No products in the cart.
Xalatan, eye drops 0.005% 2.5ml 3 pcs.
€50.97 €44.18
Description
Pharmacodynamics
Latanoprost, an analogue of prostaglandin F2α, is a selective FP (prostaglandin F) receptor agonist and reduces intraocular pressure (IOP) by increasing aqueous outflow, mainly via uveoscleral and trabecular network. IOP reduction starts approximately 3-4 hours after the drug is injected, the maximum effect is observed after 8-12 hours, the action lasts for at least 24 hours. It is established that latanoprost has no significant effect on aqueous humor production and hemato-ophthalmic barrier.
When used in therapeutic doses latanoprost has no significant pharmacological effect on cardiovascular and respiratory systems.
Pharmacokinetics
Absorption
Latanoprost, being a prodrug, is absorbed through the cornea, where its hydrolysis to bioactive acid occurs. Its concentration in aqueous humor reaches a maximum about two hours after topical application.
Distribution
The volume of distribution is 0.16 ± 0.02 L/kg. Latanoprost acid is detected in aqueous humor during the first 4 hours and in plasma only during the first hour after topical administration.
Metabolism
Latanoprost, being a prodrug, undergoes hydrolysis in the cornea by esterases to form bioactive acid. Latanoprost acid entering the systemic blood flow is metabolized mainly in the liver by beta-oxidation of fatty acids with the formation of 1,2-dinor- and 1,2,3,4-tetranor-metabolites.
Excretion
Latanoprost acid is quickly eliminated from the plasma (t1/2 =17 min). Systemic clearance is approximately 7 ml/min/kg. After beta-oxidation in the liver, metabolites are excreted mainly by the kidneys: after topical administration approximately 88% of the administered dose is excreted with the urine.
Children
Latanoprost exposure is approximately 2 times higher in children aged 3 to 12 years compared to adult patients and 6 times higher in children younger than 3 years. However, the safety profile of the drug does not differ between children and adults.
The time to reach the maximum plasma concentration of latanoprost acid is 5 minutes for all age groups. The elimination half-life of latanoprost acid in children is the same as in adults. No cumulation of latanoprost acid in plasma occurs at equilibrium concentration.
Indications
Indications
Reduction of elevated intraocular pressure (IOP) in adult patients (including elderly patients) with open-angle glaucoma and increased ophthalmotonus.
Reducing elevated IOP in children with elevated IOP and glaucoma.
Pharmacological effect
Pharmacological effect
Mechanism of action
The active substance latanoprost is an analogue of prostaglandin F2a and is a selective agonist of prostanoid FP receptors, which reduces IOP by increasing the outflow of intraocular fluid. In humans, IOP begins to decrease approximately 3 to 4 hours after administration of the drug; the maximum effect is achieved after 8 – 12 hours. The reduction in IOP lasts for at least 24 hours.
Animal and human studies indicate that the primary mechanism of action is an increase in uveoscleral outflow, and a slight increase in outflow capacity (decreased outflow resistance) has also been described in humans.
Clinical efficacy and safety
Pivotal studies have shown that Xalatan is effective when used as monotherapy. In addition, clinical studies evaluated the use of the drug as part of combination therapy. These include, among other things, studies demonstrating the effectiveness of latanoprost in combination with beta-adrenergic receptor antagonists (timolol). Short-term studies (1 or 2 weeks) suggest that the effect of latanoprost is additive when used in combination with an adrenergic agonist (dipivalyl epinephrine), an oral carbonic anhydrase inhibitor (acetazolamide) and, at least partially, additive when used with a cholinergic agonist (pilocarpine).
Clinical studies have shown that latanoprost does not have a significant effect on the production of intraocular fluid. No effect of latanoprost on the blood-ophthalmic barrier was detected.
In monkeys and at clinical doses, latanoprost has little, if any, effect on intraocular circulation. However, when applied topically, mild to moderate conjunctival or episcleral hyperemia may develop.
According to fluorescein angiography, long-term local treatment with latanoprost in monkeys after extracapsular cataract extraction had no effect on the retinal blood vessels.
When used short-term in pseudophakic patients, latanoprost did not promote fluorescein leakage into the posterior segment of the eye.
When using latanoprost in clinical doses, no significant pharmacological effects on the cardiovascular and respiratory systems were observed.
