No products in the cart.
Yarin, 3 mg+0.03 mg 21 pcs
€40.25 €33.54
EAN: 4029668001071
SKU: 206518
Categories: Contraceptive, Gynecology and Obstetrics, Hormonal, Medicine
Description
Yarina is a low-dose monophasic combined contraceptive with anti-mineralocorticoid and anti-androgenic properties. It inhibits the secretion of gonadotropic hormones of the pituitary gland, inhibits the maturation of follicles and prevents ovulation. It increases the viscosity of cervical mucus, which makes it difficult for sperm to enter the uterus.
Drospirenone has anti-mineralocorticoid action and can prevent weight gain and other symptoms associated with fluid retention in the body.
It prevents sodium retention caused by estrogens, provides very good tolerance and has a positive effect in premenstrual syndrome. In combination with ethinylestradiol, drospirenone improves the lipid profile and increases HDL levels.
Drospirenone has antiadrogenic activity and helps to reduce the appearance of acne and reduce sebum production. It does not counteract the ethinyl estradiol-induced increase in sex hormone binding globulin (hSPH) levels, which contributes to the binding and inactivation of endogenous androgens.
Drospirenone does not have any androgenic, estrogenic, glucocorticoid or antiglucocorticoid activity, which in combination with its anti-mineralocorticoid and anti-androgenic actions gives drospirenone a biochemical and pharmacological profile very similar to natural progesterone. There is evidence for a reduced risk of endometrial and ovarian cancer.
In the background of using the drug Yarina menstrual cycle becomes more regular, painful menstruation is less often observed, the intensity of menstrual discharge decreases, as a result of which the risk of iron deficiency anemia is reduced.
Indications
Indications
Hormonal contraception.
The drug is recommended for use for acne and seborrhea, as well as for hormone-dependent fluid retention in the body.
Pharmacological effect
Pharmacological effect
Yarina is a low-dose monophasic combined contraceptive drug with antimineralocorticoid and antiandrogenic properties. Inhibits the secretion of gonadotropic hormones of the pituitary gland, inhibits the maturation of follicles and prevents the ovulation process. Increases the viscosity of cervical mucus, which makes it difficult for sperm to penetrate the uterus.
Drospirenone has an antimineralocorticoid effect and is able to prevent weight gain and other symptoms associated with fluid retention in the body.
Prevents sodium retention caused by estrogen, provides very good tolerability and has a positive effect on premenstrual syndrome. In combination with ethinyl estradiol, drospirenone improves the lipid profile and increases HDL levels.
Drospirenone has antiadrogenic activity and helps reduce the appearance of acne and reduce the production of sebaceous glands. Does not counteract the ethinyl estradiol-induced increase in sex hormone binding globulin (SHBG), which promotes the binding and inactivation of endogenous androgens.
Drospirenone does not have any androgenic, estrogenic, glucocorticoid and antiglucocorticoid activity, which, in combination with antimineralocorticoid and antiandrogenic effects, provides drospirenone with a biochemical and pharmacological profile very close to natural progesterone. There is evidence of a reduced risk of endometrial and ovarian cancer.
With the use of the drug Yarina, the menstrual cycle becomes more regular, painful menstruation is observed less frequently, the intensity of menstrual flow decreases, resulting in a reduced risk of developing iron deficiency anemia.
Special instructions
Special instructions
If any of the conditions, diseases and risk factors listed below currently exist, the potential risks and expected benefits of combined oral contraceptives should be carefully weighed in each individual case and discussed with the woman before she decides to start taking the drug.
In case of worsening, intensification or first manifestation of any of these conditions, diseases or increase in risk factors, the woman should consult with her doctor, who may decide whether to discontinue the drug.
Diseases of the cardiovascular system
The results of epidemiological studies indicate a relationship between the use of combined oral contraceptives and an increased incidence of venous and arterial thrombosis and thromboembolism (such as deep vein thrombosis, pulmonary embolism, myocardial infarction, cerebrovascular disorders) when taking combined oral contraceptives. These diseases are rare.
