No products in the cart.
Actrapid NM Penfill, 100 me/ml 3 ml 5 pcs
€25.67 €21.39
Description
Actrapid® NM is a short-acting insulin preparation produced by recombinant DNA biotechnology using Saccharomyces cerevisiae strain.
Low blood glucose levels are reduced by increasing its intracellular transport after insulin binds to insulin receptors of muscle and adipose tissue and simultaneously reducing the rate of glucose production by the liver.
The normalization of plasma glucose concentration (up to 4.4-6.1 mmol/l) during intravenous administration of Actrapid® NM in intensive care unit patients who underwent serious surgical interventions (204 patients with diabetes and 1344 patients without diabetes) who had hyperglycemia (plasma glucose concentration > 10 mmol/L), reduced mortality by 42% (4.6% instead of 8%).
The action of Actrapid® NM begins within half an hour after administration and the maximum effect is seen within 1.5-3.5 hours, with a total duration of action of about 7-8 hours.
Indications
Indications
Diabetes mellitus.
Emergency conditions in patients with diabetes mellitus accompanied by impaired glycemic control.
Pharmacological effect
Pharmacological effect
Actrapid® NM is a short-acting insulin preparation produced by recombinant DNA biotechnology using the Saccharomyces cerevisiae strain.
A decrease in blood glucose levels occurs due to an increase in its intracellular transport after the binding of insulin to insulin receptors in muscle and adipose tissue and a simultaneous decrease in the rate of glucose production by the liver.
Normalization of plasma glucose concentration (to 4.4-6.1 mmol/l) with intravenous administration of the drug Actrapid® NM in intensive care unit patients undergoing major surgical interventions (204 patients with diabetes mellitus and 1344 patients without diabetes mellitus) who had hyperglycemia (plasma glucose concentration > 10 mmol/l) reduced mortality by 42% (4.6% instead of 8%).
The effect of the drug Actrapid® NM begins within half an hour after administration, and the maximum effect appears within 1.5-3.5 hours, while the total duration of action is about 7-8 hours.
Special instructions
Special instructions
An insufficient dose of the drug or cessation of treatment, especially in type 1 diabetes, can lead to the development of hyperglycemia. As a rule, the first symptoms of hyperglycemia appear gradually, over several hours or days. Symptoms of hyperglycemia are a feeling of thirst, increased urination, nausea, vomiting, drowsiness, redness and dryness of the skin, dry mouth, loss of appetite, and the appearance of the smell of acetone in the exhaled air. Without appropriate treatment, hyperglycemia in patients with type 1 diabetes can lead to diabetic ketoacidosis, a condition that is potentially fatal.
Hypoglycemia
Hypoglycemia can develop if a dose of insulin is administered that is too high in relation to the patient’s needs.
Skipping meals or unplanned intense exercise can lead to hypoglycemia.
After compensation of carbohydrate metabolism, for example, with intensified insulin therapy, patients may experience changes in their typical symptoms that are precursors of hypoglycemia, of which patients should be informed. The usual warning symptoms may disappear with prolonged diabetes mellitus.
Transferring patients to another type of insulin or to insulin from another manufacturer should only be done under medical supervision. If the concentration, manufacturer, type, type (human insulin, human insulin analogue) and/or method of manufacture changes, the dose of insulin may need to be changed. Patients switching to treatment with Actrapid NM may require a dose change or an increase in the frequency of injections compared to previously used insulin preparations. If a dose adjustment is necessary when transferring patients to treatment with Actrapid NM, this can be done already with the first dose or in the first weeks or months of therapy.
As with treatment with other insulin drugs, reactions may develop at the injection site, which is manifested by pain, redness, urticaria, inflammation, hematoma, swelling and itching. Regularly changing the injection site in the same anatomical area will help reduce symptoms or prevent these reactions from developing. The reactions usually disappear within a few days to a few weeks. In rare cases, it may be necessary to discontinue Actrapid NM due to reactions at the injection sites. Before traveling due to jet lag, the patient should consult with his/her physician, as jet lag means that the patient must eat and take insulin at different times.
When adding Actrapid NM to solutions for infusion, the amount of insulin absorbed by the infusion system is unpredictable, therefore the use of Actrapid NM in CSII is not permitted.
Simultaneous use of drugs of the thiazolidinedione group and insulin drugs
Cases of the development of chronic heart failure have been reported when patients were treated with thiazolidinediones in combination with insulin drugs, especially if such patients have risk factors for the development of chronic heart failure. This fact should be taken into account when prescribing combination therapy with thiazolidinediones and insulin drugs to patients. When prescribing such combination therapy, it is necessary to conduct medical examinations of patients to identify signs and symptoms of chronic heart failure, weight gain and the presence of edema. If heart failure symptoms worsen in patients, treatment with thiazolidinediones should be discontinued.