Children
The effectiveness of Xalatan in pediatric patients ≤ 18 years of age was demonstrated in a 12-week, double-blind clinical trial in which latanoprost was compared with timolol in 107 patients with ocular hypertension and childhood glaucoma. Infants were required to be at least 36 weeks gestational age. Patients were randomized to receive either latanoprost 50 mcg/mL once daily or timolol 0.5% (or timolol 0.25% for patients <3 years of age) twice daily. The primary efficacy endpoint was the mean reduction in IOP from baseline after 12 weeks of treatment. The mean reduction in IOP was similar in the 2 treatment groups (latanoprost and timolol). In all age groups studied (0 to <3 years, 3 to <12 years, and 12 to 18 years), the mean reduction in IOP after 12 weeks of treatment in the latanoprost group was the same as in the timolol group. However, data on the effectiveness of latanoprost in the age group from 0 to <3 years were obtained for only 13 patients, and for 4 patients who represented the age group from 0 to <1 year, corresponding effectiveness was not demonstrated. There are no data available for use in premature infants (less than 36 weeks' gestational age).
Similarly, IOP reduction in patients with primary congenital glaucoma (PCG) was similar in the 2 treatment groups (latanoprost and timolol). Similar results were observed in another subgroup (non-primary congenital glaucoma, eg: juvenile open-angle glaucoma, aphakic glaucoma).
The reduction in IOP observed after the first week of treatment (see table) was maintained throughout the 12 weeks of the study, the same as in adults.
Table. IOP reduction (mmHg) after 12 weeks by active treatment group and initial diagnosis.
Power-on average (SD):
Latanoprost N=53: 27.3 (0.75)
Timolol N=54: 27.8 (0.84)
Mean change from baseline after 12 weeks of treatment† (SD):
Latanoprost N=53: –7.18 (0.81)
Timolol N=54: –5.72 (0.81)
p-values compared with timolol treatment group:
Latanoprost N=53: 0.2056
Power-on average (SD):
PVG N=28: 26.5 (0.72)
Not PVG N=25: 28.2 (1.37)
PVG N=26: 26.3 (0.95)
Non-PVG N=28: 29.1 (1.33)
Mean change from baseline after 12 weeks of treatment† (SD):
PVG N=28: –5.90 (0.98)
Not PVG N=25: –8.66 (1.25)
PVG N=26: –5.34 (1.02)
Non-PVG N=28: –6.02 (1.18)
p-values compared with timolol treatment group:
PVG N=28: 0.6957
Not PVG N=25: 0.1317
SD – standard deviation.
†Adjusted estimate based on analysis of covariance (ANCOVA) model.
Absorption
Latanoprost (molecular weight 432.58) is an isopropyl ether and is a prodrug that is inactive by itself, but after hydrolysis to acid, latanoprost becomes biologically active.
The prodrug is well absorbed through the cornea and, completely hydrolyzed during passage through it, enters the intraocular fluid.
Distribution
Human studies indicate that concentrations in aqueous humor reach a maximum approximately two hours after topical application. Following topical administration in monkeys, latanoprost is primarily distributed in the anterior segment of the eye, conjunctiva, and eyelids. Only a small part of the drug reaches the posterior segment of the eye.
Biotransformation and elimination
In the eye, latanoprost in acid form undergoes virtually no metabolic transformation. Metabolism occurs mainly in the liver. The plasma half-life in humans is approximately 17 minutes. In animal studies, the primary metabolites, 1,2-dinor and 1,2,3,4-tetranor metabolites, had little or no biological activity and were primarily excreted in urine.
Children
An open-label pharmacokinetic study was conducted to study plasma concentrations of latanoprost acid in 22 adult patients and 25 pediatric patients (age from birth to <18 years) with intraocular hypertension and glaucoma. Patients of all age groups were treated with latanoprost at a dosage of 50 mcg/ml, one drop daily in each eye for a minimum of 2 weeks. Systemic exposure to latanoprost acid in children aged 3 to <12 years was approximately 2 times higher than in adult patients, and in children aged <3 years it was 6 times higher than in adults; however, a wide margin of safety with respect to systemic adverse effects was maintained (see section 4.9). The average time to peak plasma concentration in all age groups was 5 minutes after dosing. The mean plasma half-life was short (<20 minutes) and similar in children and adults, resulting in no accumulation of latanoprost acid in the systemic circulation at steady state.