The risk of developing VTE is greatest in the first year of taking such drugs. An increased risk is present after initial use of combined oral contraceptives or resumption of use of the same or different combined oral contraceptives (after a dosing interval of 4 weeks or more). Data from a large prospective study involving 3 groups of patients indicate that this increased risk is predominantly present during the first 3 months.
The overall risk of VTE in patients taking low-dose combined oral contraceptives (ethinyl estradiol content less than 50 mcg) is 2-3 times higher than in non-pregnant patients not taking combined oral contraceptives, however, this risk remains lower than the risk of VTE during pregnancy and childbirth. VTE can be life-threatening or fatal (in 1–2% of cases).
VTE, manifested as deep vein thrombosis or pulmonary embolism, can occur with the use of any combined oral contraceptives.
Very rarely, when using combined oral contraceptives, thrombosis of other blood vessels (for example, hepatic, mesenteric, renal, cerebral veins and arteries or retinal vessels) occurs. There is no consensus regarding the relationship between the occurrence of these events and the use of combined oral contraceptives.
Symptoms of deep vein thrombosis (DVT) include the following: unilateral swelling of the lower extremity or along a vein in the leg, pain or discomfort in the leg only when standing up or when walking, localized warmth in the affected leg, redness or discoloration of the skin on the leg.
Symptoms of pulmonary embolism (PE) include: difficulty or rapid breathing; sudden cough, incl. with hemoptysis; sharp pain in the chest, which may intensify with deep inspiration; feeling of anxiety; severe dizziness; fast or irregular heartbeat.
Some of these symptoms (eg shortness of breath, cough) are non-specific and may be misinterpreted as signs of other more or less serious events (eg respiratory tract infection).
Arterial thromboembolism can lead to stroke, vascular occlusion, or myocardial infarction. Symptoms of a stroke include: sudden weakness or loss of feeling in the face, arm or leg, especially on one side of the body, sudden confusion, problems with speech and comprehension; sudden unilateral or bilateral vision loss; sudden disturbance in gait, dizziness, loss of balance or coordination; sudden, severe or prolonged headache for no apparent reason; loss of consciousness or fainting with or without an epileptic seizure.
Other signs of vascular occlusion: sudden pain, swelling and slight blue discoloration of the extremities, acute abdomen.
Symptoms of myocardial infarction include: pain, discomfort, pressure, heaviness, a feeling of squeezing or fullness in the chest, arm, or chest; discomfort radiating to the back, cheekbone, larynx, arm, stomach; cold sweat, nausea, vomiting or dizziness, severe weakness, anxiety or shortness of breath; fast or irregular heartbeat. Arterial thromboembolism can be fatal. The risk of developing thrombosis (venous and/or arterial) and thromboembolism increases:
– with age;
– in smokers (with an increase in the number of cigarettes or an increase in age, the risk increases, especially in women over 35 years of age).
If available:
– obesity (body mass index more than 30 kg/m2);
– family history (for example, venous or arterial thromboembolism ever in close relatives or parents at a relatively young age). In the case of a hereditary or acquired predisposition, the woman should be examined by an appropriate specialist to decide on the possibility of taking combined oral contraceptives;
– prolonged immobilization, major surgery, any leg surgery or major trauma. In these situations, it is advisable to stop using combined oral contraceptives (in the case of planned surgery, at least 4 weeks before it) and not resume use for 2 weeks after the end of immobilization;
– dislipoproteinemia;
– arterial hypertension;
– migraine;
– diseases of the heart valves;
– atrial fibrillation.
The possible role of varicose veins and superficial thrombophlebitis in the development of venous thromboembolism remains controversial. The increased risk of thromboembolism in the postpartum period should be taken into account.
Poor peripheral circulation may also occur in diabetes mellitus, systemic lupus erythematosus, hemolytic uremic syndrome, chronic inflammatory bowel disease (Crohn’s disease or ulcerative colitis) and sickle cell anemia. An increase in the frequency and severity of migraine during use of combined oral contraceptives (which may precede cerebrovascular events) may be grounds for immediate discontinuation of these drugs.
