No products in the cart.
Zoloft, 50 mg 14 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Zoloft is an antidepressant.
Pharmacodynamics
Sertraline is an antidepressant, a potent specific inhibitor of serotonin reuptake (5-NT) in neurons. It has a very weak effect on norepinephrine and dopamine reuptake. At therapeutic doses, sertraline blocks serotonin uptake in human platelets. It has no stimulant, sedative or anticholinergic effects. Due to its selective inhibition of 5-NT uptake, sertraline does not increase adrenergic activity. Sertraline has no affinity for muscarinic (cholinergic), serotoninergic, dopaminergic, adrenergic, histaminergic, GABA or benzodiazepine receptors.
Sertraline does not cause drug dependence and weight gain with prolonged use.
Pharmacokinetics
Absorption is high (but at a slow rate). Bioavailability is increased with food by 25%. Food increases Cmax by 25% and shortens Tmax. In humans, when treated with sertraline at a dose of 50 to 200 mg once daily for 14 days, the Tmax in plasma is 4.5-8.4 h after ingestion. Cmax and AUC are proportional over a dose range of 50-200 mg of sertraline once daily for 14 days, with a linear pharmacokinetic relationship. The pharmacokinetic profile in adolescents and the elderly does not differ from that in patients aged 18 to 65 years. The mean T1/2 of sertraline in young and elderly men and women is 22-36 h. Corresponding to the final T1/2 there is approximately double cumulation of the drug before the onset of CSS after 1 week of treatment (once-daily dose). Binding to plasma proteins is approximately 98%. It has been shown that the pharmacokinetics of sertraline in children with obsessive-compulsive disorder (OCD, see below) are similar to those in adults (although the metabolism of sertraline is somewhat more active in children). However, given the lower body weight in children (especially those aged 6-12 years), a lower dose of the drug is recommended to avoid excessive plasma levels.
Sertraline undergoes active biotransformation on first passage through the liver. The major metabolite found in plasma, N-desmethylsertraline, is significantly inferior (approximately 20-fold) to sertraline in in vitro activity and is virtually inactive in in vivo models of depression. The T1/2 of N-desmethylsertraline varies from 62-104 h. Sertraline and N-desmethylsertraline are actively biotransformed; the resulting metabolites are excreted in equal amounts in the feces and urine. Unchanged sertraline is excreted in insignificant amounts in the urine (1/2 of the drug and AUC compared to those of healthy subjects.
Indications
Indications
Zoloft is indicated for the treatment of:
– episodes of major depressive disorder and prevention of relapse of episodes of major depressive disorder in adults over 18 years of age;
– panic disorder with or without agoraphobia in adults over 18 years of age;
– obsessive-compulsive disorder (OCD) in adults and children aged 6 years and older;
– social anxiety disorder in adults over 18 years of age;
– post-traumatic stress disorder (PTSD) in adults over 18 years of age.
Pharmacological effect
Pharmacological effect
Mechanism of action
Sertraline is a potent selective inhibitor of serotonin (5-HT) reuptake in neurons in vitro, resulting in enhanced psychological effects of 5-HT in animals. It has only a very weak effect on the reuptake of norepinephrine and dopamine by neurons. At clinical doses, sertraline blocks the uptake of serotonin by human platelets. The drug does not have stimulant, sedative or anticholinergic effects, and also does not exhibit cardiotoxic effects in animal studies. In controlled studies in healthy volunteers, sertraline did not have a sedative effect and did not affect psychomotor activity. Consistent with selective 5-HT reuptake inhibition, sertraline does not affect catecholaminergic activity. Sertraline has no affinity for muscarinic (cholinergic), serotonergic, dopaminergic, adrenergic, histaminergic, GABAergic and benzodiazepine receptors. Long-term use of sertraline in animals was accompanied by a decrease in the activity of norepinephrine receptors in the brain, which is also observed when using other clinically effective antidepressant and anti-obsessive drugs.
Sertraline does not cause drug dependence. In a placebo-controlled, double-blind, randomized study of the comparative addictogenic potential of sertraline, alprazolam, and d-amphetamine in humans, sertraline did not have positive subjective effects indicative of addictive potential. In contrast, patients rated both alprazolam and d-amphetamine significantly higher than placebo on measures of favorable attitude toward the drug, euphoria, and addictive potential. Sertraline did not produce the stimulant or anxiety effects associated with d-amphetamine, or the sedative effects and psychomotor impairment associated with alprazolam. Sertraline does not act as a positive reinforcer in rhesus monkeys trained to self-administer cocaine, nor does it replace either d-amphetamine or pentobarbital as a differential reinforcer in rhesus monkeys.
Clinical efficacy and safety
Major depressive disorder
A study was conducted in depressed outpatients who responded to sertraline 50–200 mg/day at the end of an initial 8-week open-label treatment phase. These patients (N = 295) were randomized to continue treatment with sertraline 50–200 mg/day or placebo for 44 weeks in a double-blind manner. Patients taking sertraline had a statistically significant lower relapse rate than patients taking placebo. The average dose of the drug in patients who completed the course of treatment was 70 mg/day. The proportion of patients who responded to treatment (response to treatment was defined as absence of relapse) was 83.4% in the sertraline group and 60.8% in the placebo group.
Post-traumatic stress disorder (PTSD)
Pooled data from 3 studies examining PTSD in the general population showed that treatment response rates were lower in men than in women. In the two studies in the general population that reported positive results, treatment response rates were comparable between men and women in the sertraline and placebo groups (women: 57.2% versus 34.5%; men: 53.9% versus 38.2%). The pooled total study population included 184 men and 430 women. Therefore, treatment results in women are more reliable, and in men there was a relationship between treatment results and characteristics at baseline (higher incidence of drug abuse, longer duration of illness, cause of injury, etc.), which correlated with a decrease in the effectiveness of therapy.
