No products in the cart.
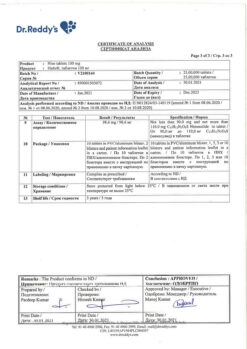
Aertal, 3 g 20 pcs.
€19.88 €16.57
Description
Pharmgroup:
NSAIDs.
Pharmic action:
Aertal is an NSAID. It has anti-inflammatory, analgesic and antipyretic effects. Inhibits the synthesis of prostaglandins and thus affects the pathogenesis of inflammation, pain and fever.
In rheumatic diseases the anti-inflammatory and analgesic effect of aceclofenac helps to significantly reduce the severity of pain, stiffness in the morning and swollen joints and improves the functional state of the patient.
Pharmacokinetics:
Absorption
Quickly and completely absorbed after oral administration. Cmax in plasma after oral administration is reached after 1.25-3 hours.
Distribution
Binding to plasma albumin is 99%.
It penetrates into the synovial fluid where its concentration reaches 57% of the plasma concentration level and Cmax is reached 2-4 hours later than in plasma. Vd is 25 liters.
Metabolism
It is metabolized to a small extent. Its main metabolite found in plasma is 4′-hydroxyacetylophenac.
Elimation
T1/2 – 4 hours. It is excreted by the kidneys mainly as hydroxy derivatives (about 2/3 of the administered dose).
Indications
Indications
Relief of inflammation and pain in:
– lumbago;
– toothache;
— humeroscapular periarthritis;
— rheumatic lesions of soft tissues.
Symptomatic treatment:
— rheumatoid arthritis;
— osteoarthritis;
– ankylosing spondylitis.
Pharmacological effect
Pharmacological effect
Pharmaceutical group:
NSAIDs.
Pharmaceutical action:
Airtal is an NSAID. It has anti-inflammatory, analgesic and antipyretic effects. Inhibits the synthesis of prostaglandins and, thus, affects the pathogenesis of inflammation, pain and fever.
In rheumatic diseases, the anti-inflammatory and analgesic effect of aceclofenac helps to significantly reduce the severity of pain, morning stiffness, and swelling of the joints, which improves the patient’s functional condition.
Pharmacokinetics:
Suction
Quickly and completely absorbed after oral administration. Cmax in plasma after oral administration is achieved within 1.25-3 hours.
Distribution
Binding to plasma albumin is 99%.
Penetrates into the synovial fluid, where its concentration reaches 57% of the plasma concentration level and Cmax is reached 2-4 hours later than in blood plasma. Vd – 25 l.
Metabolism
Metabolized to a small extent. Its main metabolite found in plasma is 4′-hydroxyaceclofenac.
Removal
T1/2 – 4 hours. Excreted by the kidneys mainly in the form of hydroxy derivatives (about 2/3 of the administered dose).
Special instructions
Special instructions
Avoid using Airtal® concomitantly with other NSAIDs, including selective cyclooxygenase-2 inhibitors.
Adverse events can be reduced by shortening the duration of treatment as much as possible and reducing the dose of the drug to the minimum necessary to achieve control of the symptoms of the disease.
Effect on the gastrointestinal tract.
Aceclofenac should be prescribed with caution and under close medical supervision to patients with the diseases listed below, as their course may worsen:
– symptoms indicating gastrointestinal diseases, including the upper and lower gastrointestinal tract;
– a history of ulcer, bleeding or perforation of a stomach or intestinal ulcer in the presence of Helicobacter pylori infection;
– history of ulcerative colitis;
– history of Crohn’s disease;
– hematological diseases, systemic lupus erythematosus (SLE), porphyria and hematopoietic disorders.
There have been reports of gastrointestinal bleeding, gastric or intestinal ulceration or perforation of the ulcer, which can lead to death when taking any NSAID at any time during treatment, with or without alarming symptoms, regardless of a history of serious gastrointestinal complications.