Biochemical indicators indicating a hereditary or acquired predisposition to venous or arterial thrombosis include the following: resistance to activated protein C, hyperhomocysteinemia, antithrombin-III deficiency, protein C deficiency, protein S deficiency, antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant). When assessing the risk-benefit ratio, it should be taken into account that adequate treatment of the relevant condition may reduce the associated risk of thrombosis. It should also be taken into account that the risk of thrombosis and thromboembolism during pregnancy is higher than when taking low-dose oral contraceptives (ethinyl estradiol content – 0.05 mg).
Tumors
The most significant risk factor for developing cervical cancer is persistent human papillomavirus infection. There are reports of a slight increase in the risk of developing cervical cancer with long-term use of combined oral contraceptives. However, the connection with the use of combined oral contraceptives has not been proven. The possibility of interrelating these data with disease screening is discussed. Controversy remains regarding the extent to which these findings are related to screening for cervical pathology or to sexual behavior (lower use of barrier methods of contraception).
A meta-analysis of 54 epidemiological studies found that there is a slightly increased relative risk of developing breast cancer diagnosed in women currently taking combined oral contraceptives (relative risk – 1.24).
The increased risk gradually disappears within 10 years of stopping these drugs. Because breast cancer is rare in women under 40 years of age, the increase in breast cancer diagnoses in women currently or recently taking combined oral contraceptives is small relative to the overall risk of breast cancer.
Its connection with the use of combined oral contraceptives has not been proven. The observed increased risk may also be a consequence of careful monitoring and earlier diagnosis of breast cancer in women using combined oral contraceptives. Women who have ever used combined oral contraceptives are diagnosed with earlier stages of breast cancer than women who have never used them.
In rare cases, during the use of combined oral contraceptives, the development of benign, and in extremely rare cases, malignant liver tumors, which sometimes led to life-threatening intra-abdominal bleeding, was observed. In case of severe abdominal pain, liver enlargement or signs of intra-abdominal bleeding, this should be taken into account when making a differential diagnosis. Malignant tumors can be life-threatening or fatal.
Other states
Clinical studies have shown no effect of drospirenone on plasma potassium concentrations in patients with mild to moderate renal failure. However, in patients with impaired renal function and an initial potassium concentration at the ULN level, the risk of developing hyperkalemia cannot be excluded while taking drugs that lead to potassium retention in the body.
Women with hypertriglyceridemia (or a family history of this condition) may have an increased risk of developing pancreatitis while taking combined oral contraceptives.
Although slight increases in blood pressure have been described in many women taking combined oral contraceptives, clinically significant increases have rarely been observed. However, if a persistent, clinically significant increase in blood pressure develops while taking the drug, these drugs should be discontinued and treatment of arterial hypertension should be initiated. The drug can be continued if normal blood pressure values are achieved with antihypertensive therapy.
The following conditions have been reported to develop or worsen both during pregnancy and while taking combined oral contraceptives (but have not been shown to be associated with combined oral contraceptives): jaundice and/or pruritus associated with cholestasis; formation of gallstones; porphyria; systemic lupus erythematosus; hemolytic uremic syndrome; chorea; herpes during pregnancy; hearing loss associated with otosclerosis.
Cases of Crohn’s disease and ulcerative colitis have also been described during the use of combined oral contraceptives. In women with hereditary forms of angioedema, exogenous estrogens may cause or worsen symptoms of angioedema.
Acute or chronic liver dysfunction may require discontinuation of the drug until liver function tests return to normal. Recurrent cholestatic jaundice, which develops for the first time during pregnancy or previous use of sex hormones, requires discontinuation of the drug.
Although combined oral contraceptives may have an effect on insulin resistance and glucose tolerance, there is no need to change the therapeutic regimen in diabetic patients using low-dose combined oral contraceptives (ethinyl estradiol content less than 0.05 mg).
However, women with diabetes should be closely monitored while taking this drug.
Chloasma can sometimes develop, especially in women with a history of pregnancy chloasma. Women with a tendency to chloasma while taking Yarina® should avoid prolonged exposure to the sun and exposure to UV radiation.