Special instructions
Special instructions
Latanoprost can gradually change eye color by increasing the amount of brown pigment in the iris. Before starting treatment, patients should be informed about the possible permanent change in eye color. Using the drug in one eye may cause irreversible heterochromia. This change in eye color was predominantly observed in patients with unevenly colored irises, namely: brown-blue, gray-brown, yellow-brown and green-brown. In studies of latanoprost, darkening typically began within the first 8 months of treatment, rarely during the second or third year, and was not observed after four years of treatment. The progression of iris pigmentation decreased over time and stabilized after 5 years. There is no data on increased pigmentation over 5 years. In a 5-year open-label safety study of latanoprost, 33% of patients developed iris pigmentation (see section 4.8). In most cases, the change in iris color was minor and often not clinically detected. The incidence ranged from 7 to 85% in patients with unequally colored irises, predominant in patients with yellow-brown irises. No changes were observed in patients with uniformly colored blue irises; in rare cases, changes were observed in uniformly colored gray, green and brown irises. The change in eye color is caused by an increase in the melanin content in the stromal melanocytes of the iris, and not by an increase in the number of melanocytes themselves. In typical cases, brown pigmentation appears around the pupil and extends concentrically to the periphery of the iris. In this case, the entire iris or parts of it acquire a brown color. After discontinuation of therapy, no further pigmentation was observed. According to available clinical data, the color change was not associated with any symptoms or pathological disorders. The drug has no effect on nevi and lentigines of the iris.
According to the results of 5-year clinical studies, pigment accumulation in the sclero-corneal trabecular meshwork or other parts of the anterior chamber of the eye was not noted. It has been shown that darkening of the iris does not lead to undesirable clinical consequences, so the use of latanaprost can be continued if such darkening occurs. However, such patients should be monitored regularly and, depending on the clinical situation, treatment may be discontinued. Experience with the use of latanoprost in the treatment of angle-closure and congenital glaucoma, pigmentary glaucoma, and open-angle glaucoma in patients with pseudophakia is limited. There is no information on the use of latanoprost in the treatment of secondary glaucoma due to inflammatory eye diseases and neovascular glaucoma.
Latanoprost does not affect pupil size. Due to the lack of experience with the use of latanoprost in the treatment of acute attacks of angle-closure glaucoma, the drug should be used with caution in such patients.
Due to the fact that information on the use of latanoprost in the postoperative period of cataract extraction is limited, caution should be exercised when using the drug in this category of patients. Caution should be exercised when using latanoprost in patients with a history of herpetic keratitis. In acute herpetic keratitis, as well as in the case of anamnestic information about chronic recurrent herpetic keratitis, especially associated with taking prostaglandin F2α analogues, it is necessary to avoid prescribing latanoprost. Macular edema, including cystoid edema, was observed during latanoprost therapy, mainly in patients with aphakia, pseudophakia, rupture of the posterior lens capsule, or in patients with risk factors for the development of cystoid macular edema (in particular, diabetic retinopathy and retinal vein occlusion). Caution should be exercised when using latanoprost in patients with aphakia, pseudophakia with a rupture of the posterior capsule of the lens or anterior chamber intraocular lenses, as well as patients with known risk factors for the development of cystoid macular edema.
Caution should be exercised when using latanoprost in patients with risk factors for developing iritis/uveitis.
Experience with the use of latanoprost in patients with bronchial asthma is limited, but in a number of cases, exacerbation of asthma and/or the appearance of shortness of breath were observed in the post-registration period. Caution should be exercised when using latanoprost in this category of patients (see also section 4.8).
There have been cases of darkening of the skin of the periorbital area, which in a number of patients was reversible with continued therapy with latanoprost. Latanoprost may cause gradual changes in eyelashes and vellus hairs, such as lengthening, thickening, increasing pigmentation, increasing thickness, or changing the direction of eyelash growth. Changes in eyelashes were reversible and disappeared after cessation of therapy.
The product contains benzalkonium chloride, which can cause eye irritation and discolor contact lenses. When using the drug in patients wearing contact lenses, they must be removed before instillation and reinserted no earlier than after 15 minutes. In patients with concomitant corneal diseases and dry eye syndrome, benzalkonium chloride may cause the development of punctate and/or ulcerative keratopathy. Monitoring of the condition of the cornea of such patients during treatment with the drug is required.
Children
Information on the effectiveness and safety of latanoprost in children under one year of age is limited. There is no experience with the use of the drug in premature infants (gestational age less than 36 weeks).
There is no information on the safety of long-term use of latanoprost in children. For primary congenital glaucoma in children aged 0 to 3 years, surgical intervention (goniotomy/trabeculotomy) remains the standard treatment method.