Impact on the ability to drive vehicles and operate machinery
Patients’ ability to concentrate and react quickly may be impaired during hypoglycemia, which can be dangerous in situations where these abilities are especially needed (for example, when driving or operating machinery). Patients should be advised to take measures to prevent the development of hypoglycemia when driving vehicles. This is especially important for patients with no or decreased severity of symptoms that are warning signs of developing hypoglycemia or who suffer from frequent episodes of hypoglycemia. In these cases, the advisability of driving vehicles and performing similar work should be considered.
Active ingredient
Active ingredient
Insulin soluble human genetically engineered
Composition
Composition
1 ml of the drug contains:
Active substance:
soluble insulin (human genetically engineered) 100 IU (3.5 mg);
1 IU corresponds to 0.035 mg of anhydrous human insulin;
Excipients:
zinc 7 mcg (as zinc chloride),
glycerin (glycerol) 16 mg,
metacresol 3.0 mg,
sodium hydroxide about 2.6 mg and/or hydrochloric acid about 1.7 mg (to adjust pH),
water for injections up to 1.0 ml.
Contraindications
Contraindications
Hypersensitivity to human insulin or to any component of this drug.
Hypoglycemia.
Side Effects
Side Effects
The most common adverse event with insulin use is hypoglycemia. During clinical studies, as well as during the use of the drug after its release to the consumer market, it was found that the incidence of hypoglycemia varies depending on the patient population, drug dosage regimen and glycemic control. At the initial stage of insulin therapy, refractive errors, swelling and reactions at the injection site may occur (including pain, redness, urticaria, inflammation, hematoma, swelling and itching at the injection site). These symptoms are usually temporary. Rapid improvement in glycemic control can lead to a condition of “acute painful neuropathy”, which is usually reversible.
Intensification of insulin therapy with a sharp improvement in the control of carbohydrate metabolism can lead to a temporary worsening of diabetic retinopathy, while at the same time, long-term improvement in glycemic control reduces the risk of progression of diabetic retinopathy. The list of side effects is presented below.
All side effects presented below, based on data obtained during clinical trials, are divided into groups according to the frequency of occurrence in accordance with MedDRA and organ systems. The incidence of side effects is defined as: very often (≥1/10); often (≥1/100 to <1/10); uncommon (≥1/1000 to <1/100); rare (≥1/10,000 to <1/1000), very rare (<1/10,000) and unknown (cannot be estimated from available data).
Immune system disorders: uncommon – urticaria, skin rash; very rarely – anaphylactic reactions.
Metabolic and nutritional disorders: very often – hypoglycemia.
Nervous system disorders: uncommon – peripheral neuropathy (“acute painful neuropathy”).
Violations of the organ of vision: infrequently – refractive errors; very rarely – diabetic retinopathy.
Disorders of the skin and subcutaneous tissues: infrequently – lipodystrophy.
General disorders and disorders at the injection site: uncommon – reactions at the injection site; infrequently – edema.
Description of individual adverse reactions:
Anaphylactic reactions
Very rare reactions of generalized hypersensitivity have been observed (including generalized skin rash, itching, increased sweating, gastrointestinal disorders, angioedema, difficulty breathing, rapid heartbeat, decreased blood pressure, and fainting/loss of consciousness, which are potentially life-threatening.
Hypoglycemia
Hypoglycemia is the most common side effect. It can develop if the insulin dose is too high in relation to the insulin requirement. Severe hypoglycemia can lead to loss of consciousness and/or seizures, temporary or permanent damage to brain function, or even death. Symptoms of hypoglycemia usually develop suddenly. These may include cold sweats, pale skin, fatigue, nervousness or tremors, anxiety, unusual tiredness or weakness, disorientation, decreased concentration, drowsiness, increased hunger, blurred vision, headache, nausea, and rapid heartbeat.
Lipodystrophy
Rare cases of lipodystrophy have been reported. Lipodystrophy may develop at the injection site.
Interaction
Interaction
There are a number of medications that affect the need for insulin. The hypoglycemic effect of insulin is enhanced by oral hypoglycemic drugs, monoamine oxidase inhibitors, angiotensin-converting enzyme inhibitors, carbonic anhydrase inhibitors, non-selective beta-blockers, bromocriptine, sulfonamides, anabolic steroids, tetracyclines, clofibrate, ketoconazole, mebendazole, pyridoxine, theophylline, cyclophosphamide, fenfluramine, lithium preparations, salicylates.
