temporarily discontinuing the ACE inhibitor at least 24 hours before the start of the desensitization procedure.
Anaphylactoid reactions during LDL apheresis
In rare cases, life-threatening anaphylactoid reactions may occur in patients receiving ACE inhibitors during LDL apheresis using dextran sulfate. To prevent an anaphylactoid reaction, ACE inhibitor therapy should be discontinued before each LDL apheresis procedure using high-flux membranes.
Hemodialysis
Anaphylactoid reactions have been reported in patients receiving ACE inhibitors during hemodialysis using high-flux membranes (eg AN69®). Therefore, it is advisable to use a different type of membrane or use an antihypertensive drug of a different pharmacotherapeutic group.
Impact on the ability to drive a car or perform work that requires increased speed of physical and mental reactions
During the treatment period, care must be taken when engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions, because Dizziness, drowsiness, confusion and other side effects are possible.
Active ingredient
Active ingredient
Ramipril
Composition
Composition
Active substance:
Ramipril – 1.25 mg.
Excipients:
Sodium bicarbonate – 10 mg;
Lactose monohydrate – 193.2 mg;
Croscarmellose sodium – 5.2 mg;
Pregelatinized starch – 39 mg;
Sodium stearyl fumarate – 2.6 mg.
Contraindications
Contraindications
Hypersensitivity to ramipril and any other component of the drug or other ACE inhibitors.
History of angioedema (hereditary, idiopathic or angioedema due to taking ACE inhibitors).
Hemodynamically significant bilateral renal artery stenosis.
Stenosis of the artery of a single kidney.
Condition after kidney transplantation.
Hemodialysis.
Renal failure (Cl creatinine
Hemodynamically significant aortic and/or mitral stenosis (risk of excessive reduction in blood pressure with subsequent impaired renal function).
Hypertrophic obstructive cardiomyopathy (HOCM).
Chronic heart failure in the stage of decompensation.
Severe arterial hypotension (BP less than 90 mm Hg) or unstable hemodynamics.
Primary hyperaldosteronism.
Galactose intolerance, lactase deficiency or glucose-galactose malabsorption syndrome.
Nephropathy, treated with corticosteroids, NSAIDs, immunomodulators and/or cytostatics.
Pregnancy.
Lactation period.
Age up to 18 years (efficacy and safety have not been established).
With caution:
Severe damage to the coronary and cerebral arteries (danger of decreased blood flow with an excessive decrease in blood pressure);
Malignant arterial hypertension;
Unstable angina;
Aortic and/or mitral stenosis;
Severe ventricular arrhythmias;
Chronic heart failure (IV functional class according to the NYHA classification);
Decompensated cor pulmonale;
Renal and/or liver failure;
Hyperkalemia;
Hyponatremia (including against the background of diuretics and a diet with limited salt intake);
Conditions accompanied by a decrease in blood volume, incl. diarrhea, vomiting;
Systemic connective tissue diseases;
Diabetes mellitus;
Inhibition of bone marrow hematopoiesis;
Old age;
Hemodialysis using high-flow polyacrylonitrile membranes – the risk of developing anaphylactoid reactions;
Before the LDL apheresis procedure;
Simultaneous desensitizing therapy with allergens (for example, hymenoptera venom).
Side Effects
Side Effects
Classification of the frequency of side effects (WHO):
Very often – ≥1/10.
Often – from ≥1/100 to
Uncommon – from ≥1/1000 to <1/100.
Rarely - from ≥1/10000 to <1/1000.
Very rare - from <1/10000, including individual reports.
From the cardiovascular system: often – a pronounced decrease in blood pressure (at the beginning of therapy, when increasing the dose or adding a diuretic to therapy), orthostatic hypotension, syncope; rarely – peripheral edema, palpitations, angina pectoris, arrhythmia; very rarely – myocardial ischemia, myocardial infarction, increased circulatory disorders against the background of stenotic vascular lesions, Raynaud’s syndrome, vasculitis, tachycardia, flushing of the facial skin.
From the nervous system: often – headache, weakness; rarely – increased fatigue, nervousness, depression, tremor, imbalance, confusion, anxiety, dizziness, restlessness, sleep disorder; very rarely – paresthesia, impaired smell perception (parosmia), transient ischemic attacks, ischemic stroke, cerebral ischemia, impaired concentration.
From the genitourinary system: rarely – transient impotence, decreased libido, impaired renal function, up to acute renal failure, increased urine output, increased pre-existing proteinuria, increased concentrations of urea and creatinine; very rarely – gynecomastia.
From the respiratory system: often – dry non-productive cough, worse at night and when lying down, more often occurring in women and non-smoking patients, sinusitis, bronchitis, shortness of breath; rarely – nasal congestion, pharyngitis, bronchospasm, including aggravation of bronchial asthma.
From the skin: often – maculopapular skin rash; rarely – skin itching, increased sweating (against the background of decreased blood pressure); very rarely – maculopapular exanthema and erythema, pemphigus, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, worsening of psoriasis, psoriasiform, pemphigoid and lichenoid lesions of the skin and mucous membranes, alopecia; very rarely – urticaria, onycholysis, exfoliative dermatitis, photosensitivity.