The risk of gastrointestinal bleeding, ulceration, or ulcer perforation is greater when treated with high doses of NSAIDs in patients with a history of gastric or intestinal ulcers, especially if complicated by bleeding or perforation, and in elderly patients. Treatment of these patients should begin with the lowest effective dose. Also, when treating these groups of patients and patients who require concomitant use of acetylsalicylic acid in low doses or other drugs that may increase the risk of gastrointestinal complications, the need for combination therapy with protective drugs (for example, misoprostol or proton pump inhibitors) should be considered.
Patients with a history of gastrointestinal disease, especially the elderly, should report any unusual abdominal symptoms (especially gastrointestinal bleeding), paying maximum attention to symptoms early in treatment. Caution should be exercised when treating patients receiving concomitant medications that may increase the risk of ulceration or bleeding, such as systemic corticosteroids, anticoagulants such as warfarin, selective serotonin reuptake inhibitors, or antiplatelet drugs such as acetylsalicylic acid.
If gastrointestinal bleeding or ulceration occurs in patients taking Airtal®, treatment should be discontinued.
Effect on the cardiovascular system and cerebral circulation.
When treating patients with arterial hypertension and/or chronic heart failure, appropriate monitoring and recommendations should be provided, as there are reports of the development of fluid retention and edema during treatment with NSAIDs.
There is evidence to suggest that some NSAIDs (especially in high doses and in long-term treatment) may increase the risk of arterial thrombotic complications (eg, myocardial infarction or stroke). There is insufficient data to exclude this risk when using aceclofenac.
Patients with uncontrolled arterial hypertension, congestive heart failure, established coronary artery disease, peripheral arterial disease and/or cerebrovascular disease should begin treatment with aceclofenac only after an informed decision by the attending physician. Likewise, the indications for long-term treatment in patients with risk factors for cardiovascular disease (eg, hypertension, hyperlipidemia, diabetes mellitus, and smoking) should be carefully assessed before initiation.
Caution and close medical supervision should also be exercised when using aceclofenac in patients with a history of cerebral hemorrhage.
Effect on the liver and kidneys.
Treatment with NSAIDs may cause a dose-dependent decrease in prostaglandin synthesis and precipitate renal failure. The importance of prostaglandins in maintaining renal blood flow in patients with impaired cardiac or renal function, liver dysfunction, patients receiving diuretic treatment or recovering from abdominal surgery, and elderly patients should be taken into account.
Caution should be exercised when treating patients with impaired liver or kidney function, as well as patients with other diseases predisposing to fluid retention. In these patients, treatment with NSAIDs may lead to impaired renal function and fluid retention. Caution must also be exercised when using the drug in patients receiving diuretic treatment or, conversely, in patients at risk of hypovolemia. The minimum effective dose should be prescribed and renal function should be regularly monitored. The effect of the drug on renal function is usually reversible after discontinuation of aceclofenac.
Treatment with aceclofenac should be discontinued if deviations from normal liver function tests persist or increase, clinical symptoms consistent with the development of liver failure appear, or other manifestations (eg, eosinophilia, rash) appear.
Hepatitis can develop without previous symptoms.
In patients with hepatic porphyria, the use of NSAIDs may provoke an exacerbation of the disease.
Hypersensitivity and skin reactions.
As with the use of other NSAIDs, allergic reactions, including diaphylactic/anaphylactoid reactions, may occur already in the early stages of drug use. In very rare cases, serious skin reactions have been observed with the use of NSAIDs, including exfoliative dermatitis, Stevens-Johnson syndrome and toxic epidermal necrolysis, some of which can lead to death. Patients are at highest risk of developing these reactions early in treatment, with most reactions occurring within the first month of treatment. At the first sign of skin rash, damage to the mucous membranes or any other symptoms of hypersensitivity, treatment with Airtal® should be discontinued.
In extremely rare cases, chickenpox can cause serious infectious complications of the skin and soft tissues. At the moment, the role of NSAIDs in worsening the course of these infectious complications cannot be excluded. Therefore, it is recommended to avoid the use of Airtal® for chickenpox.
Effect on hematological parameters.
Aceclofenac can reversibly inhibit platelet aggregation.