Electrophysiology of the heart
In a dedicated, well-designed QTc interval study performed using supratherapeutic doses at steady state in healthy volunteers (receiving 400 mg/day, twice the recommended daily dose), the upper limit of the 2-sided 90% CI for the time-matched least squares mean difference in QTcF between sertraline and placebo (11.666) ms) was greater than the preset threshold of 10 s at the 4-hour post-dose time point. Exposure-response analysis indicated a non-significant positive relationship between QTcF duration and sertraline plasma concentration (0.036 ms/(ng/mL); p < 0.0001). Based on the exposure model, the threshold for clinically significant QTcF prolongation (i.e., predicted 90% CI greater than 10 ms) is at least 2.6 times the mean Cmax (86 ng/mL) following the highest recommended dose of sertraline (200 mg/day) (see sections 4.4, 4.5, 4.8 and 4.9).Pediatric patients with OCD
The safety and effectiveness of sertraline (at a dose of 50–200 mg/day) was studied in the treatment of outpatient children (6 to 12 years) and adolescents (13 to 17 years) with obsessive-compulsive disorder (OCD) without symptoms of depression. After completing a one-week single-blind placebo run-in period, patients were randomized to receive sertraline or placebo at a variable dose for 12 weeks. For children aged 6 to 12 years, the initial dose of the drug was 25 mg. Patients randomized to the sertraline group showed significantly greater improvement compared with patients receiving placebo, as measured by scores on the Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS) (p = 0.005), National Institute of Mental Health General Obsessive-Compulsive Scale (P=0.005). – NIMH) (p = 0.019) and the subscale for assessing improvement of the Clinical Global Impression (CGI) scale (p = 0.002). In addition, the sertraline group tended to show greater improvement than the placebo group on the CGI severity subscale (p = 0.089). In the placebo group, the mean CY-BOCS score at baseline was 22.25 ± 6.15, and the change in this indicator from baseline was –3.4 ± 0.82, and in the sertraline group, the values of these indicators were 23.36 ± 4.56 and –6.8 ± 0.87, respectively. In a retrospective analysis, the proportion of patients who responded to treatment was 53% in the sertraline group compared with 37% in the placebo group (p = 0.03). Treatment response was defined as a reduction in CY-BOCS score, the primary outcome measure, of at least 25% at endpoint compared with baseline.
Long-term clinical studies assessing effectiveness in pediatric patients have not been conducted.
Children
There are no data on the use of the drug in children under 6 years of age.
Post-marketing safety study of SPRITES
An observational post-marketing safety study was conducted in 941 patients aged 6 to 16 years to evaluate the long-term safety of sertraline treatment (with or without psychotherapy) compared with psychotherapy on cognitive, emotional, physical and pubertal maturation lasting up to 3 years. This study was also conducted in a clinical setting in children and adolescents with a primary diagnosis of OCD, depression, or other anxiety disorders, and assessed cognitive function (as assessed by the Number-Letter Connection Test (Part B) and the metacognitive index from the Behavior Rating Inventory of Executive Function (BRIEF), behavioral/emotional control (as assessed by the Behavioral Control Index from the BRIEF), and physical/pubertal maturation (assessed by standardized height/weight index/body mass index (BMI) and Tanner scale)]. Sertraline is approved for use in pediatric patients only for children aged 6 years and older with OCD (see section 4.1).
Standardization for each primary outcome measure based on age- and sex-specific norms indicated that overall results were consistent with normal development. There were no statistically significant differences in the main efficacy criteria, with the exception of body weight. A statistically significant change for standardized body weight was observed in the comparative analyses, but the magnitude of the change in body weight was small [mean (SD) change in standardized z-scores < 0.5 SD]. Body weight increased depending on the dose of the drug.Absorption
When administered orally daily at a dose of 50 to 200 mg once daily for 14 days, peak concentrations of sertraline in human plasma were achieved approximately 4.5 to 8.4 hours after dosing.
Food intake does not significantly affect the bioavailability of sertraline tablets.
Distribution
Approximately 98% of the drug binds to blood plasma proteins.
Biotransformation
Sertraline undergoes active first-pass metabolism in the liver.
Clinical and in vitro data indicate that sertraline is metabolized via multiple pathways, including CYP3A4, CYP2C19 (see section 4.5) and CYP2B6. Under in vitro conditions, sertraline and its main metabolite, desmethyl sertraline, are also p-glycoprotein substrates.
Elimination
The mean elimination half-life of sertraline is approximately 26 hours (range, 22 to 36 hours). Based on the terminal half-life, drug accumulation approximately doubles until steady state concentration is achieved, which is achieved after one week of once-daily dosing. The half-life of N-desmethylsertraline ranges from 62 to 104 hours. Sertraline and N-desmethylsertraline are actively metabolized in the human body, and the final metabolites are excreted in feces and urine in equal amounts. Only a small portion of sertraline (<0.2%) is excreted unchanged in the urine.
Linearity/nonlinearity
In the dose range from 50 to 200 mg, the pharmacokinetics of sertraline are proportional to the dose taken.
Special patient groups
Children
Pediatric patients with obsessive-compulsive disorder
The pharmacokinetics of sertraline were studied in a group of 29 patients aged 6 to 12 years and 32 adolescents aged 13 to 17 years. The initial dose of the drug, which was 25 or 50 mg per day, was gradually increased over 32 days (in increments of 25 or 50 mg, respectively) to 200 mg/day. These dosing regimens (25 mg and 50 mg increments) were equally well tolerated. When taking the drug at a dose of 200 mg, the concentration of sertraline in the blood plasma at steady state in the group of patients 6–12 years old was approximately 35% higher than in the group of patients 13–17 years old, and 21% higher than in adults in the comparison group. There were no statistically significant differences between boys and girls in terms of drug clearance. Thus, when using the drug in children, it is recommended to start treatment with a low dose and increase it in increments of 25 mg, especially in children with low body weight. In adolescents, the same doses can be used as in adults.
Teenagers and older people
The pharmacokinetic profile in both adolescents and elderly patients does not differ significantly from that in adult patients aged 18 to 65 years.
Liver failure
In patients with liver damage, the half-life of sertraline is increased and the AUC value is increased by 3 times (see sections 4.2 and 4.4).
Kidney failure
In patients with moderate to severe renal impairment, no significant accumulation of sertraline was observed.
Pharmacogenomics
In patients with low metabolizing activity of CYP2C19 enzymes, sertraline plasma concentrations were approximately 50% higher than in patients with high metabolizing activity. The clinical significance of these data is uncertain. The dose of the drug must be selected taking into account the clinical response to treatment.
Special instructions
Special instructions
Serotonin syndrome (SS) and neuroleptic malignant syndrome (NMS)
Potentially life-threatening syndromes such as serotonin syndrome (SS) and neuroleptic malignant syndrome (NMS) have been reported with the use of selective serotonin reuptake inhibitors (SSRIs), including sertraline. The risk of serotonin syndrome or NMS during treatment with SSRIs increases when sertraline is co-administered with other serotonergic drugs (including other serotonergic antidepressants, amphetamines and triptans), drugs that impair serotonin metabolism (including MAOIs, such as methylene blue), antipsychotic drugs and other dopamine antagonists, and opioids. Patients should be monitored for the development of signs and symptoms of serotonin syndrome or NMS.
Switching from selective serotonin reuptake inhibitors (SSRIs), antidepressants or anti-obsessive medications
There is only limited experience from controlled studies regarding the optimal timing of switching from SSRIs, antidepressants and anti-obsessive medications to sertraline. Therefore, caution and careful medical judgment should be used when changing medications, especially long-acting medications such as fluoxetine.
Other serotonergic drugs such as tryptophan, fenfluramine, and 5-HT receptor agonists
Co-administration of sertraline and other drugs that enhance the effects of serotonergic neurotransmission, such as amphetamines, tryptophan, fenfluramine, 5-HT receptor agonists or the herbal remedy St. John’s wort (Hypericum perforatum), should be used with caution and avoided if possible due to the potential risk of pharmacodynamic interactions.