From the digestive system: often – inflammation of the gastrointestinal mucosa, indigestion, abdominal discomfort, dyspepsia, nausea, diarrhea, vomiting; rarely – increased activity of liver enzymes, increased bilirubin concentration, cholestatic jaundice, acute liver failure, cholestatic hepatitis, hepatocellular lesions, dry oral mucosa, abdominal pain, gastritis, constipation, pancreatitis, incl. and with a fatal outcome (cases of pancreatitis with a fatal outcome when taking ACE inhibitors were extremely rare), intestinal angioedema, loss of appetite, anorexia; very rarely – glossitis; aphthous stomatitis.
From the musculoskeletal system: often – myalgia, muscle cramps; rarely – arthralgia.
From the senses: rarely – visual disturbances, including blurred vision, conjunctivitis, hearing impairment, disturbances of smell and taste (for example, metallic taste, partial or temporary loss of taste).
Allergic reactions: very rarely – angioedema with involvement of the mucous membrane of the lips, eyes, tongue, larynx and pharynx, anaphylactic or anaphylactoid reactions (insect poisons), increased concentration of antinuclear bodies.
Laboratory indicators: rarely – hyperkalemia, moderate (sometimes severe) hypohemoglobinemia or neutropenia, erythropenia and thrombocytopenia, increased activity of pancreatic enzymes; very rarely – hyponatremia, proteinuria (although usually ACE inhibitors reduce previous proteinuria) or increased diuresis (in combination with deterioration of cardiac function), agranulocytosis, pancytopenia, bone marrow depression, hemolytic anemia.
Other: rarely – hyperthermia; very rarely – fever.
Interaction
Interaction
Vasopressor sympathomimetics (epinephrine, norepinephrine) may reduce the hypotensive effect of ramipril. When these drugs are used concomitantly, blood pressure levels should be carefully monitored.
ACE inhibitors enhance the inhibitory effect of ethanol on the central nervous system.
Lithium preparations: with simultaneous use of lithium preparations and ACE inhibitors, cases of reversible increases in the concentration of lithium in the blood serum have been reported. Concomitant use with thiazide diuretics may increase lithium concentrations and the risk of its toxic effects while taking an ACE inhibitor.
NSAIDs: combination of ACE inhibitors with NSAIDs (non-selective inhibitors of COX-1 and COX-2 from the NSAID group, for example acetylsalicylic acid in doses that have an anti-inflammatory effect): the hypotensive effect of ACE inhibitors is reduced; the risk of renal dysfunction increases, up to the development of acute renal failure; serum potassium levels increase in patients with pre-existing renal impairment.
Tricyclic antidepressants, antipsychotics (neuroleptics): enhance the hypotensive effect and increase the risk of orthostatic hypotension (additive effect).
GCS, tetracosactide: decreased hypotensive effect (fluid retention).
Potassium-sparing diuretics (spironolactone, triamterene, amiloride, eplerenone) and potassium preparations: the combined use of ramipril and potassium-sparing diuretics, as well as potassium preparations and potassium-containing table salt substitutes is not recommended.
Caution should be exercised and regular monitoring of potassium levels in the blood plasma and ECG parameters should be carried out.
Oral hypoglycemic agents (sulfonylureas) and insulin: the use of ACE inhibitors may enhance the hypoglycemic effect of oral hypoglycemic agents and insulin in patients with diabetes mellitus; when used together, it is possible to increase glucose tolerance, which may require dose adjustment of oral hypoglycemic agents and insulin.
Allopurinol, cytostatic drugs, immunosuppressants, corticosteroids (for systemic use) and procainamide: simultaneous use of these drugs with ACE inhibitors may increase the risk of developing leukopenia.
General anesthetics: ACE inhibitors may enhance the hypotensive effect of some general anesthetics.
Gold preparations: when prescribing ACE inhibitors, incl. ramipril, patients receiving the gold drug (sodium aurothiomalate) intravenously were noted to have nitrate-like reactions (nausea, vomiting, marked decrease in blood pressure, facial skin flushing).
Overdose
Overdose
Symptoms: marked decrease in blood pressure, bradycardia, shock, water and electrolyte imbalance, acute renal failure, stupor.
Treatment: in mild cases of overdose – gastric lavage, administration of adsorbents and sodium picosulfate (preferably within 30 minutes after ingestion). With a pronounced decrease in blood pressure – intravenous administration of catecholamines, alpha1-adrenergic agonists (norepinephrine, dopamine), angiotensin II (angiotensinamide), the patient should be laid on his back on a surface with a low head, if necessary, the volume of blood volume can be replenished by infusion of 0.9% sodium chloride solution; In case of bradycardia, a temporary artificial pacemaker can be installed. It is necessary to carefully monitor blood pressure, renal function and serum potassium levels. The effectiveness of hemodialysis has not been established.
Storage conditions
Storage conditions
At a temperature not exceeding 25 ° C. Keep out of the reach of children.
Manufacturer
Manufacturer
KRKA dd Novo Mesto, Slovenia
Additional information
| Conditions of storage | At a temperature not higher than 25 ° C. Keep out of reach of children. |
|---|---|
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | pills |
| Brand | KRKA dd Novo mesto |
Other forms…
Related products
Buy Amprilan, tablets 1,25mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.