No products in the cart.
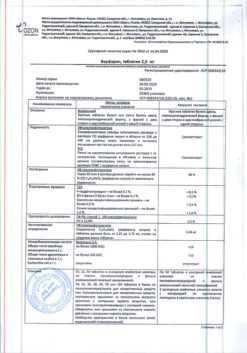
Warfarin-Alium, tablets 2.5mg 100 pcs
€3.26 €2.72
Description
Warfarin s belongs to the group of anticoagulants – drugs that prevent blood clotting, and is intended for long-term use.
It has an indirect anticoagulant effect, inhibiting in the liver the synthesis of a number of factors involved in the regulation of blood clotting.
Warfarex prevents the formation of new blood clots and prevents the increase of already formed ones.
Indications
Indications
Treatment and prevention of thrombosis and embolism of blood vessels: acute venous thrombosis and pulmonary embolism; postoperative thrombosis; repeated myocardial infarction; as an additional agent during surgical or medicinal (thrombolytic) treatment of thrombosis, as well as during electrical cardioversion of atrial fibrillation; recurrent venous thrombosis; repeated pulmonary embolism; prosthetics of heart valves and blood vessels (combination with acetylsalicylic acid is possible); thrombosis of peripheral, coronary and cerebral arteries; secondary prevention of thrombosis and thromboembolism after myocardial infarction and atrial fibrillation.
Pharmacological effect
Pharmacological effect
Warfarin belongs to the group of anticoagulants – drugs that prevent blood clotting, and is intended for long-term use.
It has an indirect anticoagulant effect, inhibiting in the liver the synthesis of a number of factors involved in regulating the blood clotting process.
Warfarex prevents the formation of new blood clots and prevents the expansion of already formed ones.
Special instructions
Special instructions
A prerequisite for warfarin therapy is the patient’s strict adherence to the prescribed dose of the drug.
Patients suffering from alcoholism, as well as patients with dementia, may be unable to adhere to the prescribed warfarin regimen. Conditions such as fever, hyperthyroidism, decompensated heart failure, alcoholism with concomitant liver damage can enhance the effect of warfarin. With hypothyroidism, the effect of warfarin may be reduced. In the case of renal failure or nephrotic syndrome, the level of the free fraction of warfarin in the blood plasma increases, which, depending on concomitant diseases, can lead to either an increase or decrease in the effect. In cases of moderate liver failure, the effect of warfarin is enhanced. In all of the above conditions, careful monitoring of MHO levels should be carried out.
For patients receiving warfarin, paracetamol, tramadol or opiates are recommended for pain relief. If it is necessary to achieve a rapid antithrombotic effect, it is recommended to begin treatment with the administration of heparin; then combination therapy with heparin and warfarin should be administered for 5-7 days until the target IHO level is maintained for 2 days. To avoid coumarin necrosis, patients with hereditary antithrombotic protein C or S deficiency should first be given heparin. The concomitant initial loading dose should not exceed 5 mg. Heparin administration should continue for 5-7 days.
During treatment with warfarin, it is necessary to refrain from drinking ethanol (risk of developing hypoprothrombinemia and bleeding).
In case of individual resistance to warfarin (rare), 5 to 20 loading doses of warfarin are required to achieve a therapeutic effect.
If taking warfarin in such patients is ineffective, other possible reasons should be established, including: concomitant use of warfarin with other drugs (see the corresponding section of the instructions), inadequate diet, laboratory errors.
Treatment of elderly patients should be carried out with special precautions, because the synthesis of coagulation factors and hepatic metabolism in such patients is reduced, as a result of which an excessive effect of warfarin may occur.
Active ingredient
Active ingredient
Warfarin
Composition
Composition
For 1 tablet:
active substance:
warfarin sodium clathrate – 2.71 mg, in terms of warfarin sodium – 2.5 mg;
excipients:
magnesium stearate,
lactose monohydrate,
corn starch,
calcium hydrogen phosphate dihydrate,
povidone K-30.
Contraindications
Contraindications
Hypersensitivity, acute bleeding, severe liver or kidney disease, severe arterial hypertension, acute disseminated intravascular coagulation syndrome, protein C and S deficiency, hemorrhagic diathesis, thrombocytopenia, gastric and duodenal ulcers in the acute stage, cerebral hemorrhage, alcoholism, renal failure, pregnancy, hereditary lactose intolerance, lactase deficiency, glucose-galactose malabsorption.
Side Effects
Side Effects
Most often: >1/10 – bleeding.
Often: >1/100, <1/10 - increased sensitivity to warfarin after long-term use.
Uncommon: >1/1,000, <1/100 - anemia, vomiting, abdominal pain, nausea, diarrhea.
Rarely: >1/10,000, <1/1,000 - eosinophilia, increased activity of liver enzymes, jaundice, rash, urticaria, itching, eczema, skin necrosis, vasculitis, hair loss, nephritis, urolithiasis, tubular necrosis.
Bleeding. The most common risk factor for intracranial hemorrhage. The likelihood of bleeding increases if the INR is significantly higher than the target level. If bleeding begins when the INR is within the target level, there are other underlying conditions that should be investigated.
From the digestive system. Vomiting, nausea, diarrhea.
Necrosis. Coumarin necrosis. In 90% of cases, necrosis develops in women. Lesions are observed from the 3rd to the 10th day of taking the drug and the etiology suggests a deficiency of antithrombotic protein C or S.
Hand-foot syndrome. A very rare complication during warfarin therapy, its development is typical for men with atherosclerotic diseases.