The hypoglycemic effect of insulin is weakened by oral contraceptives, glucocorticosteroids, thyroid hormones, thiazide diuretics, heparin, tricyclic antidepressants, sympathomimetics, growth hormone (somatropin), danazol, clonidine, slow calcium channel blockers, diazoxide, morphine, phenytoin, nicotine.
Beta blockers may mask the symptoms of hypoglycemia and impair recovery from hypoglycemia. Octreotide/lanreotide can either increase or decrease the body’s need for insulin.
Alcohol can increase or decrease the hypoglycemic effect of insulin.
Incompatibility
Actrapid NM can only be added to compounds with which it is known to be compatible. Some drugs (for example, drugs containing thiols or sulfites) when added to an insulin solution can cause its degradation.
Overdose
Overdose
There is no specific dose required for insulin overdose, but hypoglycemia can develop gradually if doses of insulin are administered that are too high in relation to the patient’s needs.
The patient can eliminate mild hypoglycemia himself by ingesting glucose or sugar-containing foods. Therefore, patients with diabetes are advised to carry sugar-containing products with them at all times.
In cases of severe hypoglycemia when the patient is unconscious, 0.5 mg to 1 mg of glucagon should be administered intramuscularly or subcutaneously (can be administered by a trained person), or a dextrose (glucose) solution should be administered intravenously (can only be administered by a healthcare professional). It is also necessary to administer dextrose intravenously if the patient does not regain consciousness 10-15 minutes after the administration of glucagon. After regaining consciousness, the patient is advised to take a carbohydrate-rich meal to prevent relapse of hypoglycemia.
Storage conditions
Storage conditions
In a place protected from light, at a temperature of 2–8 °C (do not freeze)
Shelf life
Shelf life
2.5 years
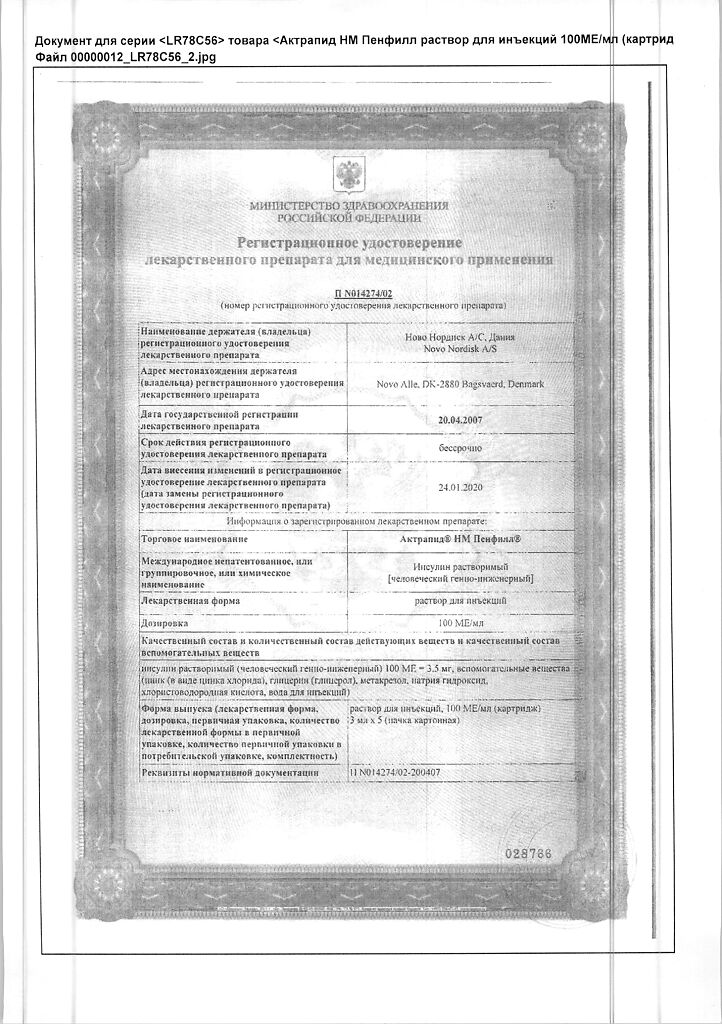
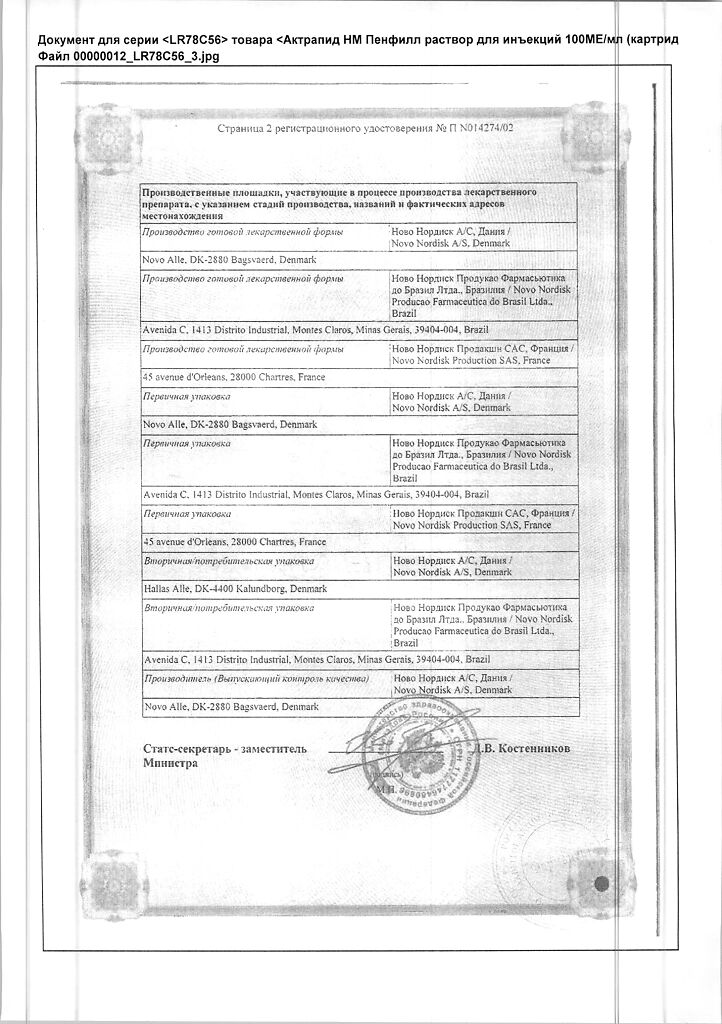
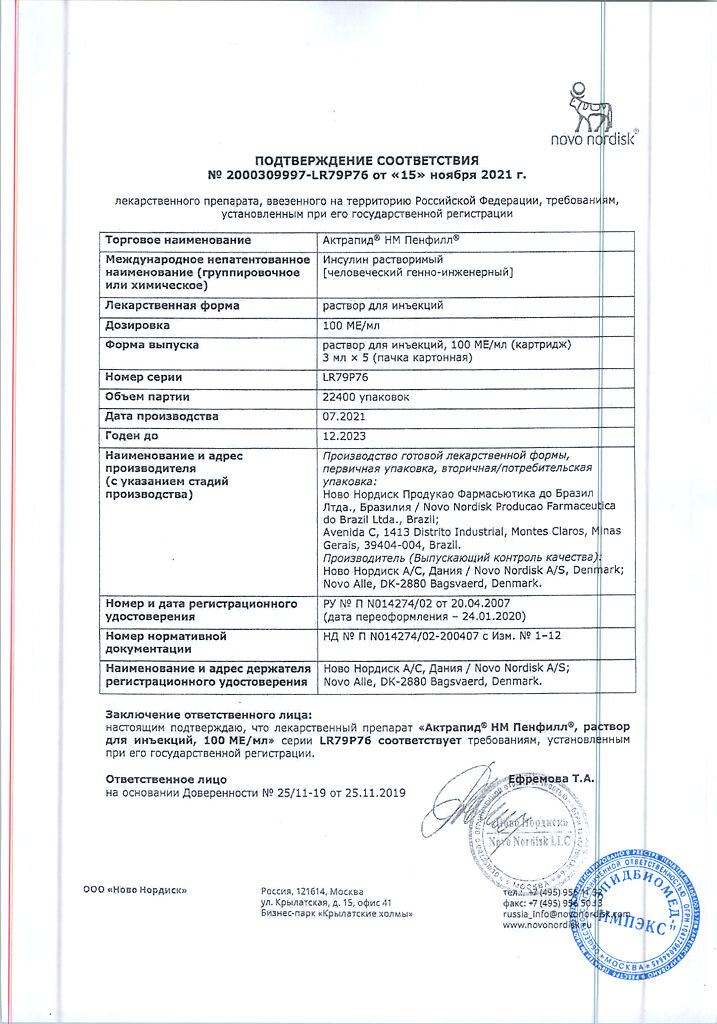
Manufacturer
Manufacturer
Novo Nordisk A/S, Denmark
Additional information
| Shelf life | 2.5 years |
|---|---|
| Conditions of storage | In the dark place at 2-8 °C (do not freeze) |
| Manufacturer | Novo Nordisk A/S, Denmark |
| Medication form | solution for injection |
| Brand | Novo Nordisk A/S |
Related products
Buy Actrapid NM Penfill, 100 me/ml 3 ml 5 pcs with delivery to USA, UK, Europe and over 120 other countries.