Respiratory system disorders.
Caution should be exercised when using the drug in patients with bronchial asthma or with a history of bronchial asthma, as there are reports that NSAIDs may cause bronchospasm in such patients.
Elderly patients.
Caution should be exercised when treating elderly patients, as in this age group the incidence of adverse events associated with NSAID treatment is increased, especially gastrointestinal bleeding and ulcer perforation, which can lead to death. In addition, elderly patients are more susceptible to renal, hepatic or cardiovascular failure.
Long-term treatment.
It is necessary to carefully monitor all patients receiving long-term treatment with NSAIDs, regularly performing complete blood count, liver and kidney function tests.
Each sachet of Airtal®, powder for oral suspension, 100 mg, contains 2.64 g of sorbitol, which can cause gastrointestinal disorders and diarrhea. Patients with rare hereditary fructose intolerance should not be prescribed this drug.
Airtal®, powder for oral suspension, 100 mg, contains aspartame, a source of phenylalanine. Patients with phenylketonuria should note that each sachet contains 5.61 mg of phenylalanine.
Impact on the ability to drive vehicles and operate machinery.
You should refrain from driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions, as the drug may cause dizziness and other side effects that may affect these abilities.
Active ingredient
Active ingredient
Aceclofenac
Composition
Composition
1 pack:
– aceclofenac 100 mg
Excipients:
sorbitol – 2.639 g,
sodium saccharinate – 0.01 g,
aspartame – 0.01 g,
colloidal silicon dioxide – 0.006 g,
hypromellose – 0.018 g,
titanium dioxide – 0.012 g,
milk flavoring – 0.1 g,
caramel flavoring – 0.05 g,
cream flavoring – 0.05 g.
Pregnancy
Pregnancy
Pregnancy:
Airtal® is contraindicated during pregnancy. There is no information on the use of aceclofenac during pregnancy.
Inhibition of prostaglandin synthesis may adversely affect the course of pregnancy and/or the development of the embryo/fetus.
During the third trimester of pregnancy, all prostaglandin synthesis inhibitors:
– having cardiopulmonary toxicity, they can cause premature closure of the Botallo duct with the development of pulmonary hypertension;
– may cause impaired fetal renal function, which can progress to renal failure in combination with oligohydramnios.
Late pregnant mothers and newborns:
– the drug may affect the duration of bleeding due to the antiplatelet effect, which can develop even after using very low doses;
– the drug may suppress uterine contractions, leading to delayed labor or prolonged labor.
Lactation:
Airtal® should not be taken during breastfeeding. There is no data on the excretion of aceclofenac in human milk; When radioactive 14C-aceclofenac was administered to lactating rats, no noticeable transfer of radioactivity into milk was observed.
Fertility:
NSAIDs may affect fertility and are not recommended for use by women planning pregnancy.
Contraindications
Contraindications
– erosive and ulcerative lesions of the gastrointestinal tract in the acute phase (including ulcerative colitis, Crohn’s disease);
– gastrointestinal bleeding or suspicion of it;
– complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid or other NSAIDs (including a history);
– hypersensitivity to aceclofenac or components of the drug Airtal;
– severe liver failure or active liver disease;
– disorders of hematopoiesis and coagulation;
– severe renal failure (creatinine clearance <30 ml/min), progressive kidney disease, confirmed hyperkalemia;
– severe heart failure;
– period after coronary artery bypass grafting;
– pregnancy and lactation;
– children’s age up to 18 years:
– fructose intolerance;
– feinylketonuria.
With caution:
Chronic heart failure, coronary heart disease, arterial hypertension, decreased circulating blood volume (including conditions after major surgical interventions), cerebrovascular diseases, peripheral arterial diseases, chronic renal failure (creatinine clearance less than 60 ml/min), liver failure, history of liver, kidney and gastrointestinal diseases, history of ulcerative colitis, Crohn’s disease history, bronchial asthma, dyspeptic symptoms at the time of drug prescription, anamnestic data on the development of ulcerative lesions of the gastrointestinal tract, the presence of Helicobacter pylori infection, diabetes mellitus, dyslipidemia/hyperlipidemia, old age, smoking, long-term use of NSAIDs, use of systemic glucocorticosteroids, anticoagulants, antiplatelet agents, serotonin reuptake inhibitors, diuretics, alcoholism, severe somatic diseases, hematological diseases, hematopoietic disorders, systemic lupus erythematosus (SLE), porphyria, chickenpox.