Other. Hypersensitivity reactions manifesting as skin rash and characterized by a reversible increase in liver enzyme concentrations, cholestatic hepatitis, vasculitis, priapism, reversible alopecia and tracheal calcification. Independent risk factors for the development of serious bleeding during treatment with warfarin are: older age, high intensity of concomitant anticoagulant and antiplatelet therapy, a history of strokes and gastrointestinal bleeding. The risk of bleeding is increased in patients with polymorphism of the CYP2C9 gene.
Interaction
Interaction
When used simultaneously with anticoagulants and drugs with antiplatelet activity, the risk of bleeding increases.
When used simultaneously with anticholinergic drugs, memory and attention problems may occur in elderly patients.
When used simultaneously with inhibitors of microsomal liver enzymes, the anticoagulant effect of warfarin is enhanced and the risk of bleeding increases.
When used simultaneously with hypoglycemic agents, sulfonylurea derivatives may enhance their hypoglycemic effect.
With simultaneous use, the anticoagulant effect of warfarin is reduced by: inducers of microsomal liver enzymes (including barbiturates, phenytoin, carbamazepine), glutethimide, griseofulvin, dicloxacillin, coenzyme Q10, mianserin, paracetamol, retinoids, rifampicin, sucralfate, phenazone, cholestyramine, glutethimide, vitamin K, acitretin, diuretics (spironolactone and chlorthalidone), aminoglutethimide, mercaptopurine, mitotane, cisapride, ginseng preparations, glucagon.
It is possible to enhance the anticoagulant effect of warfarin and increase the risk of bleeding when used simultaneously with heparin, NSAIDs (including acetylsalicylic acid), pyrazolone derivatives (including phenylbutazone, sulfinpyrazone), tramadol, dextropropoxyphene, a combination of paracetamol and codeine, antiarrhythmic drugs (in including with amiodarone, quinidine, propafenone, moracizine), antimicrobial and antifungal agents (including with chloramphenicol, metronidazole, cefamandole, cefmetazole, cefoperazone, cefazolin, erythromycin, azithromycin, roxithromycin, clarithromycin, co-trimoxazole, miconazole, ketoconazole, itraconazole, fluconazole, nalidixic acid, ciprofloxacin, norfloxacin, ofloxacin, aminosalicylic acid, benzylpenicillin, doxycycline, isoniazid, neomycin, tetracyclines, aztreonam), glibenclamide, valproic acid, quinine, proguanil, cyclophosphamide, methotrexate, fluorouracil, with combinations of etoposide and vindesine or carboplatin, ifosfamide with mesna, tamoxifen, flutamide, interferon alpha (for chronic hepatitis C), interferon beta, saquinavir, clofibrate, ciprofibrate, fenofibrate, gemfibrozil, cimetidine, lovastatin, fluvastatin, simvastatin, piracetam, danazol, tramadol.
When used simultaneously with tricyclic antidepressants, disopyramide, felbamate, terbinafine, allopurinol, dipyridamole, chloral hydrate, ranitidine, ascorbic acid, and tocopherol, data on drug interactions are ambiguous.
In patients with chronic alcoholism taking disulfiram, an increase in the effects of warfarin was observed.
When used simultaneously with cholestyramine, the absorption and bioavailability of warfarin is reduced.
Cases of liver damage have been reported when used concomitantly with ticlopidine. The anticoagulant effect of warfarin does not change.
When used simultaneously with phenazone, the concentration of warfarin in the blood plasma decreases.
When used concomitantly with phenytoin, an initial increase in anticoagulant activity followed by a decrease has been reported.
When used simultaneously with fluoxetine, trazodone, and vitamin E, there are reports of increased effects of warfarin.
When used simultaneously with cyclosporine, a mutual decrease in effects is observed.
When used simultaneously with enoxacin, the clearance of the R-isomer, but not the S-isomer, decreases, while the prothrombin time does not increase.
When used simultaneously with ethacrynic acid, the diuretic effect and hypokalemia may be enhanced, because as a result of competition for binding to plasma proteins, the concentration of free (active) ethacrynic acid increases.
Regular alcohol consumption may reduce the effects of warfarin, apparently due to the induction of liver enzymes. However, if the liver is damaged, the effects of warfarin may be enhanced.
Accidental ingestion of large amounts of alcohol may increase the effect of warfarin.
Overdose
Overdose
The treatment effectiveness indicator is on the borderline of bleeding development, so the patient may have minor bleeding, for example, microhematuria, bleeding gums, etc. In mild cases, it is enough to reduce the dose of the drug or stop treatment for a short period. For minor bleeding, it is enough to stop taking the drug until the INR reaches the target level.
In case of severe bleeding, administration of vitamin K (intravenously) and activated charcoal, clotting factor concentrate or fresh frozen plasma. If oral anticoagulants are indicated for further use, large doses of vitamin K should be avoided, because Warfarin resistance develops within 2 weeks.
After treatment, long-term monitoring of the patient is necessary, given that the half-life of warfarin is 20-60 hours.
Manufacturer
Manufacturer
Obolenskoye FP JSC, Russia
Additional information
| Manufacturer | Obolenskoe FP JSC, Russia |
|---|---|
| Medication form | pills |
| Brand | Obolenskoe FP JSC |
Other forms…
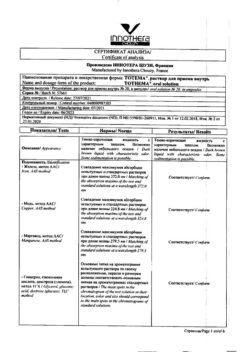
Related products
Buy Warfarin-Alium, tablets 2.5mg 100 pcs with delivery to USA, UK, Europe and over 120 other countries.