Preclinical safety data
Preclinical data from routine repeated-dose toxicity, genotoxicity, carcinogenicity and reproductive toxicity studies do not indicate a particular risk to humans. However, it should be remembered that sex steroids can promote the growth of certain hormone-dependent tissues and tumors.
Laboratory tests
Taking combined oral contraceptives may affect the results of some laboratory tests, including liver, kidney, thyroid, adrenal function, plasma transport protein levels, carbohydrate metabolism, blood coagulation and fibrinolysis. Changes usually do not go beyond normal values. Drospirenone increases plasma renin activity and plasma aldosterone levels, which is associated with its antimineralocorticoid effect.
Reduced efficiency
The effectiveness of Yarina® may be reduced in the following cases: if you miss taking pills, with vomiting and diarrhea (see “Taking missed pills”) or as a result of drug interactions.
Insufficient control of the menstrual cycle
While taking Yarina®, irregular (acyclic) spotting/bleeding from the vagina (spotting or breakthrough bleeding) may occur, especially during the first months of use.
Therefore, evaluation of any irregular menstrual-like bleeding should be carried out after an adaptation period of approximately 3 cycles. If irregular menstrual-like bleeding recurs or develops after previous regular cycles, a thorough examination should be performed to rule out malignancy or pregnancy.
Some women may not develop withdrawal bleeding during a pill-free break. If Yarina® is taken as recommended, it is unlikely that the woman is pregnant. However, if the drug is not used regularly and there are no two consecutive menstrual-like bleedings, the drug cannot be continued until pregnancy has been ruled out.
Medical examinations