Prolongation of the QTc interval/polymorphic ventricular tachycardia of the “pirouette” type (Torsade de pointes – TdP)
Cases of TdP and QTc prolongation have been reported during post-marketing use of sertraline. Most cases have been reported in patients at increased risk for QTc prolongation/TdP. The effect on QTc interval prolongation was confirmed in a comprehensive QTc interval study in healthy volunteers, showing a statistically significant positive exposure-response relationship. Therefore, in patients with additional risk factors for QTc prolongation, such as cardiovascular disease, hypokalemia or hypomagnesemia, a family history of QTc prolongation, bradycardia, and concomitant use of drugs that prolong the QTc interval, sertraline should be used with caution.
Activation of manic and hypomanic states
Symptoms of mania or hypomania have been reported in a small percentage of patients receiving commercially available antidepressants and anti-obsessive medications, including sertraline. In this regard, sertraline should be used with caution in patients with a history of manic/hypomanic states. During treatment, careful monitoring of the patient’s condition by a doctor is necessary. If the disease progresses to the manic phase, sertraline therapy should be discontinued.
Schizophrenia
Psychotic symptoms may increase in patients with schizophrenia.
Cramps
Convulsive seizures may occur during treatment with sertraline, so use of the drug should be avoided in patients with unstable epilepsy and the condition of patients with controlled epilepsy should be carefully monitored. If seizures develop, sertraline therapy should be discontinued.
Suicide/suicidal thoughts/suicide attempts or clinical exacerbation
Depression increases the likelihood of suicidal thoughts and increases the risk of self-harm and suicide (suicidal acts and manifestations). This risk continues until there is significant improvement in symptoms. Since improvement may not occur within the first few weeks of treatment, patients should be closely monitored until improvement occurs. Clinical experience to date shows that the initial stage of treatment may increase the risk of suicide.
Other mental disorders for which sertraline is intended to treat may also be associated with an increased risk of suicidal behavior and behavior. These disorders may also co-occur with depression (major depressive disorder). Therefore, the same precautions should be taken when treating patients with other mental illnesses as when treating patients with major depressive disorder.
If you have a history of suicidal actions and manifestations, as well as if there are significant manifestations of suicidal thinking before starting treatment, the likelihood of suicidal thoughts and suicide attempts during treatment increases. In such cases, it is necessary to especially carefully monitor the condition of patients during treatment. A meta-analysis of placebo-controlled clinical trials of antidepressants in adult patients under 25 years of age with mental disorders demonstrated an increased likelihood of suicidal behavior with antidepressants compared with placebo.
When conducting drug therapy, especially at the initial stage and after changing the dose of drugs, it is necessary to carefully monitor the condition of patients, especially patients at high risk of suicide. Patients (and their caregivers) should be warned to monitor for any signs of clinical exacerbation, suicidal behavior or ideation, or unusual changes in behavior. If these symptoms occur, you should seek immediate medical attention.
Sexual dysfunction
Selective serotonin reuptake inhibitors (SSRIs) may cause symptoms of sexual dysfunction. There have been reports of long-term sexual dysfunction, symptoms of which persisted despite discontinuation of SSRIs.
Children
Sertraline should not be used to treat children and adolescents under 18 years of age, except in patients with OCD aged 6 years or older. In clinical studies, suicidality (suicide attempts and suicidal ideation) and hostility (primarily aggression, oppositional behavior, and anger) were observed more frequently in children and adolescents receiving antidepressant therapy than in those receiving placebo. If a decision has been made to proceed with therapy based on the clinical assessment of the patient, the patient should be carefully monitored for symptoms of suicidal behavior, especially at the beginning of therapy. Long-term safety in relation to cognitive, emotional, physical and pubertal maturation in children and adolescents aged 6 to 16 years was assessed in a long-term observational study of up to 3 years. Several cases of growth retardation and delayed puberty have been reported during post-marketing experience. The clinical significance and causality still remain unclear. When treating pediatric patients long-term, clinicians should monitor for developmental abnormalities.
Pathological bleeding/hemorrhage
Cases of abnormal bleeding, including bleeding into the skin (subcutaneous hemorrhage and purpura) and other bleeding phenomena such as gastrointestinal bleeding and genital bleeding (in women), including fatal bleeding, have been reported with the use of SSRIs. Taking SSRI/SNRI medications may increase the risk of postpartum hemorrhage. Caution is advised when using SSRIs in patients, especially when used concomitantly with drugs known to affect platelet function (eg, anticoagulants, atypical antipsychotics and phenothiazines, most tricyclic antidepressants, acetylsalicylic acid and nonsteroidal anti-inflammatory drugs (NSAIDs)), as is the case in patients with a history of bleeding disorders.
Hyponatremia
Hyponatremia may occur as a result of treatment with SSRIs or SNRIs, including sertraline. In many cases, hyponatremia appears to be a consequence of syndrome of inappropriate antidiuretic hormone secretion (SIADH). Cases of serum sodium levels below 110 mmol/L have been reported.
In elderly patients, the risk of developing hyponatremia may be increased when taking SSRIs and SNRIs. Patients taking diuretics or who are otherwise dehydrated may also be at increased risk (see Use in Elderly Patients). In patients with symptomatic hyponatremia, discontinuation of sertraline therapy should be considered; they should be provided with appropriate medical care. Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory loss, confusion, weakness, and poor balance, which can lead to falls. Signs and symptoms associated with more severe and/or acute cases included hallucination, syncope, seizures, coma, respiratory arrest, and death.
Withdrawal symptoms when stopping sertraline therapy
After discontinuation of the drug, especially in case of abrupt cessation of use, withdrawal syndrome often develops. In clinical studies, the incidence of withdrawal symptoms was 23% in patients who stopped taking the drug, compared with 12% of patients who continued sertraline therapy.
The likelihood of developing withdrawal symptoms may depend on a number of factors, including the dose and duration of treatment, and the rate of dose reduction. The most common reactions include dizziness, sensory disturbances (including paresthesia), sleep disturbances (including insomnia and vivid dreams), agitation or anxiety, nausea and/or vomiting, tremor and headache. Typically these symptoms are mild to moderate, but in some cases they can be severe. Usually these symptoms develop in the first few days after stopping treatment, but very rare cases of these symptoms appearing when a dose of the drug is accidentally missed are reported. Withdrawal symptoms usually resolve without treatment within 2 weeks, but in some patients they may persist for longer (2–3 months or longer). Therefore, upon discontinuation of therapy, it is recommended to gradually reduce the dose of sertraline over several weeks or months depending on the patient’s condition.
Akathisia/psychomotor agitation
The use of sertraline in some cases was accompanied by the development of akathisia, a condition characterized by an unpleasant or painful feeling of restlessness and a desire to move, combined with the inability to sit or stand quietly. These changes are more likely to develop in the first few weeks of treatment. Increasing the dose of the drug in the presence of these symptoms may lead to a worsening of the patient’s condition.