Side Effects
Side Effects
The following are adverse events reported in clinical studies and post-marketing surveillance; Adverse events are grouped according to Medical Dictionary for Regulatory Activities (MedDRA) organ system classes and frequency of occurrence. Very common (≥1/10); often (from ≥1/100 to
– Blood and lymphatic system disorders Rare: anemia.
Very rare: bone marrow suppression, granulocytopenia, thrombocytopenia, neutropenia, hemolytic anemia.
– Immune system disorders
Rare: anaphylactic reactions (including shock), hypersensitivity.
– Metabolic and nutritional disorders
Very rare: hyperkalemia.
– Mental disorders
Very rare: depression, unusual dreams, insomnia.
– Nervous system disorders
Common: dizziness.
Very rare: paresthesia, tremor, drowsiness, headache, dysgeusia (taste perversion).
– Visual disorders
Rarely: visual disturbance.
– Hearing and labyrinth disorders
Very rare: dizziness, ringing in the ears.
– Cardiac disorders
Rare: heart failure.
Very rare: palpitations.
– Vascular disorders
Rarely: increased blood pressure, worsening arterial hypertension.
Very rare: hyperemia, hot flashes, vasculitis.
– Disorders of the respiratory system, thoracic and mediastinal organs
Rarely: shortness of breath.
Very rare: bronchospasm.
– Gastrointestinal disorders
Common: dyspepsia, abdominal pain, nausea, diarrhea.
Uncommon: flatulence, gastritis, constipation, vomiting, ulcerative stomatitis.
Rarely: melena, formation of stomach and intestinal ulcers, hemorrhagic diarrhea, gastrointestinal bleeding.
Very rare: stomatitis, vomiting blood, intestinal perforation, exacerbation of Crohn’s disease and ulcerative colitis, pancreatitis.
– Disorders of the liver and biliary tract
Common: increased activity of liver enzymes.
Very rare: liver disease (including hepatitis), increased alkaline phosphatase activity.
– Disorders of the skin and subcutaneous tissues
Uncommon: itching, rash, dermatitis, urticaria.
Rare: Quincke’s edema.
Very rare: purpura, eczema, severe mucocutaneous reactions (including Stevens-Johnson syndrome and toxic epidermal necrolysis).
– Renal and urinary tract disorders
Uncommon: increased serum urea concentration, increased serum creatinine concentration.
Very rare: nephrotic syndrome, renal failure.
– General disorders and disorders at the injection site
Very rare: swelling, weakness, muscle cramps.
– Changes in laboratory and instrumental studies
Very rare: weight gain.
Interaction
Interaction
No drug interaction studies have been conducted, with the exception of interaction studies with warfarin.
Aceclofenac is metabolized in the cytochrome P450 2C9 system and, according to in vitro studies, can inhibit this isoenzyme. Therefore, there is a possible risk of pharmacokinetic interactions with phenytoin, cimetidine, tolbutamide, phenylbutazone, amiodarone, miconazole and sulfaphenazole. As with other NSAIDs, there is also a risk of pharmacokinetic interactions with other renally excreted drugs such as methotrexate and lithium. Aceclofenac is almost completely bound to plasma proteins; therefore, there is a possibility of interaction with other drugs that have a high affinity for plasma proteins, by type of substitution, which should be taken into account.
Since pharmacokinetic interaction studies are insufficient, the information below is based on data obtained for other NSAIDs:
The following combinations of drugs should be avoided:
Lithium and digoxin: Some NSAIDs inhibit the renal clearance of lithium and digoxin, resulting in increased serum concentrations of these drugs. This combination of drugs should be avoided unless frequent monitoring of lithium and digoxin levels is possible.