Before starting or resuming the use of the drug Yarina®, it is necessary to familiarize yourself with the woman’s life history and family history, conduct a thorough general medical and gynecological examination, and exclude pregnancy. The scope of research and the frequency of follow-up examinations should be based on existing standards of medical practice, with the necessary consideration of the individual characteristics of each patient. As a rule, blood pressure and heart rate are measured, body mass index is determined, the condition of the mammary glands, abdominal cavity and pelvic organs is checked, including a cytological examination of the cervical epithelium (Papanicolaou test). Typically, follow-up examinations should be carried out at least once every 6 months.
A woman should be warned that hormonal contraceptives do not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Impact on the ability to drive a car or perform work that requires increased speed of physical and mental reactions. Not identified.
Active ingredient
Active ingredient
Drospirenone, Ethinylestradiol
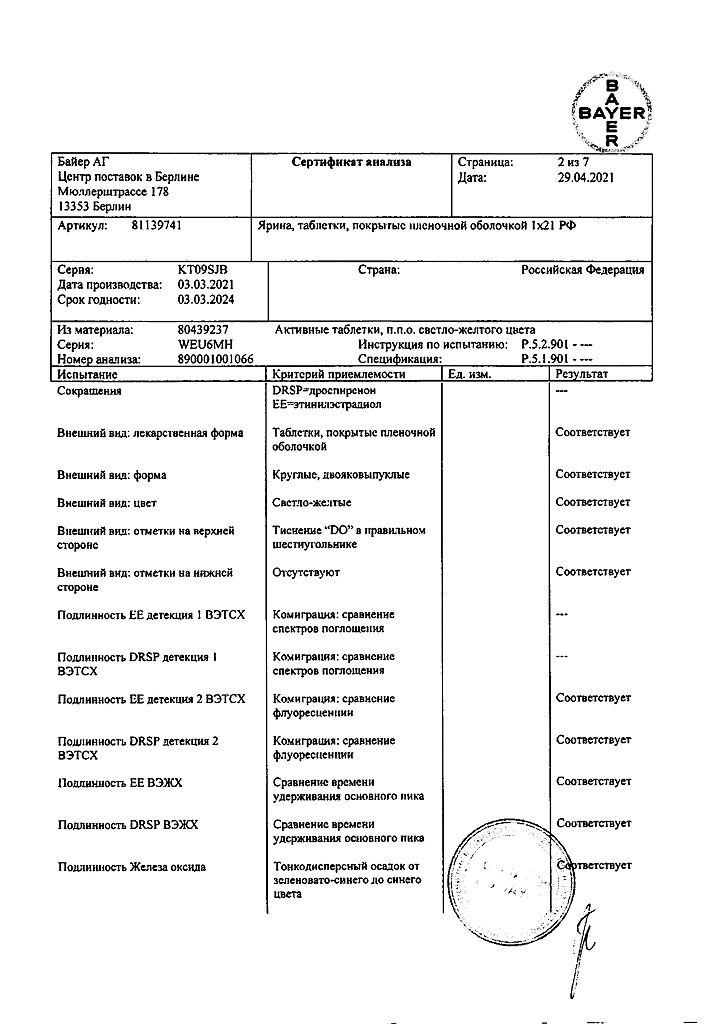
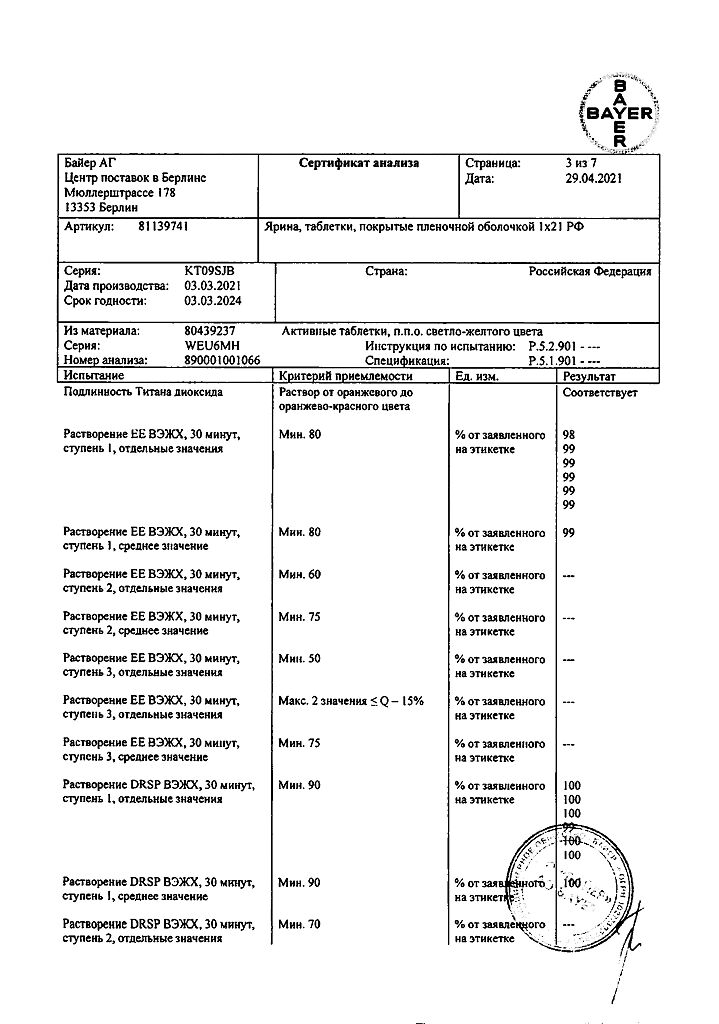
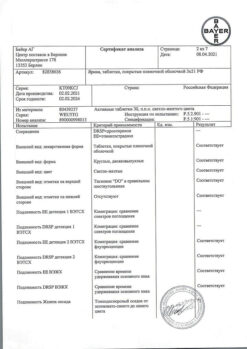
Composition
Composition
1 tablet contains:
active substances:
drospirenone 3 mg,
ethinyl estradiol 0.03 mg;
excipients:
lactose monohydrate – 48.17 mg;
corn starch – 14.4 mg;
pregelatinized corn starch – 9.6 mg;
povidone K25 – 4 mg;
magnesium stearate – 800 mcg;
hypromellose (hydroxypropyl methylcellulose) – 1.0112 mg;
macrogol 6000 – 202.4 mcg;
talc (magnesium hydrosilicate) – 202.4 mcg;
titanium dioxide (E171) – 556.5 μg;
iron (II) oxide (E172) – 27.5 μg
Pregnancy
Pregnancy
The drug is not prescribed during pregnancy and breastfeeding. If pregnancy is detected while taking Yarina®, it should be discontinued immediately.