Liver dysfunction
Sertraline undergoes extensive metabolic transformation in the liver. In a multiple-dose pharmacokinetic study, patients with compensated mild liver cirrhosis experienced an increase in drug half-life and an approximately three-fold increase in AUC and Cmax values compared to patients without liver dysfunction. There were no significant differences between these two groups in the degree of binding of the drug to plasma proteins. The use of sertraline in patients with liver disease should be approached with caution. In patients with liver failure, the dose of the drug should be reduced or the frequency of its administration should be reduced. Sertraline is not recommended for use in patients with severe liver dysfunction.
Renal dysfunction
Sertraline undergoes extensive metabolic transformation, and excretion of the drug in urine in unchanged form is an additional route of elimination. In studies involving patients with mild to moderate renal impairment (creatinine clearance 30–60 ml/min) or moderate to severe renal impairment (creatinine clearance 10–29 ml/min), the main pharmacokinetic parameters with repeated dosing (AUC0–24 and Cmax) were not significantly different from patients with normal renal function. No dose adjustment of sertraline is required based on the degree of renal impairment.
Use in elderly patients
More than 700 elderly patients (>65 years) took part in clinical studies. The nature and incidence of adverse reactions in elderly patients were similar to those in younger patients.
However, clinically significant decreases in blood sodium levels have been reported when SSRIs and SNRIs, including sertraline, are used in elderly patients who may be at risk for developing hyponatremia (see Hyponatremia).
Diabetes mellitus
In patients with diabetes mellitus, SSRIs may impair glycemic control. These patients may require dosage adjustments of insulin and/or oral hypoglycemic agents.
Electroconvulsive therapy (ECT)
No clinical studies have been conducted to evaluate the risks and possible benefits of the combined use of ECT and sertraline.
Grapefruit juice
Drinking grapefruit juice during treatment with sertraline is not recommended.
Impact on urine screening tests
False-positive results of benzodiazepine immunoassays have been reported in patients taking sertraline. This was due to the lack of specificity of enzyme-linked immunosorbent screening assays. False-positive test results can be expected for several days after stopping sertraline therapy. Confirmatory tests such as gas chromatography/mass spectrometry will help differentiate sertraline from benzodiazepines.
Angle-closure glaucoma
SSRIs, including sertraline, can affect pupil size, causing mydriasis. This mydriatic effect can cause a narrowing of the angle of the eye, causing increased intraocular pressure and angle-closure glaucoma, especially in patients with a corresponding predisposition. In this regard, sertraline should be used with caution in patients with closed-angle glaucoma or a history of glaucoma. Sertraline can cause a narrowing of the anterior chamber angle of the eye, which can lead to increased intraocular pressure and the development of angle-closure glaucoma.
Excipients
Zoloft tablets in dosages of 50 mg and 100 mg contain 18.75 mg and 37.5 mg of sodium compounds, respectively. Patients following a hyposodium diet may be advised that this drug contains virtually no sodium.
Active ingredient
Active ingredient
Sertraline
Composition
Composition
Each tablet contains 55.95 mg sertraline hydrochloride, equivalent to 50 mg sertraline.
Excipients, the presence of which must be taken into account in the composition of the medicinal product: sodium carboxymethyl starch
Excipients:
Calcium hydrogen phosphate dihydrate
Microcrystalline cellulose (PH102)
Hyprolose
Sodium carboxymethyl starch
Magnesium stearate
Film casing:
Opadry white (contains hypromellose, titanium dioxide, macrogol 400, polysorbate 80);
Opadry transparent (contains hypromellose, macrogol 400/8000).
Pregnancy
Pregnancy
Pregnancy
No controlled studies have been conducted in pregnant women. However, a large body of evidence suggests that taking sertraline does not cause birth defects. Animal studies have shown a possible effect of sertraline on reproductive function, which is likely due to maternal toxicity caused by the pharmacodynamic effects of the active substance and/or direct pharmacodynamic effects of the drug on the fetus.
Some infants whose mothers took sertraline during pregnancy experienced symptoms similar to withdrawal reactions. This phenomenon was also observed when taking other SSRI antidepressants. It is not recommended to use sertraline during pregnancy, unless the expected benefit of treatment to the mother outweighs the possible risk to the fetus.
Observational data indicate an increased (less than 2-fold) risk of postpartum hemorrhage after using SSRI/SNRI drugs within one month before delivery.
It is necessary to monitor the condition of newborns whose mothers continued to take sertraline in late pregnancy (especially in the third trimester). Newborns whose mothers took sertraline during late pregnancy may experience the following symptoms: respiratory distress, cyanosis, apnea, convulsions, instability of body temperature, feeding difficulties, vomiting, hypoglycemia, hypertonicity, hypotonicity, hyperreflexia, tremors, muscle twitching, increased excitability, lethargy, prolonged crying, drowsiness and difficulty falling asleep. These symptoms may be due to direct serotonergic effects or may be drug withdrawal symptoms. In most cases, these symptoms begin immediately or shortly (within 24 hours) after birth.
Epidemiological studies suggest that the use of SSRIs during pregnancy (especially in late pregnancy) may increase the risk of persistent pulmonary hypertension of the newborn (PPHN). Thus, the observed incidence of PPHN was approximately 5 cases per 1000 births. Moreover, in the general population, PPHN occurs with a frequency of 1–2 cases per 1000 pregnancies.
Lactation
According to published data, sertraline and its metabolite N-desmethylsertraline are excreted in breast milk in small quantities. At the same time, these substances were not detected in the child’s blood serum or their concentrations were negligible. In only one case, the concentration in the infant’s blood serum was about 50% of the mother’s serum concentration (no visible negative effect on the child’s health was observed). Currently, there is no evidence that breastfeeding while taking sertraline negatively affects the health of the child. However, the risk cannot be completely eliminated. In this regard, the use of the drug in nursing mothers is not recommended (except in cases where the benefit, in the opinion of the doctor, outweighs the risk).
Fertility
Data from animal studies indicate that sertraline does not affect fertility.
According to the described clinical cases, taking some SSRIs has an effect on sperm quality, but this effect is reversible. To date, no effect of sertraline on human fertility has been observed.
Contraindications
Contraindications
The use of Zoloft is contraindicated in:
– hypersensitivity to the active substance or to any of the excipients
– The use of sertraline in patients receiving irreversible monoamine oxidase inhibitors (MAOIs) is contraindicated due to the risk of developing serotonin syndrome with symptoms such as restlessness, tremor and hyperthermia. Sertraline should be prescribed no earlier than 14 days after discontinuation of therapy with irreversible MAOIs. Sertraline therapy must be discontinued no later than 7 days before starting treatment with irreversible MAOIs.
– simultaneous use with pimozide is contraindicated.