Active ingredient
Active ingredient
Latanoprost
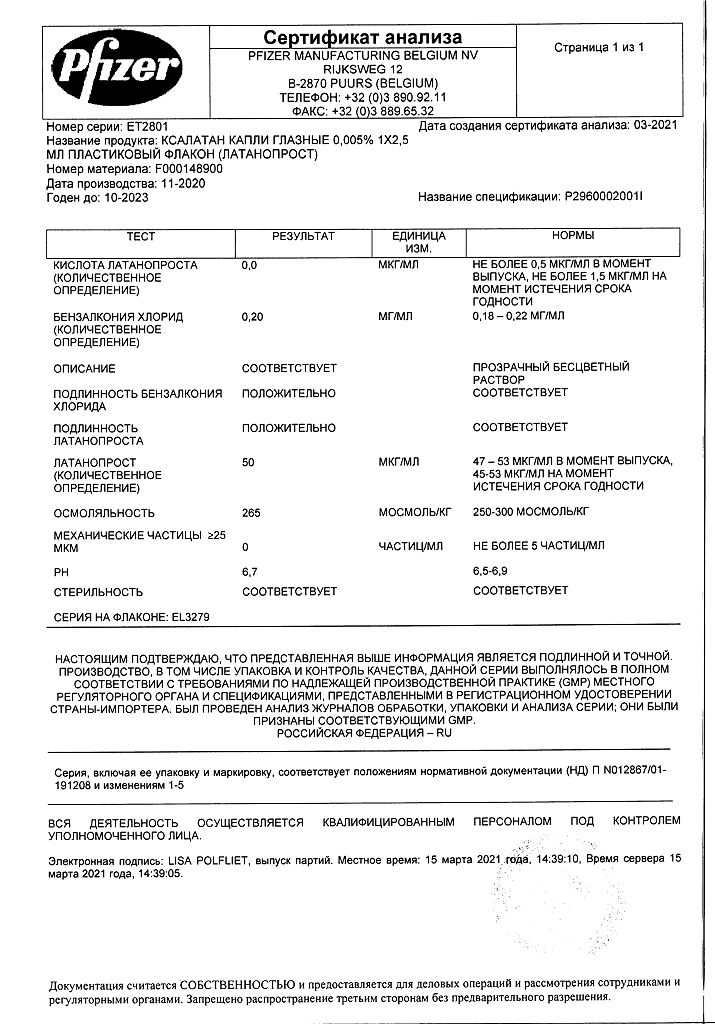
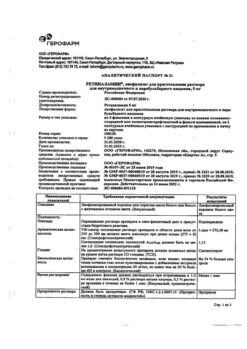
Composition
Composition
Active ingredient: latanoprost
Each 1 ml of solution contains 50 mcg of latanoprost.
List of excipients:
Sodium chloride
Benzalkonium chloride
Sodium dihydrogen phosphate monohydrate
Sodium hydrogen phosphate anhydrous
Water for injection
Pregnancy
Pregnancy
Pregnancy
The safety of latanoprost during pregnancy in humans has not been established. Latanoprost may have toxic effects on pregnancy, the fetus and the newborn. Use during pregnancy is contraindicated.
Lactation
Latanoprost and its metabolites can pass into breast milk. Use during breastfeeding is contraindicated. If it is necessary to use the drug, breastfeeding should be stopped.
Fertility
Latanoprost has not been found to have an effect on male or female fertility in animal studies (see section 5.3).
Contraindications
Contraindications
– Hypersensitivity to the active substance or to any of the excipients listed in section 6.1.
– Age up to 1 year (efficacy and safety have not been established).
Side Effects
Side Effects
Security Profile Summary
Most of the unwanted reactions affect the visual system. In a 5-year open-label safety study of latanoprost, iris pigmentation developed in 33% of patients (see section 4.4). Other adverse reactions from the organ of vision were mostly short-term and occurred during the administration of the drug.
Tabular summary of adverse reactions
The table shows adverse reactions by systemic organ class (SOC) and frequency. The incidence is defined as: very common (≥ 1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), very rare (< 1/10,000) or unknown (cannot be determined from available data). data):
Infections and infestations:
Rarely – Herpetic keratitis
Nervous system disorders:
Uncommon – Headache, dizziness
Visual disorders:
Very common – Hyperpigmentation of the iris; mild moderate conjunctival injection, eye irritation (burning sensation, feeling of sand in the eyes, itching, tingling and foreign body sensation); changes in vellus hair eyelashes (lengthening, thickening, increasing pigmentation and increasing the thickness of eyelashes).
Common: Punctate keratitis, mostly asymptomatic, blepharitis, eye pain, photophobia, conjunctivitis.
Uncommon: Eyelid swelling, dry eyes, keratitis, blurred vision, macular edema, including cystoid macular edema, uveitis.