However, extensive epidemiological studies have not revealed an increased risk of developmental defects in children born to women who received sex hormones before pregnancy or teratogenic effects in cases of inadvertent use of sex hormones in early pregnancy.
At the same time, data on the results of taking Yarina® during pregnancy are limited, which does not allow us to draw any conclusions about the negative impact of the drug on pregnancy, the health of the newborn and the fetus. Currently, no significant epidemiological data are available.
Taking combined oral contraceptives may reduce the amount of breast milk and change its composition, so their use is not recommended until you stop breastfeeding. Small amounts of sex steroids and/or their metabolites may be excreted in milk.
Contraindications
Contraindications
– presence of thrombosis (venous and arterial) currently or in history (for example, deep vein thrombosis, pulmonary embolism, myocardial infarction, cerebrovascular disorders);
– the presence or history of conditions preceding thrombosis (for example, transient cerebrovascular accidents, angina pectoris);
– diabetes mellitus with vascular complications;
– presence of severe or multiple risk factors for venous or arterial thrombosis;
– current or history of severe forms of liver disease (until liver test results are normalized);
– presence or history of benign or malignant liver tumors;
– identified or suspected hormone-dependent malignant diseases of the genital organs or mammary glands;
– severe or acute renal failure;
– vaginal bleeding of unknown origin;
– pregnancy or suspicion of it;
– lactation (breastfeeding);
– hypersensitivity to the components of the drug.
Side Effects
Side Effects
The most commonly reported adverse reactions to Yarina® include nausea and breast pain. They occurred in more than 6% of women using this drug.
Serious adverse reactions include arterial and venous thromboembolism.
The table below shows the frequency of adverse reactions. which were reported during clinical trials of the drug Yarina® (N=4897). Within each group, allocated depending on the frequency of occurrence of an adverse reaction, adverse reactions are presented in order of decreasing severity. By frequency they are divided into frequent (≥1/100 and
Table 1
Systemic organ classes (MedDRA version) Often Uncommon Rare Frequency unknown Psychiatric disorders Mood swings, depression, depressed mood, decreased or loss of libido Nervous system Migraine Vascular disorders Venous or arterial thromboembolism* Gastrointestinal tract Nausea Skin and subcutaneous tissues Erythema multiforme Reproductive system and mammary glands Breast pain, Irregular uterine bleeding, bleeding from the genital tract of unspecified origin. Breast hypertrophy. Vaginal discharge, discharge from the mammary glands.
Adverse events during clinical trials were codified using the MedDRA dictionary (Medical Dictionary for Regulatory Activities, version 12.1). Different MedDRA terms reflecting the same symptom were grouped together and presented as a single adverse reaction to avoid diluting or diluting the true effect.
* – Approximate frequency based on the results of epidemiological studies covering the group of combined oral contraceptives. The frequency bordered on very rare.
– Venous or arterial thromboembolism includes the following entities: peripheral deep vein occlusion, thrombosis and embolism/pulmonary vascular occlusion, thrombosis, embolism and infarction/myocardial infarction/cerebral infarction and stroke not defined as hemorrhagic.
For venous and arterial thromboembolism, migraine, see also “Contraindications” and “Special instructions”.
Additional information
Listed below are adverse reactions with a very rare incidence or with delayed symptoms, which are believed to be associated with taking drugs from the group of combined oral contraceptives (see also “Contraindications” and “Special instructions”).
Tumors:
– The incidence of breast cancer diagnosis in women taking combined oral contraceptives is slightly increased. Because breast cancer is rare in women under 40 years of age, the increase in breast cancer diagnoses in women taking combined oral contraceptives is small relative to the overall risk of breast cancer.
– liver tumors (benign and malignant).