Side Effects
Side Effects
Security Profile Summary
The most common adverse reaction is nausea. In the treatment of social anxiety disorder, sexual dysfunction (lack of ejaculation) was observed in men in 14% of cases when using sertraline, compared to 0% when using placebo. These adverse reactions are dose dependent and usually resolve with continued therapy.
When using the drug, blood pressure may increase.
The adverse reaction profile most frequently observed in double-blind, placebo-controlled studies in patients with OCD, panic disorder, PTSD and social anxiety disorder was no different from that observed in clinical studies in patients with depression.
The following is information about adverse reactions observed with sertraline, based on data obtained during post-marketing (frequency unknown) and placebo-controlled clinical studies (studies were conducted with 2542 patients receiving sertraline and 2145 patients receiving placebo). These studies were conducted in patients with depression, OCD, panic disorder, PTSD and social anxiety disorder.
Some of the adverse reactions listed below may decrease in intensity and frequency with continued therapy and generally do not lead to discontinuation of therapy.
Within each frequency group, adverse reactions are arranged in descending order of severity. The incidence is defined as: very common (≥ 1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), very rare (< 1/10,000) and frequency unknown (based on available data impossible to estimate)
Incidence of adverse reactions in placebo-controlled clinical trials for depression, OCD, panic disorder, PTSD, and social anxiety disorder.
Summary analysis and experience of post-marketing use.
Infections and infestations
Common – Upper respiratory tract infections, pharyngitis, rhinitis
Uncommon – Gastroenteritis, otitis media
Rarely – Diverticulitis§
Benign, malignant and unspecified neoplasms (including cysts and polyps)
Uncommon – Neoplasms
Blood and lymphatic system disorders
Rarely – Lymphadenopathy, thrombocytopenia*§, leukopenia*§
Immune system disorders
Uncommon – Hypersensitivity*, seasonal allergies*
Rarely – Anaphylactoid reactions*
Endocrine disorders
Uncommon – Hypothyroidism*
Rarely – Hyperprolactinemia*§, inadequate secretion of anti-diuretic hormone*§
Metabolic and nutritional disorders
Often – Decreased appetite, increased appetite*
Rarely – Hypercholesterolemia, diabetes mellitus*, hypoglycemia*, hyperglycemia*§, hyponatremia*§
Mental disorders
Very often – Insomnia
Often – Anxiety*, depression*, agitation*, decreased libido*, increased excitability, depersonalization, nightmares, grinding teeth in sleep*
Uncommon – Suicidal thoughts/behavior, psychotic disorders*, thought disorder, apathy, hallucinations*, aggression*, euphoria*, paranoia
Rare – Conversion disorder*§, paronyria*§ (painful dreams), drug dependence, sleepwalking, premature ejaculation
Nervous system disorders
Very common – Dizziness, headache*, drowsiness
Common – Tremor, motor dysfunction (including extrapyramidal disorders such as hyperkinesis, hypertonicity, dystonia, teeth grinding or gait disturbances), paresthesia*, hypertonicity*, impaired attention, dysgeusia
Uncommon – Amnesia, hypoesthesia*, involuntary muscle contractions*, fainting*, hyperkinesia*, migraine*, convulsions*, postural dizziness, incoordination, speech impairment
Rarely – Coma*, akathisia, dyskinesia, hyperesthesia, cerebrovascular spasm (including reversible cerebral vasoconstriction and Call-Fleming syndrome)*§, psychomotor agitation*§, sensory disturbances, choreoathetosis§, signs and symptoms associated with serotonin syndrome* or neuroleptic malignant syndrome have also been reported: agitation, impaired consciousness, diaphoresis, diarrhea, fever, arterial hypertension, muscle rigidity, tachycardia§. In some cases, these symptoms are associated with the concomitant use of serotonergic drugs.
Visual disorders
Often – Visual impairment*
Uncommon – Mydriasis*
Rarely – Scotoma, glaucoma, diplopia, photophobia, hemorrhage in the anterior chamber of the eye*§, different pupil sizes*§, visual impairment§, lacrimal apparatus disorders
Frequency unknown – Maculopathy
Disorders of the hearing organ and labyrinth
Often – Ringing in the ears*
Uncommon – Ear pain
Cardiac disorders
Often – Palpitations*
Uncommon – Tachycardia*, heart disease
Rarely – myocardial infarction*§, development of polymorphic ventricular tachycardia of the “pirouette” type (torsade de pointеs)*§, bradycardia, prolongation of the QTc interval*
Vascular disorders
Often – “Tides”*
Uncommon – Pathological bleeding (eg, gastrointestinal bleeding)*, hypertension*, flushing, hematuria*
Rarely – Peripheral ischemia
Disorders of the respiratory system, chest and mediastinal organs
Often – Yawning*
Uncommon – Dyspnea, epistaxis*, bronchospasm*
Rarely – Hyperventilation, interstitial lung disease*§, eosinophilic pneumonia*§, laryngospasm, dysphonia, stridor*§, hypoventilation, hiccups
Gastrointestinal disorders
Very common – Nausea, diarrhea, dry mouth
Often – Dyspepsia, constipation*, abdominal pain*, vomiting*, flatulence
Uncommon – Melena, dental damage, esophagitis, glossitis, hemorrhoids, increased salivation, dysphagia, belching, tongue damage
Rarely – Ulcerative lesions of the oral mucosa, pancreatitis*§, blood in the stool, ulcerative lesions of the tongue, stomatitis
Frequency unknown – Microscopic colitis*
Disorders of the liver and biliary tract
Rare – Liver dysfunction, serious liver dysfunction (including hepatitis, jaundice and liver failure)
Disorders of the skin and subcutaneous tissues
Common – Increased sweating, rash*
Uncommon – Periorbital edema*, urticaria*, alopecia*, pruritus*, purpura*, dermatitis, dry skin, facial edema, cold sweat
Rare – Rare reports of severe cutaneous adverse reactions (SCAR): e.g. Stevens-Johnson syndrome* and epidermal necrolysis*§, skin reaction*§, photosensitivity reaction§, angioedema, hair texture disorder, change in skin odor, bullous dermatitis, rash follicular
Muscle, skeletal and connective tissue disorders
Common – Back pain, arthralgia*, myalgia
Uncommon – Osteoarthritis, muscle cramps, muscle spasms*, muscle weakness
Rarely – Rhabdomyolysis*§, bone tissue disorders
Frequency unknown – Trismus*
Renal and urinary tract disorders
Uncommon – Frequent urination, urinary dysfunction, urinary retention, urinary incontinence*, polyuria, nocturia
Rarely – Urinary retention*, oliguria
Disorders of the reproductive system and mammary glands
Very common – Ejaculation disorders
Common – Menstrual irregularities*, erectile dysfunction
Uncommon – Sexual dysfunction, menorrhagia, vaginal bleeding, sexual dysfunction in women
Rarely – Galactorrhea*, atrophic vulvovaginitis, genital discharge, balanoposthitis*§, gynecomastia*, priapism*
Frequency unknown – Postpartum hemorrhage*†
General disorders and reactions at the injection site
Very common – Increased fatigue*
Common – Malaise*, chest pain*, asthenia*, pyrexia*
Uncommon – Peripheral edema*, chills, gait disturbance*, thirst
Rarely – Hernia, decreased drug tolerance
Laboratory and instrumental data
Common – Weight gain*
Uncommon – Increased activity of alanine aminotransferase*, increased activity of aspartate aminotransferase*, decreased body weight*
Rarely – elevated cholesterol levels in the blood*, abnormal laboratory parameters, abnormal properties of seminal fluid, impaired platelet function*§
Injuries, intoxications and complications of procedures
Often – Injuries
Surgical and medical procedures
Rarely – Vasodilation
* ADRs identified in the post-marketing period
§ The incidence of ADR is represented by the upper threshold value calculated at a 95% confidence interval using the “rule of 3” (the rule for finding the unknown term of the proportion).