Anticoagulants: NSAIDs inhibit platelet aggregation and damage the gastrointestinal mucosa, which may lead to increased anticoagulant activity and increase the risk of gastrointestinal bleeding in patients taking anticoagulants. The combination of aceclofenac and oral coumarin anticoagulants, ticlopidine, thrombolytic drugs and heparin should be avoided unless closely monitored.
Antiplatelet drugs and selective serotonin reuptake inhibitors in combination with NSAIDs may increase the risk of gastrointestinal bleeding. The following combinations of drugs may require dose adjustment and caution:
Methotrexate: NSAIDs inhibit the tubular secretion of methotrexate, so the possible interactions between NSAIDs and methotrexate should also be considered when treating with low doses of methotrexate, especially in patients with renal impairment. In cases where combination treatment is necessary, renal function should be monitored. Caution should be exercised when both NSAIDs and methotrexate are administered together within 24 hours, as methotrexate concentrations may increase, resulting in increased toxicity.
Cyclosporine, tacrolimus: Concomitant use of NSAIDs and cyclosporine or tacrolimus is considered to increase the risk of renal toxicity due to decreased renal prostacyclin synthesis. Therefore, it is very important to carefully monitor renal function during combination treatment.
Other NSAIDs: Concomitant use of acetylsalicylic acid and other NSAIDs may increase the incidence of adverse events, so caution should be exercised.
Glucocorticosteroids: The risk of developing gastrointestinal ulcers or gastrointestinal bleeding may increase.
Diuretics: aceclofenac, like other NSAIDs, can inhibit the activity of diuretics, reduce the diuretic effect of furosemide, bumetanide and the antihypertensive effect of thiazides. Concomitant treatment with potassium-sparing diuretics may be associated with an increase in potassium levels; therefore, it is necessary to monitor serum potassium levels.
Aceclofenac has been shown to have no effect on blood pressure control when used concomitantly with bendrofluazide, although drug interactions with other diuretics cannot be excluded.
Antihypertensive drugs: NSAIDs may also reduce the effectiveness of certain antihypertensive drugs. ACE inhibitors or angiotensin II receptor antagonists in combination with NSAIDs can lead to impaired renal function. Some patients with reduced kidney function, such as elderly patients or patients with dehydration, may be at risk of developing acute renal failure, which is usually reversible. Therefore, caution should be exercised when combining these drugs with NSAIDs, especially when treating elderly or dehydrated patients. Patients should be adequately hydrated and it is recommended that renal function be monitored after initiation of combination treatment and periodically during treatment.
Aceclofenac has been shown to have no effect on blood pressure control when administered concomitantly with bendrofluazide, although interactions with other diuretics cannot be excluded.
Hypoglycemic drugs: Clinical studies have shown that diclofenac can be used concomitantly with oral hypoglycemic drugs without affecting their clinical effectiveness. However, there are isolated reports of hypoglycemic and hyperglycemic effects of this drug. Therefore, with regard to aceclofenac, the possibility of dose adjustment of drugs that can cause hypoglycemia should be considered.
Zidovudine: Concomitant use of NSAIDs and zidovudine increases the risk of hematological toxicity. There is evidence of an increased risk of hemarthrosis and hematoma formation in HIV-positive patients with hemophilia receiving concomitant treatment with zidovudine and ibuprofen.
Overdose
Overdose
There is no data on an overdose of aceclofenac in humans.
Possible symptoms: nausea, vomiting, stomach pain, dizziness, headache, hyperventilation with increased convulsive readiness.
Treatment: gastric lavage, administration of activated carbon, symptomatic therapy. Forced diuresis and hemodialysis are not effective enough.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C
Shelf life
Shelf life
4 years
Manufacturer
Manufacturer
Industrias Pharmaceuticas Almiralle S.A., Spain
Additional information
| Shelf life | 4 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | Industrias Pharmaseuticas Almirall S.A., Spain |
| Medication form | Powder for oral suspension |
| Brand | Industrias Pharmaseuticas Almirall S.A. |
Other forms…
Related products
Buy Aertal, 3 g 20 pcs. with delivery to USA, UK, Europe and over 120 other countries.