Rarely – Iritis, corneal edema, corneal erosion, periorbital edema, trichiasis, distichiasis, iris cyst, local skin reaction to
eyelids, darkening of the skin of the eyelids, pseudopemphigoid of the conjunctiva.
Very rare – Changes in the periorbital area and in the eyelid area,
leading to deepening of the eyelid furrow.
Cardiac disorders:
Uncommon – Angina pectoris, palpitations.
Very rare – Unstable angina.
Disorders of the respiratory system, chest and mediastinal organs:
Uncommon – Bronchial asthma, shortness of breath.
Rarely – exacerbation of bronchial asthma.
Skin and subcutaneous tissue disorders:
Uncommon – Rash.
Rarely – Itching.
Muscle, skeletal and connective tissue disorders:
Uncommon – Myalgia, arthralgia.
General disorders and reactions at the injection site:
Uncommon – Chest pain.
Very rare cases of corneal calcification have been reported in some patients with significant corneal damage in association with the use of phosphate eye drops.
Other special populations
Children
In two short-term clinical studies (≤ 12 weeks) involving 93 (25 and 68) pediatric patients, the safety profile was comparable to that in adults; no new adverse events were identified. Short-term safety profiles were also comparable across pediatric populations (see section 5.1). Adverse effects that were observed more often in pediatric patients than in adults: nasopharyngitis and fever.
Reporting suspected adverse reactions
It is important to report suspected adverse reactions after registration of a medicinal product to ensure continuous monitoring of the benefit-risk ratio of the medicinal product. Healthcare professionals are encouraged to report any suspected adverse drug reactions through the national adverse reaction reporting systems of the member states of the Eurasian Economic Union.
Interaction
Interaction
Cases of paradoxical increases in IOP have been reported after simultaneous ophthalmic use of two prostaglandin analogues. Concomitant use of two or more prostaglandins, prostaglandin analogues or prostaglandin derivatives is not recommended.
Pharmaceutically incompatible with eye drops containing thiomersal – precipitation (see section 6.2).
Children
Interaction studies were conducted in adult patients only.
In vitro studies have shown that when eye drops containing thiomersal are mixed with Xalatan, precipitation occurs. When using such medications, eye drops should be instilled at intervals of at least 5 minutes.
Overdose
Overdose
Symptoms
Apart from eye irritation and conjunctival injection, no other ophthalmic effects have been identified following an overdose of Xalatan.
Treatment
In case of accidental ingestion of Xalatan, the following information should be considered:
One vial contains 125 mcg of latanoprost. More than 90% of the dose is metabolized after the first passage through the liver. Intravenous infusion at a dose of 3 mcg/kg in healthy volunteers did not cause any symptoms, but nausea, abdominal pain, dizziness, fatigue, hot flashes and excessive sweating were observed when a dose of 5.5-10 mcg/kg was administered. In monkeys, administration of latanoprost by intravenous infusion in doses up to 500 mcg/kg did not have a significant effect on the cardiovascular system.
In monkeys, intravenous administration of latanoprost was accompanied by temporary bronchospasm. However, in patients with moderate bronchial asthma, administration of latanoprost into the eyes at a dose 7 times higher than the clinical dose of Xalatan did not cause bronchospasm.
In case of overdose with Xalatan, treatment should be symptomatic.
Action
Action
The active substance latanoprost is an analogue of prostaglandin F2, which reduces IOP by increasing the outflow of intraocular fluid. In humans, IOP begins to decrease approximately 3 to 4 hours after administration of the drug; the maximum effect is achieved after 8 – 12 hours. The reduction in IOP lasts for at least 24 hours.
If no improvement is observed while using the drug or you feel a worsening (intensification or appearance of symptoms such as blurred vision, pain in the eyes, burning, stinging, itching, redness of the eyes, sensation of a foreign body in the eye, a feeling of heaviness in the eyes, increased sensitivity to light, the appearance of rainbow circles when looking at bright light, narrowing of the field of vision) you should consult a doctor.
Storage conditions
Storage conditions
Store at a temperature of 2 to 8 °C, protected from light.
Store the opened bottle at a temperature not exceeding 25 °C.
Shelf life
Shelf life
3 years. Use the opened bottle within 4 weeks.
Manufacturer
Manufacturer
USA
Additional information
| Shelf life | Shelf life: 3 years Shelf life: 1 month |
|---|---|
| Conditions of storage | Store at + 2 – + 8 ° C in a light-protected place. |
| Manufacturer | Pfizer, Puerto Rico |
| Medication form | eye drops |
| Brand | Pfizer |
Other forms…
Related products
Buy Xalatan, eye drops 0.005% 2.5ml 3 pcs. with delivery to USA, UK, Europe and over 120 other countries.