†This phenomenon has been reported within the SSRI/SNRI therapeutic class
Withdrawal symptoms when stopping sertraline therapy
Stopping treatment with sertraline (especially abruptly) often leads to the development of withdrawal syndrome. The most commonly reported symptoms are dizziness, sensory disturbances (including paresthesia), sleep disturbances (including insomnia and vivid dreams), agitation or psychomotor agitation, nausea and/or vomiting, tremor and headache. In general, these reactions are mild, moderate and limited in nature. However, in some patients they can be severe and long-lasting. In this regard, if the patient does not need to continue treatment with sertraline, the drug should be gradually withdrawn by gradually reducing the dose.
Elderly patients
The use of SSRIs and SNRIs, including sertraline, has in some cases been associated with the development of severe hyponatremia in elderly patients, who may be at increased risk of developing this complication.
Children
In more than 600 pediatric patients treated with sertraline, the overall adverse reaction profile was generally similar to the safety profile in adult patients. In controlled studies (involving 281 patients receiving sertraline), the following adverse reactions were observed.
Very common – Headache (22%), insomnia (21%), diarrhea (11%) and nausea (15%).
Often – Chest pain, mania, pyrexia, vomiting, anorexia, affective lability, aggressive behavior, agitation, increased excitability, impaired attention, dizziness, hyperkinesia, migraine, drowsiness, tremor, blurred vision, dry oral mucosa, dyspepsia, nightmares, increased fatigue, urinary incontinence, rash, acne, nosebleeds, flatulence.
Uncommon – Prolongation of the QT interval on the ECG, suicide attempts, seizures, extrapyramidal disorders, paresthesia, depressive symptoms, hallucinations, purpura, hyperventilation, anemia, liver dysfunction, increased alanine aminotransferase (ALT), cystitis, herpes simplex, otitis, ear pain, pain in the eyeballs, mydriasis, malaise, hematuria, pustular rash, rhinitis, trauma, weight loss, involuntary muscle contractions, atypical dreams, apathy, albuminuria, pollakiuria, polyuria, chest pain, menstrual irregularities, alopecia, dermatitis, skin lesions, change in skin odor, urticaria, grinding teeth in sleep (bruxism), “flushes” of blood to the facial skin.
Frequency unknown – Enuresis
Class effects
In epidemiological studies conducted primarily in patients aged 50 years and older, there was an increased risk of bone fractures in patients taking SSRIs and tricyclic antidepressants (TCAs). The mechanism of this side effect is unknown.
Reporting suspected adverse reactions
It is important to report suspected adverse reactions after registration of a medicinal product to ensure continuous monitoring of the benefit-risk ratio of the medicinal product. Healthcare professionals are encouraged to report any suspected adverse drug reactions through the national adverse reaction reporting systems of the member states of the Eurasian Economic Union.
Interaction
Interaction
Contraindications
Monoamine oxidase inhibitors
Irreversible MAOIs (eg, selegiline)
Sertraline should not be used concomitantly with irreversible MAOIs such as selegiline. Sertraline should be prescribed no earlier than 14 days after discontinuation of irreversible MAOIs. Sertraline should be discontinued at least 7 days before starting therapy with irreversible MAOIs.
Reversible selective MAOI (moclobemide)
Due to the risk of developing serotonin syndrome, it is not recommended to take reversible selective MAOIs, such as moclobemide, and sertraline simultaneously. After using reversible MAOIs, a shorter period than 14 days may be allowed before starting sertraline. Sertraline should be discontinued at least 7 days before starting therapy with reversible MAOIs.
Reversible non-selective MAOI (linezolid)
The antibiotic linezolid is a weak, reversible, non-selective MAOI. It should not be used in patients receiving sertraline therapy.
Severe adverse reactions have been reported in patients who recently discontinued MAOI therapy and started sertraline (eg, methylene blue) or who recently stopped sertraline and started MAOI therapy. These reactions included tremor, myoclonus, diaphoresis, nausea, vomiting, facial flushing, dizziness, hyperthermia with symptoms resembling neuroleptic malignant syndrome, seizures and death.
Pimozide
According to the study, with a single dose of pimozide at a low dose (2 mg) together with sertraline, the concentration of pimozide increased by approximately 35%. This was not associated with any ECG changes. Since the mechanism of this interaction is unknown and pimozide has a narrow therapeutic index, simultaneous use of pimozide and sertraline is contraindicated.
Concomitant use of sertraline and the following drugs is not recommended
CNS depressants and alcohol
In healthy subjects, concomitant use of sertraline 200 mg daily did not potentiate the effect of alcohol, carbamazepine, haloperidol, or phenytoin on cognitive and psychomotor performance. However, drinking alcohol during treatment with sertraline is not recommended.
Other serotonergic drugs
Caution is advised when using opioids (eg, fentanyl [used during anesthesia or to treat chronic pain]) and other serotonergic drugs (including serotonergic antidepressants, amphetamines, triptans).
Special precautions
Drugs that prolong the QT interval
The risk of QTc prolongation and/or ventricular arrhythmias (eg, torsade de pointes) may be increased when sertraline is co-administered with other drugs that prolong the QTc interval (eg, some antipsychotics and antibiotics).
Lithium
According to a placebo-controlled study involving healthy volunteers, the pharmacokinetics of lithium did not change significantly when administered concomitantly with sertraline. However, an increase in tremor was noted (compared to placebo), which may indicate a possible pharmacodynamic interaction. When sertraline is used concomitantly with lithium preparations, patients should be constantly monitored.
Phenytoin
The results of a placebo-controlled study in healthy volunteers indicate that long-term use of sertraline at a dose of 200 mg per day does not have a clinically significant inhibition of phenytoin metabolism. However, there are isolated reports of increased phenytoin concentrations when used concomitantly with sertraline. Therefore, it is recommended to monitor the concentration of phenytoin in the blood plasma from the moment sertraline is prescribed with appropriate dose adjustment. In addition, during therapy with phenytoin and known CYP3A4 inducers, sertraline plasma levels may decrease.