Other states:
– erythema nodosum;
– women with hypertriglyceridesmia (increased risk of pancreatitis while taking combined oral contraceptives);
– increased blood pressure;
– conditions that develop or worsen while taking combined oral contraceptives, but their connection with taking the drug has not been proven (jaundice and/or itching associated with cholestasis; formation of gallstones; porphyria; systemic lupus erythematosus; hemolytic-uremic syndrome; Sydenham’s chorea; herpes of pregnancy; hearing loss associated with otosclerosis);
– in women with hereditary angioedema, taking estrogens can cause or aggravate its symptoms;
– liver dysfunction;
– impaired glucose tolerance or effect on insulin resistance;
– Crohn’s disease, ulcerative colitis;
– chloasma;
– hypersensitivity (including symptoms such as rash, urticaria).
Interaction
Interaction
Interaction of oral contraceptives with other drugs may lead to breakthrough bleeding and/or decreased contraceptive reliability. Women taking these drugs should temporarily use barrier methods of contraception in addition to Yarina®, or choose another method of contraception.
The following types of interactions have been reported in the literature.
Effect on hepatic metabolism. The use of drugs that induce liver microsomal enzymes can lead to an increase in the clearance of sex hormones, which in turn can lead to breakthrough bleeding or reduced contraceptive reliability. These drugs include: phenytoin, barbiturates, primidone, carbamazepine, rifampicin, rifabutin, possibly also oxcarbazepine, topiramate, felbamate, griseofulvin and preparations containing St. John’s wort.
HIV protease inhibitors (eg ritonavir) and non-nucleoside reverse transcriptase inhibitors (eg nevirapine) and combinations thereof also have the potential to affect hepatic metabolism.
Effect on enterohepatic circulation. According to individual studies, some antibiotics (for example, penicillins and tetracyclines) may reduce the enterohepatic circulation of estrogens, thereby lowering the concentration of ethinyl estradiol.
While taking medications that affect microsomal enzymes, and for 28 days after their discontinuation, you should additionally use a barrier method of contraception.
While taking antibiotics (such as penicillins and tetracyclines) and for 7 days after their discontinuation, you should additionally use a barrier method of contraception. If during these 7 days of the barrier method of contraception the tablets in the current package run out, then you should start taking tablets from the next package of Yarina® without the usual break in taking the tablets.
The main metabolites of drospirenone are formed in plasma without the participation of the cytochrome P450 system. Therefore, the effect of inhibitors of the cytochrome P450 system on the metabolism of drospirenone is unlikely.
Oral combination contraceptives may affect the metabolism of other drugs, leading to an increase (for example, cyclosporine) or a decrease (for example, lamotrigine) in their plasma and tissue concentrations.
Based on in vitro interaction studies, as well as an in vivo study in female volunteers taking omeprazole, simvastatin and midazolam as markers, it can be concluded that the effect of drospirenone 3 mg on the metabolism of other medicinal substances is unlikely.
There is a theoretical possibility of an increase in serum potassium levels in women receiving Yarina® concomitantly with other drugs that can increase serum potassium levels. These drugs include angiotensin II receptor antagonists, some anti-inflammatory drugs, potassium-sparing diuretics, and aldosterone antagonists. However, in studies evaluating the interaction of drospirenone with ACE inhibitors or indomethacin, there was no significant difference in serum potassium concentrations compared with placebo.
Overdose
Overdose
Symptoms (identified based on cumulative experience with oral contraceptives): nausea, vomiting, spotting or metrorrhagia.
Treatment: symptomatic. There is no specific antidote.
No serious adverse events have been reported following overdose.
Storage conditions
Storage conditions
At room temperature no higher than 25 °C
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Bayer AG, Germany
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At room temperature not higher than 25 °C |
| Manufacturer | Bayer Weimar GmbH & Co. KG, Germany |
| Medication form | pills |
| Brand | Bayer Weimar GmbH & Co. KG |
Other forms…
Related products
Gynecology and Obstetrics
Buy Yarin, 3 mg+0.03 mg 21 pcs with delivery to USA, UK, Europe and over 120 other countries.