Metamizole
The simultaneous use of sertraline with metamizole, which is an inducer of metabolizing enzymes, including CYP2B6 and CYP3A4, may reduce the concentration of sertraline in the blood plasma with a potential decrease in the clinical effectiveness of the drug. In this regard, it is recommended to exercise caution when using metamizole and sertraline simultaneously; If necessary, monitor clinical response and/or drug concentrations.
Triptans
During post-marketing use of the drug, rare cases of weakness, hyperreflexia, incoordination, confusion, anxiety and agitation have been reported in patients taking sertraline and sumatriptan at the same time. Symptoms of serotonin syndrome may also occur when used concomitantly with other drugs of the same class. If there are clinical indications for the simultaneous use of sertraline and triptans, appropriate monitoring of the patient’s condition is recommended.
Warfarin
With simultaneous use of sertraline at a dose of 200 mg per day with warfarin, a small but statistically significant increase in prothrombin time was observed, which in some cases can lead to an imbalance in the International Normalized Ratio (INR) values. In this regard, the prothrombin time should be carefully monitored during the period of initiation of sertraline therapy and during the period of drug withdrawal.
Other drug interactions (digoxin, atenolol, cimetidine)
Concomitant use of sertraline and cimetidine significantly reduces the clearance of sertraline. The clinical significance of these changes is unknown. Sertraline did not affect the β-adrenergic blocking effect of atenolol. No drug interactions have been identified between sertraline (200 mg per day) and digoxin.
Drugs affecting platelet function
An increased risk of bleeding may occur when SSRIs (including sertraline) are used concomitantly with drugs that affect platelet function (eg, NSAIDs, acetylsalicylic acid, and ticlopidine), or drugs that may increase the risk of bleeding.
Muscle relaxants (NMAC)
Selective serotonin reuptake inhibitors (SSRIs) may decrease plasma cholinesterase activity, thereby prolonging the duration of action of muscle relaxants such as mivacurium or other neuromuscular blockers on neuromuscular transmission.
Drugs metabolized by cytochrome P450
Sertraline may inhibit CYP2D6 to a mild to moderate extent. It has been established that long-term treatment with sertraline at a dose of 50 mg per day increases (on average by 23–37%) the equilibrium plasma concentration of desipramine (a marker of CYP2D6 isoenzyme activity). Clinically significant interactions are also observed with simultaneous use with drugs with a narrow therapeutic index, the metabolism of which involves the CYP2D6 isoenzyme (for example, tricyclic antidepressants, typical antipsychotics and class 1C antiarrhythmic drugs, such as propafenone and flecainide). In such cases, clinically significant drug interactions are especially common when taking high doses of sertraline.
Sertraline does not clinically significantly inhibit the isoenzymes CYP3A4, CYP2C9, CYP2C19 and CYP1A2. This has been confirmed by in vivo studies examining interactions with CYP3A4 (endogenous cortisol, carbamazepine, terfenadine, alprazolam), CYP2C19 (diazepam) and CYP2C9 (tolbutamide, glibenclamide and phenytoin) substrates. In vitro studies indicate that sertraline has little or no inhibitory effect on CYP1A2 activity.
Drinking three glasses of grapefruit juice daily increased plasma sertraline concentrations by approximately 100% (according to a crossover study in eight healthy Japanese subjects). Therefore, concomitant use of sertraline and grapefruit juice should be avoided.
Based on interaction studies between sertraline and grapefruit juice, it cannot be excluded that concomitant use of sertraline and strong CYP3A4 inhibitors (e.g. protease inhibitors, ketoconazole, itraconazole, posaconazole, voriconazole, clarithromycin, telithromycin and nefazodone) may result in an even greater increase in sertraline exposure. This also applies to moderate CYP3A4 inhibitors (such as aprepitant, erythromycin, fluconazole, verapamil and diltiazem). Thus, the use of potent inhibitors of the CYP3A4 isoenzyme should be avoided during sertraline therapy. It is also impossible to exclude the ability of other inducers of the CYP3A4 isoenzyme (for example, phenobarbital, carbamazepine, St. John’s wort preparations, rifampicin) to reduce the concentration of sertraline in the blood plasma. In patients who slowly metabolize the CYP2C19 isoenzyme, there is an increase in the concentration of sertraline in the blood plasma. blood plasma is 50% higher than in patients who rapidly metabolize this enzyme. An interaction between potent inhibitors of the CYP2C19 isoenzyme (such as omeprazole, lansoprazole, pantoprazole, rabeprazole, fluoxetine and fluvoxamine) and sertraline cannot be excluded.
Overdose
Overdose
Toxicity
The safety of sertraline depends on the patient population and/or the concomitant drug taken. Cases of death associated with sertraline overdose have been reported when taking the drug alone or in combination with other drugs and/or alcohol. In this regard, it is necessary to carry out intensive therapy for any overdose of sertraline.
Symptoms
Symptoms of overdose include serotonin-mediated side effects such as drowsiness, gastrointestinal disturbances (eg, nausea and vomiting), tachycardia, tremor, restlessness, and dizziness. In some cases, the development of coma was noted.
Overdose can cause serotonin syndrome with prolongation of the QTc interval, the development of torsade de pointes (TdP), therefore, in case of sertraline overdose, it is recommended to monitor ECG parameters.
Treatment
There is no specific antidote for sertraline. It is recommended to establish and maintain a patent airway and, if necessary, provide adequate levels of oxygenation and respiratory function. Administration of activated charcoal along with a laxative may be more effective than gastric lavage, so its use should be considered in the treatment of overdose. Inducing vomiting is not recommended. It is recommended to monitor cardiac vital signs (eg, ECG) and other vital signs, as well as general symptomatic and supportive care. Sertraline has a large volume of distribution, so forced diuresis, dialysis, hemoperfusion or blood transfusion may not be effective.
Storage conditions
Storage conditions
Store at a temperature not exceeding 30 °C.
Shelf life
Shelf life
5 years.
Do not use after the expiration date stated on the package.
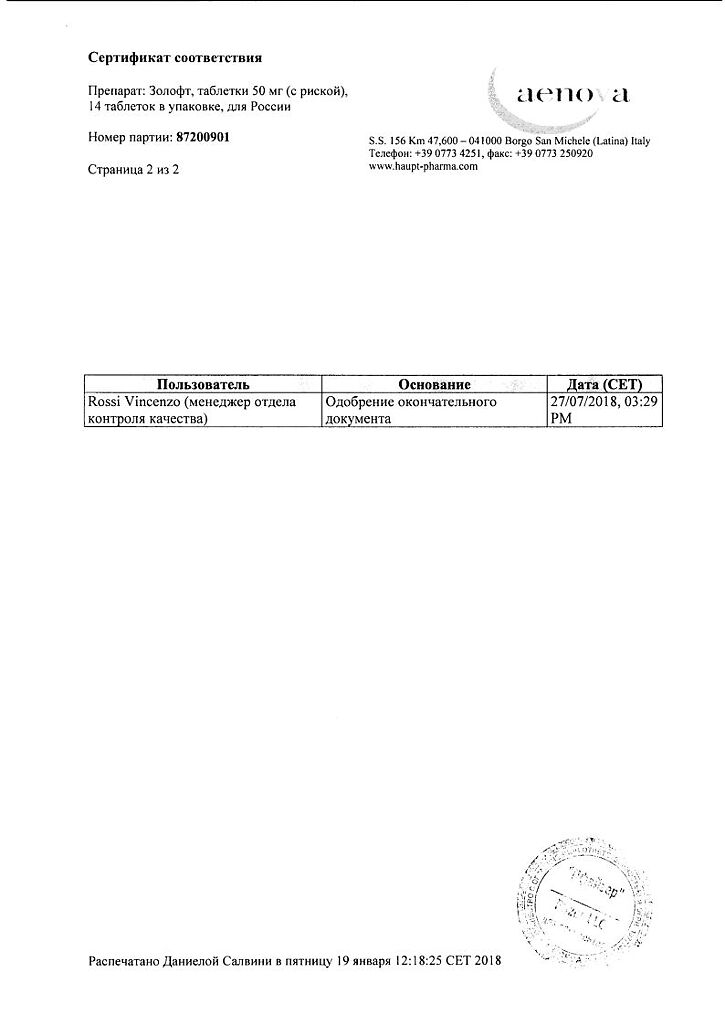
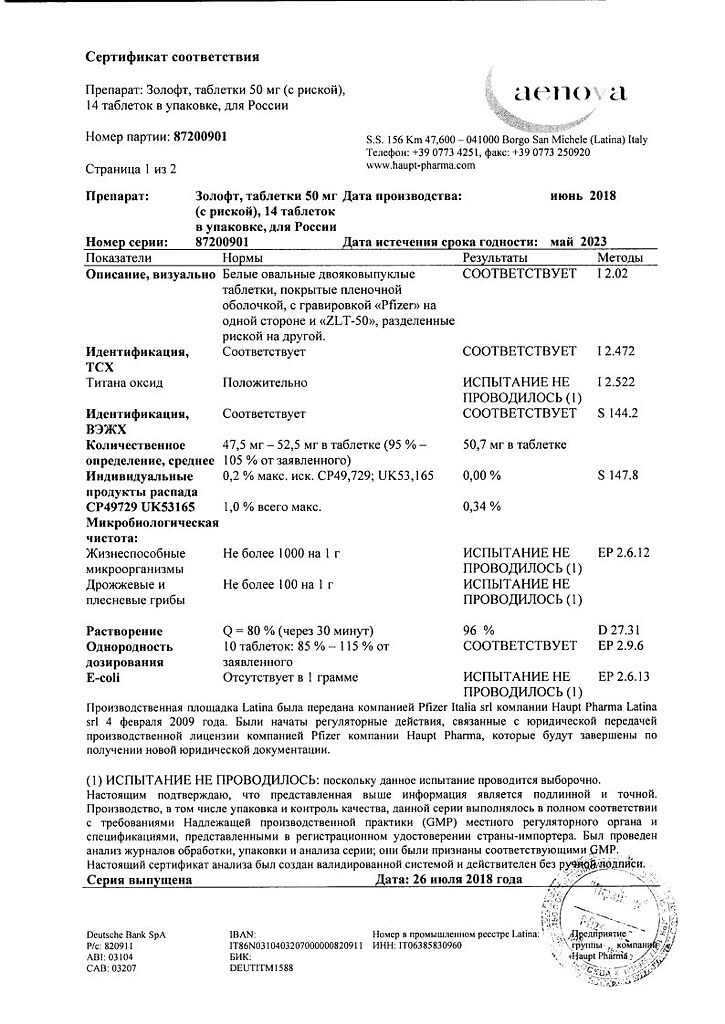
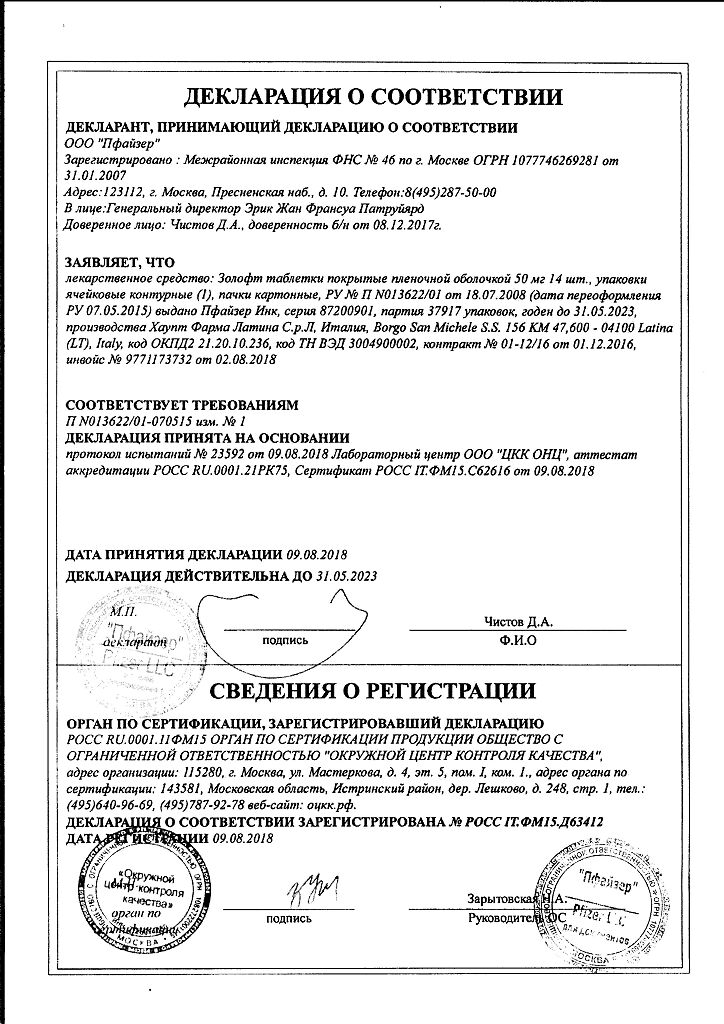
Manufacturer
Manufacturer
Pfizer Manufacturing Deutschland GmbH, Germany
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 30 °C |
| Manufacturer | Pfizer Manufacturing Deutschland GmbH, Germany |
| Medication form | pills |
| Brand | Pfizer Manufacturing Deutschland GmbH |
Related products
Buy Zoloft, 50 mg 14 pcs with delivery to USA, UK, Europe and over 120 other countries.